Nursing: Family Centered Care
Introduction, the family centered care, reference list.
Family centered care is a practice incorporates the family of a patient to be part of intensive care. The family in this case is the patient’s relatives or people that the patient considers closest to him. Mitchell et al refer to Family Centered Care as [an innovative approach to the planning, delivery, and evaluation of health care that is grounded in mutually beneficial partnerships among health care patients, families, and providers.
Patient and family centered care applies to patients of all ages, and it may be practiced in any health care setting] (Mitchell et al., 2009, 543). Family Centered care therefore is a collaboration of the nurses and the family of the patient to provide intensive care. This collaboration between the family and the nurses results in complete care for the patient. Below is an overview of the Family Centered Care in the Intensive Care Unit.
The patient’s kin play an important role in critical care. They provide information when the patient is unable to speak and make decision for the patients. They are involved in making giving opinions, making, assessing and implementing care. As a result the family centered care benefits the patient. The intensive care “is based on mutual respect, collaboration, and support for the family and the patient” (Mitchell et al 2009, 544).
The family of the patient during intensive care expects that the health providers will notify and assure them of recovery as well as have access to see their relative. Family members who are allowed to assist in giving care ended up with a positive attitude. They assist in giving care even after the patient recovers and is discharged. The patient benefits from the company of the relative. After discharge the patient has an easier time coping with home care given by the relatives, while the relatives cope easily with the giving care.
Furthermore fewer readmission occur (Mitchell et al 2009, 544). According to Gavaghan, family centered care is the key to an all rounded care for intensive care patients. The family receives necessary information in order to support the patient. The nurses on the other hand receive support from the family, while the patient benefits from the intensive care.
In their study, Mitchell et al (2009, 543) observed that there are three indicators of family centered care. They include; respect, collaboration and support. Hennman and Cardin (2002, 65) affirms that the relatives feel respected if they are given information about the patient. The family cares to know the sleeping patterns, the medical procedures the patient is expected to undergo and if the patient is recovering. The family also needs to know when to offer help. This is because they are willing and ready to give support. In this case nurses explain what the family cannot understand, for instance when to let the patient rest. The family needs reassurance. When there is no hope, the family should be informed that the patients comfort is important.
York (2004, 84) found out that health providers have culturally been neglecting the patients family. While the patient is receiving medical attention, the relatives are left in the waiting area without any information. Centrally to that culture, the presence of the kinsmen could have a positive effect. As she further mentions, the family of the patient can alleviate the difficulty of accepting negative results after medical efforts to save life are unsuccessful.
Providing Family centered care is a challenging task. A nurse must practice patience when dealing with the patient and the relatives (Cooley and McAllister, 1999, 121). They should have a positive attitude towards the support to provide intensive care to the patient. Another challenge is the Perceptions about the family. Nurses assume that relatives cause the patient to have stress and therefore time given for visitation is limited.
The nurses see this restriction as a benefit to the patient. This is because they create time for themselves rather than spent a lot of time in the hospital. Nurses should not assume that the presence of a relative on the bedside is an indicator of their inability to work. Also, patients on the other hand should not see the presence of relatives as invasion into their privacy. Instead, they should see it as collective support, to assist them recover. Hennman and Cardin (2002, 64) argue that the important point to consider is to ensure that the patients needs are the determining factor of every action.
In order to ensure that the family centered care is a success there should be some form of regulation. Order can be achieved if there are clearly outlined rules that explain what extend of care the family is allowed to give the patients. There should be a structure that is considerate of the patient, the relatives and the nurses. This will ensure that care is given at the right time, in the right way and by the right person. Information booklets or flyers can be availed to the patient’s relative so that there is understanding amongst them. The importance of this information is to clarify doubts, and states the dos and don’ts. The relatives could be allowed to give feedback in order to improve family centered care (Sisterhen et al., 2007, 319).
Family Centered care contributes to the recovery of a patient through combined efforts. The needs of the patient and the family are met while the nurse gets support in providing care. The patient needs should guide the actions in the family centered care. The end result of this relationship is that the family participates actively in giving support.
Cooley, W. C., & McAllister, J. W. (1999). Putting Family-Centered Care into Practice: A Response to the Adaptive Practice Model . Developmental and Behavioral Pediatrics , 20 (2), 120-122.
Gavaghan, S. R. & Carroll, D. L. (2002). Families of critically ill patients and the effect of nursing interventions. Dimensions in Critical Care Nursing , 21 (2), 64-71.
Henneman, E. A. & Cardin, S. (2002). Family-centered critical care: A practical Approach to making it Happen. Critical Care Nurse , 22 (6), 12-19.
Mitchell, M., Chaboyer, W., Burmeister, E., Foster, M. (2009). Positive Effects of Nursing Intervention on Family- Centered Care in Adult Critical Care. American Journal of Critical Care , 18 (2), 543-552.
Sisterhen, L. L., Blaszak, R. T., Woods, M. B. & Smith, C. E. (2007). Defining family-centered rounds. Teaching and Learning in Medicine , 19 (2), 319-322.
York, N. (2004). Implementing a Family Presence Protocol Option . Dimensions of Critical Care Nursing , 23(2), 84-88.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, April 17). Nursing: Family Centered Care. https://studycorgi.com/nursing-family-centered-care/
"Nursing: Family Centered Care." StudyCorgi , 17 Apr. 2022, studycorgi.com/nursing-family-centered-care/.
StudyCorgi . (2022) 'Nursing: Family Centered Care'. 17 April.
1. StudyCorgi . "Nursing: Family Centered Care." April 17, 2022. https://studycorgi.com/nursing-family-centered-care/.
Bibliography
StudyCorgi . "Nursing: Family Centered Care." April 17, 2022. https://studycorgi.com/nursing-family-centered-care/.
StudyCorgi . 2022. "Nursing: Family Centered Care." April 17, 2022. https://studycorgi.com/nursing-family-centered-care/.
This paper, “Nursing: Family Centered Care”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: July 30, 2022 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.
- Research article
- Open access
- Published: 13 August 2019

Towards a universal model of family centered care: a scoping review
- Kristina M. Kokorelias 1 ,
- Monique A. M. Gignac 2 ,
- Gary Naglie 3 , 4 &
- Jill I. Cameron ORCID: orcid.org/0000-0003-4161-1572 1 , 5
BMC Health Services Research volume 19 , Article number: 564 ( 2019 ) Cite this article
93k Accesses
197 Citations
70 Altmetric
Metrics details
Families play an important role meeting the care needs of individuals who require assistance due to illness and/or disability. Yet, without adequate support their own health and wellbeing can be compromised. The literature highlights the need for a move to family-centered care to improve the well-being of those with illness and/or disability and their family caregivers. The objective of this paper was to explore existing models of family-centered care to determine the key components of existing models and to identify gaps in the literature.
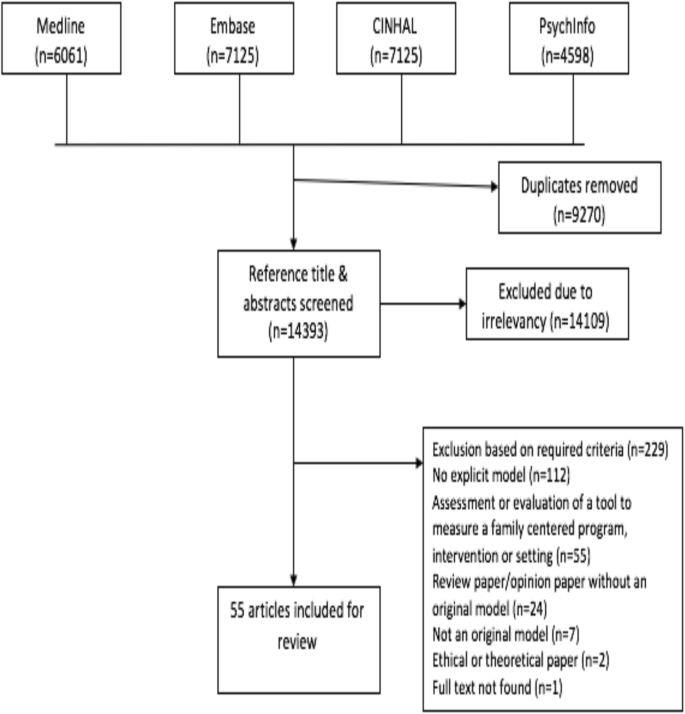
A scoping review guided by Arksey & O’Malley (2005) examined family-centered care models for diverse illness and age populations. We searched MEDLINE, PsycINFO, CINAHL and EMBASE for research published between 1990 to August 1, 2018. Articles describing the development of a family-centered model in any patient population and/or healthcare field or on the development and evaluation of a family-centered service delivery intervention were included.
The search identified 14,393 papers of which 55 met our criteria and were included. Family-centered care models are most commonly available for pediatric patient populations ( n = 40). Across all family-centered care models, the consistent goal is to develop and implement patient care plans within the context of families. Key components to facilitate family-centered care include: 1) collaboration between family members and health care providers, 2) consideration of family contexts, 3) policies and procedures, and 4) patient, family, and health care professional education. Some of these aspects are universal and some of these are illness specific.
Conclusions
The review identified core aspects of family-centred care models (e.g., development of a care plan in the context of families) that can be applied to all populations and care contexts and some aspects that are illness specific (e.g., illness-specific education). This review identified areas in need of further research specifically related to the relationship between care plan decision making and privacy over medical records within models of family centred care. Few studies have evaluated the impact of the various models on patient, family, or health system outcomes. Findings can inform movement towards a universal model of family-centered care for all populations and care contexts.
Peer Review reports
Families play an integral role providing care to individuals with health conditions. As the number of individuals facing chronic illness continues to rise worldwide, there is a timely need to increase recognition of the care input made by family members. Nearly half of Canadians aged 15 years and older have provided care to persons with illness and/or disabilities [ 1 ]. Definitions of caregivers vary, but in general they are an unpaid family member, close friend, or neighbour who provides assistance with every day activities, including hands-on care, care coordination and financial management [ 2 ]. We use the term caregivers to reflect this definition. We use the term family to include the patient, caregiver(s) and other family members. When caring for patients with progressively deteriorating conditions and increasing care needs, over time, caregivers perform more complex care duties similar to those carried out by professional health or social service providers [ 3 , 4 ]. Thus, caregivers play an important role in the care of persons with illnesses or disability across the entire illness trajectory.
Caregiving can be associated with negative outcomes. Caregivers’ physical and mental health, financial status, and social life are often negatively impacted, regardless of the care recipients’ illness [ 2 , 3 , 4 ]. As a result, the quality and sustainability of care provision at home may be threatened [ 5 , 6 ]. Policies and programs to help sustain the caregiving role may reduce the negative consequences of caregiving and optimize care provision in the home.
The need to support caregivers to minimize negative outcomes and optimize the care they provide has received considerable attention in recent policy initiatives. In 2007, the Ontario Ministry of Health and Long-Term Care (MOHLTC) announced the Aging at Home Strategy, “to enable people to continue leading healthy and independent lives in their own homes” [ 7 ]. The strategy implies a shift away from institutional (e.g., long-term care) care towards home care, using population-based funding allocations to offer health and social services to seniors and their caregivers [ 7 ]. This is similar to initiatives in other provinces, such as British Columbia’s Choice in Supports for Independent Living (CSIL) program, introduced in 1994. As these strategies place increasing demands on caregivers, a broader initiative, the National Carer Strategy launched in 2008 and updated in 2014 articulates the need for universal priorities to support caregivers [ 8 ]. Changes in Canada are echoed in other countries, including Sweden and Vietnam [ 9 , 10 , 11 ]. These initiatives aim to facilitate a collaborative action plan to support seniors through policy.
Family-centered care has been proposed to address the needs of not only the patient, but also their family members. To date, family-centered care has been defined by a number of organizations. The Institute for Patient- and Family-Centered Care (IPFCC) [ 12 ] defines family-centered care as mutually beneficial partnerships between health care providers (HCPs), patients, and families in health care planning, delivery, and evaluation. Alternatively, Perrin and colleagues [ 13 ] define family-centered care as an organized system of healthcare, education and social services offered to families, that permits coordinated care across systems. In palliative care, family-centered care is defined by Gilmer [ 14 ] as a seamless continuity in addressing patient, family, and community needs related to terminal conditions through interdisciplinary collaboration. In the broadest scope, the notion of family-centred care embraces the view of the care-client as the patient and their family, rather than just the patient [ 14 ].
Building upon existing definitions, models of family-centered care have been proposed for a number of patient populations. The family-centered approach to healthcare delivery, developed most notably for pediatric-care, values a partnership with family members in addressing the medical and psychosocial health of patients. Parents are considered experts concerning their child’s abilities and needs [ 15 , 16 ]. In the context of critical care, family-centered interventions may decrease the strain of caregiving in families during a crisis [ 17 ]. In the context of stroke, a family-centered approach to rehabilitation showed an improvement in adult children caregivers’ depression and health status one-year post stroke [ 18 ]. Other researchers have argued that family-centered care offers an opportunity to support families and strengthen a working partnership between the patient, family, and health professionals during end of life care [ 19 ]. With an aging population and a growing number of people living with chronic illness, family-centered care can help health care systems to provide support and improve quality-of-life, for patients and their families.
To date, there has been no synthesis of key components of original family-centered care models across all illness populations. Therefore, the objective of this paper was to conduct a scoping review of original models of family-centered care to determine the key model components and to identify aspects that are universal across illness populations, and care contexts and aspects that are illness- or care-context specific. This paper also aimed to identify gaps in the literature to provide recommendations for future research. A scoping review was selected as optimum because its goals are to generate a profile of the key concepts in the existing literature on a topic and identify gaps in the literature [ 20 ].
We used a scoping review methodology guided by Arksey & O’Malley [ 21 ] to gather and summarize the existing literature on family-centred care models.
Search strategy
A literature search of MEDLINE (including ePub ahead of print, in process & other non-indexed citations), CINAHL, PSYCHInfo and EMBASE databases was conducted. The search terms “family-centered”, “family-centred” were applied. The search strategy utilized a narrow focus due to the high degree of noise additional keywords generated. All searches were limited to English language publications from 1990 to August 1, 2018. We did not limit the patient population as we believed that the expected number of models in any sub-set of populations would be low. Searches were conducted by an Information Specialist. EndNote was used to organize the literature and assist with removal of duplicates. See Additional file 1 for an example of the search strategy.
Inclusion and exclusion criteria
Inclusion criteria.
The focus of the article was on the development and/or evaluation of a family-centered model or a family-centered service delivery intervention
The article considered healthcare providers’ communication/interactions with patients and families
The focus of the article was on the development of a family-centered model in any patient population and/or location of care (i.e., acute care hospital, inpatient rehabilitation, community, institutional long-term care).
For the purposes of this paper, we used The Agency for Clinical Innovation (ACI)‘s definition of a model of care: “the way health services are delivered” ([ 22 ], p., 3). The definition includes where, by whom and how the intervention is delivered.
Exclusion criteria
The focus of the article was an assessment or the evaluation of a tool that measured the degree of family-centeredness of a program, intervention or setting and not the evaluation of an original family-centered care model
The article considered only interactions between family members
The article was a review paper that did not propose an original model of family-centered care
The article pertained primarily to ethical issues or the theoretical understandings of family-centered care
The article was focused on training healthcare providers on how to deliver family-centered care and did not offer an original model of family-centered care.
The article reviewed or discussed only the history, implications or rationale for family-centered care (e.g., the study conclusions suggested the need for a model of family-centered care)
The article described a patient-centered care model that only included discussion of family interactions
The focus of the article was on the development of a family-centered model exclusively for social support, rather than in a clinical, health-care context.
Study selection and charting the data
The search identified 14,393 papers. One of the authors (K.M.K.) reviewed the citations and abstracts using the inclusion and exclusion criteria. Two other individuals reviewed 30% of the retrieved abstracts. Any discrepancies were discussed until consensus was reached. The inclusion/exclusion criteria were modified as needed to enhance clarity (final inclusion/exclusion criteria aforementioned). Full-text articles of all potentially relevant references were retrieved, and each was independently assessed for eligibility by one of the authors (K.M.K.) and the two other reviewers. There was 100% concordance between all reviewers on this second step. Reference lists of the included articles were reviewed by one of the authors (K.M.K.) and the two other reviewers, but no additional articles were added to the review.
Data were extracted by the lead author (K.M.K.) and the abstracted data content was reviewed for accuracy by the two other reviewers. Data were extracted relating to elements of the family-centered care model including details of the targeted population, objectives, intervention (if applicable), key findings and desired outcomes of the model. The key components of the models were systematically charted using a data charting form developed in Microsoft Word with a priori categories to guide the data extraction (see Additional file 2 ).
Data synthesis
The purpose of this scoping review was to aggregate the family-centred model descriptions and present an overview of the key elements of the models. Methodological rigour of the publications was not examined, as consistent with scoping review methodologies [ 21 ].
The extracted data were collated to identify key components of models of family-centered care. K.M.K extracted the data and J.I.C reviewed the extracted data. K.M.K and J.I.C then followed qualitative thematic analysis using techniques of scrutinizing, charting and sorting the extracted data according to crucial nuances of the data, and this was summarized into descriptive themes characterizing model components [ 21 , 23 ]. Data were synthesized using summary tables with tentative thematic headings. Themes and potential components of family-centered care models were discussed between K.M.K and J.I.C until consensus was achieved, and final themes were developed. When discussing themes, K.M.K and J.I.C analyzed the data within and then across different patient populations (diagnoses), age groups (pediatric vs. adult literature), and care contexts (e.g., acute care, community care) to identify aspects of models that are universal (i.e., do not differ across populations and care contexts) and aspects that are illness-specific. Final themes were then discussed with all authors. These themes represent answers to our study objective.
Fifty-five articles were included in this review (see Fig. 1 ). The majority of articles were not grounded in empirical research but proposed models for family-centered care and offered practical suggestions to inform implementation (91%). Of the 9 empirical studies, four articles (7%) described randomized control trials (RCTs) and one (2%) described a pre-test, post-test evaluation of their model. Three of the models tested in RCTs were developed to support families at the end of the patients’ lives, with the other model focused on behavioural change as part of childhood obesity treatment. The article describing a pre-test, post-test evaluation aimed to reduce alcohol and drug use through positive peer and family influences. Another study used longitudinal experimental quantitative design to measure the impact of their family-centered care model over two time points, using t-test analysis [ 24 ]. These studies demonstrated benefits of the models including enhanced feelings of mastery and empowerment for family members in care planning through skill building [ 24 , 25 , 26 ].
Search Selection
Two articles (3%) examined the feasibility of applying the concepts of family-centered models into practice. Eight articles (14%) described case studies of an implemented model that included families and children with complex medical needs in palliative and sub-acute settings with conditions including HIV, cancer and stem-cell transplantations. Another described patients and families in cardiac intensive care units (CICU) after operative procedures. Nine (16%) articles were literature reviews on FCC that lead to the description of a single hypothetical family-centered care model, but did not review all existing FCC models. One article (2%) compared HCPs’ roles in traditional models of care with their roles the family-centered model.
Out of the 55 included papers, 40 (73%) were explicitly designed for pediatric care recipients. In the pediatric literature, family-centered care models were proposed for a variety of populations which included, but were not limited to, cancer ( n = 5), AIDS/HIV ( n = 3), motor dysfunction (e.g. cerebral palsy) ( n = 3), non-illness specific disabilities ( n = 2), obesity ( n = 3), asthma ( n = 1), oral disease (1 paper), trauma ( n = 2), autism ( n = 1) and transplant recipients ( n = 1). Eighteen studies did not report on a specific population. In adult populations, models have been presented for palliative care ( n = 3), heart failure ( n = 1), mental health ( n = 1), cancer ( n = 1), age-related chronic conditions ( n = 1) and unspecified populations ( n = 8).
Many of the family-centered care models have been developed for a variety of care contexts (e.g., community, acute care) and incorporate a variety of health care professionals. Care contexts included home/community care, acute hospital wards, emergency departments, critical care units, inpatient rehabilitation units and palliative care units. Professionals identified in the models primarily included nurses, social workers, physicians and nutritionists. In some models, psychologists, rehabilitation therapists and chaplains also were included. The core elements of FCC models did not differ by diagnosis, age or care context. This suggested that some aspects of FCC models were universal. We use the term “universal” to refer to this notion of high-level concepts that can be applied across illness populations, ages and care contexts. Universal and illness-specific aspects of FCC will be discussed in detail below.
Thematic analysis revealed a universal goal of FCC models to develop and implement patient care plans within the context of families. To facilitate this aim, family-centered care models require: 1) collaboration between family members and health care providers, 2) consideration of family contexts, 3) education for patients, families, and HCPs, and 4) dedicated policies and procedures. Figure 2 provides a graphical overview of the key components of FCC. This figure highlights the overarching goal of FCC models and the key components required to help facilitate this goal including both universal and illness-specific components.

Universal Model of Family-Centered Care
Overarching theme: family-centred care plan development and implementation
This overarching theme describes the universal goal of family-centered care models to develop and implement patient care plans that are created within the context of unique family situations.
All 55 models supported the development of family-centered care plans with specific short and long-term outcomes [ 27 , 28 , 29 ]. Patients, families and HCPs were considered key partners who should contribute to the clarification of care plan goals [ 30 , 31 , 32 , 33 ]. Care plans should consider the day-to-day ways of living for patients and families [ 34 , 35 , 36 , 37 , 38 , 39 , 40 ] by encouraging the maintenance of home routines [ 41 ]. Potential goals identified included achieving family and patient identified functional milestones like a new motor skill (e.g., running) [ 30 ]; decreasing delays or complications at hospital discharge [ 42 ]; improving patient and family satisfaction with care [ 40 , 41 , 42 ]; and improving caregiver support [ 43 ]. Patient involvement in care plans was acknowledged as conditional upon the patient’s capacity to participate (it may exclude young children, people with illnesses affecting their cognition, etc.). From the initial diagnosis, the models championed that all members of the patients care team should elicit families’ perspectives regarding priorities, families’ needs and concerns, and their abilities to provide care [ 14 , 29 , 37 , 44 , 45 , 46 , 47 , 48 ]. Understanding families’ needs and priorities was deemed important and as contributing to realistic and better-defined outcomes [ 24 , 45 ], as well as important to enhance families’ abilities to support the plan and optimize patient outcomes [ 41 , 49 , 50 , 51 ].
The models also emphasized that HCPs and family members should share in the implementation of the care plan. Care delivery should commence when everyone is in agreement with the care plan [ 42 ]. It was noted that family members should be encouraged to communicate any issues or priorities they have regarding care to HCPs [ 27 , 44 ]. Family members of relatives who are inpatients also should be involved in discharge planning, such as describing their concerns and ability to perform care duties [ 42 ] so as to troubleshoot and optimize care in the community. Some models noted that care plans can be made achievable by breaking them down into smaller steps for the family [ 27 ]. One model also hypothesized that monitoring the success of the care plan has the potential to optimize service use by bridging service gaps and eliminating any duplication of resources [ 52 ].
Model components
In addition to the overarching theme related to care plan development and implementation (described above), other key model components needed to facilitate family-centered care plans were identified. These encompassed collaboration and communication; education and support; consideration of the family context; and the need for policies and procedures.
Collaboration
Family-centered care models highlighted collaboration between HCPs, patients and families as key in the development of care plans. Collaboration was noted as being required across the illness and care trajectory [ 53 ] to enhance patients’ and families’ abilities to maintain control over the patient’s care plan and delivery [ 54 ], particularly as care becomes increasingly complex [ 55 ].
Many of the family-centered care models offered some insight into how families and HCPs could work together in the delivery of care across the care trajectory. Trusting [ 54 ], caring and collaborative relationships [ 44 ] between families and HCPs were identified as key and efforts should be undertaken to cultivate them. In this collaborative relationship, HCPs were encouraged to relinquish their role as a single authority. Some authors even argued that families should have decision-making authority to decide upon the role and the degree of involvement of HCPs in developing care plans [ 28 ]. Attharos and colleagues [ 55 ] further suggested that family-centered care models should have defined roles for each family member, the patient, and all involved HCPs. All roles are essential to the development of care plans [ 56 ].
Communication
Family-centered care models were thought to better facilitate communication and exchange of information and insights among family members, patients and HCPs related to the development and delivery of care plans [ 54 ]. One model suggested that clinicians should offer care options and patients and families should advocate for patient preferences and family values [ 57 ]. The exchange of information was encouraged to be open, timely, complete and objective [ 27 , 55 ].
The models encouraged HCPs to use a variety of strategies to communicate with and support caregivers and patients, including interdisciplinary care and diagnostic reports, community follow-up in-person or by virtual meetings, and resource notebooks listing community supports to help care for the patient [ 29 ]. HCPs were also encouraged to communicate disease-specific information to help patients and family members make appropriately-informed disease-related decisions [ 32 , 39 , 57 ].
Education about care provision and the disease was deemed necessary to enable family-centered care. Education was typically approached from the concept of mutual learning, whereby patients, family members and HCPs all learn and support each other [ 38 , 54 ]. In general, models advocated for training of HCPs to effectively elicit information and communicate with patients and family members. This was thought to decrease anxiety and increase control for patients and caregivers [ 14 , 32 , 58 , 59 ].
Various researchers posited ways to best provide education about the illness and care provision to patients and families. Connor [ 60 ] suggested that written information, describing the family-centered approach to care should be provided to patients and caregivers. Further, all information should be presented at a language level that is understandable to the family and patient [ 42 , 43 , 60 ], which means minimizing technical (e.g., medical) jargon [ 59 ].
Education was though to be ongoing, meaning that it often doesn’t end when a patient is discharged from an inpatient setting. Models highlighted a need to establish methods to continue educating caregivers beyond inpatient care [ 49 ], such as by providing the patient and family with a follow–up care plan after discharge and possibly follow-up contact by HCPs [ 33 ]. Appropriately communicated education is believed to foster a sense of trust [ 42 ] and help patients and family members become more knowledgeable. As a result, patients and families were thought to become more independent in making informed treatment decisions [ 14 , 35 , 37 ].
Some models noted that patients and their family members find it helpful to learn from other patients and caregiver peers [ 32 ]. Peer sharing of mutually supportive resources and other experiences related to living with an illness or providing care can serve as an important means of improving knowledge about support resources [ 32 ] and enhancing emotional support [ 60 , 61 ]. This was thought to be possible as part of family centered care models by care teams helping to cultivate friendships and general peer support with other families in similar caregiving situations (for example, those caring for care recipients with the same illness). Other mechanisms to offer peer support could include patient and caregiver support groups, workshops, group retreat trips, and shared respite care [ 14 ].
Family support needs
Family members may experience a negative impact on their own well-being as part of the ongoing demands of caregiving. Recognizing that families are often psychologically stressed and can have difficulties coping [ 59 ], family-centered care models emphasized support for family members’ well-being [ 62 ]. Supporting families often included emotional support and providing education and training on care delivery that takes into account caregiver needs and preferences. Family-centered models acknowledge that caregivers are experts in matters concerned with their own well-being [ 47 ]. HCPs were thought to support caregivers’ by providing education to foster caregivers’ confidence in their ability to provide care and develop care plans.
Family-centered care models emphasized that care recipients function best in a supportive family environment [ 41 ]. Identifying the impact of the illness on the patient and the family is crucial to providing emotional support [ 42 ]. At a minimum, information about support needs should be gathered from both patient and family [ 63 ]. Particularly in pediatric patient populations, authors spoke of identifying types of support that are based on the patient’s developmental capacities [ 64 ] and needs, while also taking into consideration the social context of the patient and family’s life [ 48 ]. Support needs can be determined through well-designed, semi-structured activities, including questionnaires [ 48 ] and discussions with the family.
Health systems utilizing a family-centered care model were thought to help sustain caregivers by providing them with resources to support their caregiving activities [ 65 ]. Goetz and Caron [ 49 ] state that organizational support should make existing health service community resources more family-centered by considering the family in all aspects of program delivery. Topics that need to be addressed by services offered to family members included, mental health, home care, insurance/financing, transportation, public health, housing, vocational services, education and social services [ 13 ].
Consideration of family context
Family was conceptualized in different ways across models. For example, some models described including the family-as-a-whole (every family member, not just those that provide care) [ 63 , 64 ], whereas others described the family as those who provide care [ 44 ]. Authors highlighted that families have ‘the ultimate responsibility’ [ 63 ] and should have a constant presence throughout the care and illness trajectory [ 60 ]. Consistently across family-centered care models, families were seen as vital members of the care team [ 38 ] who provide emotional, physical, and instrumental levels of support to the patient [ 32 , 54 ].
Family strengths
Three of the models underscored that family-centered care is based on a belief that all families have unique strengths that should be identified, enhanced, and utilized [ 41 , 53 , 66 ]. Models identified various examples of family strengths in care delivery including resilience [ 41 ], coping strategies [ 58 ], competence and skill in providing care [ 25 , 26 ] and motivation [ 49 ]. None of the models discussed how these strengths would be identified when implementing family centered care. Three of the models stated that family-centered care should continuously encourage caregivers to utilize these strengths [ 53 , 57 , 64 ] although specific examples of how to do so were not included. Identifying areas of weakness that may require education and training was not discussed in the models.
Cultural values
Families were thought to contribute to a culturally sensitive care plan by discussing their specific cultural needs, as well as their strengths related to personal values, preferences and ideas. Caregivers’ social, religious, and/or cultural backgrounds can influence the provision of care to their family member [ 29 , 49 , 57 , 58 ]. One model suggested that HCPs need to elicit information about families’ beliefs [ 26 ] to help guide culturally sensitive care plans (e.g. religious participation). The process by which this would occur was not discussed in detail.
Dedicated policies and procedures to support implementation
To support implementation, family-centered care models should have dedicated policies and procedures that are also transparent [ 56 , 67 , 68 ]. Both the macro and micro levels of society need to be considered when trying to implement family-centered practices [ 13 ]. Perrin and colleagues [ 13 ] described macro level issues as including government policies and agencies (e.g., national, provincial, municipal), while micro level factors include community service systems (e.g., physicians, other HCPs, schools, public transportation, etc.). Examples of macro-level considerations include incorporating families in nation-wide policy making and program development [ 29 , 53 , 56 , 60 ]. Micro-level considerations include incorporating family members and patients in decision-making for local community organizations [ 69 ], the implementation of health programs and care policies at regional hospitals, as well as in HCP education [ 29 ].
Family-centered care policies were identified as important as they legitimize and support families’ contributions to the care of their family member. For example, in pediatrics, Regan and colleagues [ 39 ] suggested changing policy to open visitation hours to increase family members’ roles as partners in care. This could increase the number of interactions between HCPs, patients and families, and, as a result, further support caregivers in their caring role [ 24 ].
Family-centered care models also noted the importance of considering the physical environment when developing policies and practices. The physical environment of care settings should be created and tailored to meet the needs of patients and families [ 54 ], although concreate examples were not provided. Both the patient and family should be included in the development and evaluation of facility design [ 29 ], where possible, as well as modifications to the home environment.
The purpose of this scoping review was to identify core components of family-centered care models and to identify components that are universal and can be applied across care populations. This paper also aimed to identify gaps in the literature to provide recommendations for future research. Most models were developed for pediatric populations with a number of models emerging for the care of adult populations. The synthesis suggests that there are core components of family-centered care models that were not unique to specific illness populations or care contexts making them applicable across diverse health conditions and experiences. From a theoretical perspective, our review adds to our understanding of how FCC is conceptualized within the current state of the literature and suggests the possibility of moving towards a universal model of FCC. This includes developing a care plan with defined outcomes and that incorporates patient and family perspectives and their unique characteristics. This also includes collaboration between HCPs and family members and flexible policies and procedures. However, there were some aspects of models that were specific to illness populations such as illness-specific patient and family education.
Currently, person-centered care is considered best practice for improving care and outcomes for many illness populations. Patient-centered care has been described as being “respectful of and responsive to individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions” [ 70 ]. Person-centered care involves: acknowledging the individuality of persons in all aspects of care, and personalizing care and surroundings; offering shared decision making; interpreting behavior from the person’s viewpoint; and prioritizing relationships to the same extent as care tasks [ 71 ]. Aspects of patient and person-centered care were identified as key components of family-centered care models including focusing on patient and family values, preferences and needs, related to their own circumstances and family contexts. In addition, this review identified specific components that go beyond patient-centered care that are required to address the needs of families including focusing on respectful communication to facilitate the necessary patient/family-professional partnerships and collaboration needed to develop and implement care plans. Moreover, there is the need for the patient/family-professional partnerships to respect the strengths, cultures and expertise that all members of this partnership bring to the development and delivery of care plans.
Implementation of illness-specific models of care for multiple different illnesses may be challenging for health care systems. As many individuals live with multi-morbidity, a non-illness specific family-centered care model may meet the needs of more individuals [ 72 ]. Yet, there is a lack of discussion in the literature of concrete strategies to help implement the key concepts identified in our review. Moreover, the research on implementing FCC models in real world situations is scant. In order to encourage changes in health care systems there is a need for evidence that the concepts of FCC lead to improvements.
This review identified aspects of family-centered care that are illness-specific. Illness-specific education and support is required at each stage of the illness recognizing differences in illness trajectories across patient populations [ 73 ]. Currently, the models are described with static concepts that are not reflective of ongoing and changing illness trajectories. Providing illness-specific care, advice, and information that is sensitive to their place in the illness trajectory may greatly influence caregivers’ capacity to support the care recipient. Further research is needed to understand how family-centered care may evolve across the illness and care trajectory.
More research is needed to enhance the potential of a universal family-centered care model that crosses age groups, conditions, and care settings. For instance, in the current models of FCC, there is not consistent definition of what constitutes the family. In the pediatric literature the family primarily includes the parents of the child, but does not usually include siblings or extended family members who may be providing care. Moreover, current FCC models fail to address conflict and mediation for circumstances where there is the potential for family members to disagree with one another, with the patient or with the HCPs regarding care plans or other aspects of care.
As many of the models were developed for pediatric populations, they fail to acknowledge aspects such as privacy issues and cognitive capacity. These issues become relevant as we consider models of care for adult populations. In instances where patients’ cognitive capacity influences their ability to participate in decision-making, family caregivers become active contributors to care plan development and implementation. Caregivers can benefit from having access to patients’ medical information to contribute to treatment decision making and inform care and service use. Current privacy legislation does not automatically give families access to relevant information. Future research should explore adult patients’ preferences for family members to have access to their medical records, as their preferences will influence the management of privacy in models of FCC.
Lastly, the articles included in this review were primarily descriptive and not evaluative. Evaluations are needed to demonstrate the benefit of FCC to patient, caregiver and health system outcomes. Potential evaluation outcomes can include satisfaction with care, improvements in patient health and caregiver health and stress, and efficient use of health services. There should be consensus regarding outcome measures to be used when evaluating FCC models to enhance our ability to compare across models. Model evaluation is needed to provide empirical evidence to support or reject the concepts of FCC in both universal and illness-specific contexts. Moreover, we need methods to assess implementation of FCC in practice. For example, measures to assess the family-centered nature of care are being developed [ 24 , 25 , 26 ]. The review suggests we may need new assessment tools to assess, for example, family strengths.
Concrete steps are needed to implement a universal FCC care model into practice. While we have defined the components of a model, we have also highlighted additional empirical research that is needed to further define model components in real-world settings, within and across various care contexts and illness populations. In particular, we recommend the testing of our universal model in the context of a randomized control trial (RCT).
Lastly, we recommend the development of outcomes measures to determine if FCC leads to improvements in patient and family satisfaction, mental and physical health outcomes, enhanced efficiency, health system utilization (e.g., decreased length of hospital stay or return hospital visits), community reintegration and cost-effectiveness. Important outcomes should relate to families, patients of all ages and health care professionals. Outcome measures related to health care professionals may include enhanced comfort working with families and patients. Valid and reliable measures are essential for the evaluation of a model’s effectiveness and to translate FCC models into practice.
Study limitations
This scoping review is not without limitations. Only published, English language articles were included, thus excluding other models that may exist in other languages. This may have also limited models to those that were developed and/or tested in predominantly English-speaking counties. We also did not explore grey literature, limiting our models to only those that underwent peer review. Many of the included models were designed for the pediatric population, so findings have limited application to adult populations.
This paper used an established scoping review methodology to synthesize 55 models of family-centered care. We were able to determine the universal components of the models that place both the patient and family at the center of care, regardless of the patient’s illness or care context. Findings outline aspects of FCC that are universal and aspects that are illness specific. Universal aspects include collaboration between family members and health care providers to define care plans that take into consideration the family contexts. It also includes the need for flexible policies and procedures and the need for patient, family, and health care professional education. Non-universal aspects include illness-specific patient and family education. Future research should evaluate the ability of FCC to improve important patient, family, caregiver, and health system outcomes. Health care policies and procedures are needed that incorporate FCC to create system level change. Our review moves the field of FCC forward by identifying the universal and illness-specific model components that can inform model development, testing, and implementation. Advancing FCC has the potential to optimize outcomes for patients, families, and caregivers.
Availability of data and materials
Not applicable.
Abbreviations
Family-centered care
Health care professionals
Sinha M. Portrait of caregivers, 2012. Ottawa: Statistics Canada; 2013. Retrieved from: http://healthcareathome.ca/mh/en/Documents/Portrait%20of%20Caregivers%202012.pdf
Google Scholar
Brodaty H, Donkin M. Family caregivers of people with dementia. Dialogues Clin Neurosci. 2009;11(2):217.
PubMed PubMed Central Google Scholar
Schulz R, Martire LM. Family caregiving of persons with dementia: prevalence, health effects, and support strategies. Am J Geriatr Psychiatry. 2004;12(3):240–9.
Article PubMed Google Scholar
Collins LG, Swartz K. Caregiver care. Am Fam Physician. 2011;83(11):1309.
PubMed Google Scholar
Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. The Gerontologist. 1980;20(6):649–55.
Article CAS PubMed Google Scholar
Government of Canada. Canada Health Act [“CHA”], R.S.C. 1985, c. C-6. Ottawa, Retrieved from https://web.archive.org/web/20031205153216/http://laws.justice.gc.ca/en/C-6/
Ministry of Health and Long-Term Care. Ontario's Aging at Home Strategy. Toronto: Ministry of Health and Long-Term Care; 2007. Retrieved from: http://www.health.gov.on.ca/english/public/ program/ltc/33_ontario_strategy.html
Carers Canada. Canada’s Carer strategy. Ottawa. Retrieved from: http://www.carerscanada.ca/wp-content/uploads/2017/01/CC-Caregiver-Strategy_v4.pdf .
Feinberg LF, Newman SL. A study of 10 states since passage of the National Family Caregiver Support Program: policies, perceptions, and program development. The Gerontologist. 2004;44(6):760–9.
Hokenstad MC Jr, Restorick RA. International policy on ageing and older persons: implications for social work practice. Int Soc Work. 2011;54(3):330–43.
Article Google Scholar
Sweden Report, Supra note 20, sat 9; social services act, SFS 2001:453, promulgated June 7, 2001, online: Ministry of Health and Social Affairs, Sweden.
Institute for Patient- and Family-Centered Care. What is patient- and family-centered care? Available at: http://www.ipfcc.org/about/pfcc.html
Perrin JM, Romm D, Bloom SR, Homer CJ, Kuhlthau KA, Cooley C, Duncan P, Roberts R, Sloyer P, Wells N, Newacheck P. A family-centered, community-based system of services for children and youth with special health care needs. Arch Pediatr Adolesc Med. 2007;161(10):933–6.
Gilmer MJ. Pediatric palliative care. Crit Care Nurs Clin North Am. 2002;14(2):207–14.
MacKean G, Spragins W, L’Heureux L, Popp J, Wilkes C, Lipton H. Advancing family-centred care in child and adolescent mental health. A critical review of the literature. Healthc Q. 2012;15:64–75.
Chu S, Reynolds F. Occupational therapy for children with attention deficit hyperactivity disorder (ADHD), part 2: a multicentre evaluation of an assessment and treatment package. Br J Occup Ther. 2007;70(10):439–48.
Johnson SK, Craft M, Titler M, Halm M, Kleiber C, Montgomery LA, Megivern K, Nicholson A, Buckwalter K. Perceived changes in adult family members' roles and responsibilities during critical illness. J Nurs Scholarsh. 1995;27(3):238–43.
Article CAS Google Scholar
Visser-Meily A, Post M, Gorter JW, Berlekom SB, Van Den Bos T, Lindeman E. Rehabilitation of stroke patients needs a family-centred approach. Disabil Rehabil. 2006;28(24):1557–61.
Teno JM, Casey VA, Welch LC, Edgman-Levitan S. Patient-focused, family-centered end-of-life medical care: views of the guidelines and bereaved family members. J Pain Symptom Manag. 2001;22(3):738–51.
Gagliardi AR, Berta W, Kothari A, Boyko J, Urquhart R. Integrated knowledge translation (IKT) in health care: a scoping review. Implement Sci. 2015;11(1):38.
Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
The Agency for Clinical Innovation (ACI). Understanding the process to develop a Model of Care: An ACI Framework. A practical guide on how to develop a Model of Care . 2013 May [cited 2018 April 27]. Available from: https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0009/181935/HS13-034_Framework-DevelopMoC_D7.pdf
Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69.
Article PubMed PubMed Central Google Scholar
Marcenko MO, Smith LK. The impact of a Fmaily-centered case management approach. Soc Work Health Care. 1992;17(1):87–100.
Kissane D. Family focused grief therapy: the role of the family in preventive and therapeutic bereavement care. Bereave Care. 2003;22(1):6–8.
Kissane D, Lichtenthal WG, Zaider T. Family care before and after bereavement. Omega. 2008;56(1):21–32.
Leviton A, Mueller M, Kauffman C. The family-centered consultation model: practical applications for professionals. Infants Young Child. 1992;4(3):1–8.
Sharifah WW, Nur HH, Ruzita AT, Roslee R, Reilly JJ. The Malaysian childhood obesity treatment trial (MASCOT). Malays J Nutr. 2011;17(2):229–36.
CAS PubMed Google Scholar
Jasovsky DA, Morrow MR, Clementi PS, Hindle PA. Theories in action and how nursing practice changed. Nurs Sci Q. 2010 Jan;23(1):29–38.
Darrah J, Law M, Pollock N. Family-centered functional therapy-a choice for children with motor dysfunction. Infants Young Child. 2001;13(4):79–87.
Dowling J, Vender J, Guilianelli S, Wang B. A model of family-centered care and satisfaction predictors: the critical care family assistance program. Chest. 2005;128(3):81S–92S.
Madigan CK, Donaghue DD, Carpenter EV. Development of a family liaison model during operative procedures. MCN Am J Matern Child Nurs. 1999;24(4):185–9.
Sisterhen LL, Blaszak RT, Woods MB, Smith CE. Defining family-centered rounds. Teach Learn Med. 2007;19(3):319–22.
Hyman D. Reorganizing health systems to promote best practice medical care, patient self-management, and family-centered care for childhood asthma. Ethnicity & disease. 2003;13(3 Suppl 3):S3–94.
Kaufman J. Case management services for children with special health care needs. A family-centered approach. J Case Manag. 1992;1(2):53–6.
Prelock PA, Beatson J, Contompasis SH, Bishop KK. A model for family-centered interdisciplinary practice in the community. Top Lang Disord. 1999;19(3):36–51.
Cormany EE. Family-centered service coordination: a four-tier model. Infants Young Child. 1993;6(2):12–9.
King G, Tucker MA, Baldwin P, Lowry K, Laporta J, Martens L. A life needs model of pediatric service delivery: services to support community participation and quality of life for children and youth with disabilities. Phys Occup Ther Pediatr. 2002;22(2):53–77.
Regan KM, Curtin C, Vorderer L. Paradigm shifts in inpatient psychiatric care of children: approaching child-and family-centered care. J Child Adolesc Psychiatr Nurs. 2006;19(1):29–40.
McKlindon D, Barnsteiner JH. Therapeutic relationships: evolution of the Children's Hospital of Philadelphia model. MCN Am J Matern Child Nurs. 1999;24(5):237–43.
Romero-Daza N, Ruth A, Denis-Luque M, Luque JS. An alternative model for the provision of services to hiV-positive orphans in Haiti. J Health Care Poor Underserved. 2009;20(4):36–40.
Muething SE, Kotagal UR, Schoettker PJ, del Rey JG, DeWitt TG. Family-centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119(4):829–32.
Raina P, O'Donnell M, Rosenbaum P, Brehaut J, Walter SD, Russell D, Swinton M, Zhu B, Wood E. The health and well-being of caregivers of children with cerebral palsy. Pediatrics. 2005;115(6):e626–36.
Hernandez LP, Lucero E. Days La Familia community drug and alcohol prevention program: family-centered model for working with inner-city Hispanic families. J Prim Prev. 1996;16(3):255–72.
MacFarlane MM. Family centered care in adult mental health: developing a collaborative interagency practice. J Fam Psychother. 2011;22(1):56–73.
Mausner S. Families helping families: an innovative approach to the provision of respite care for families of children with complex medical needs. Soc Work Health Care. 1995;21(1):95–106.
Biggert RA, Watkins JL, Cook SE. Home infusion service delivery system model: a conceptual framework for family-centered care in pediatric home care delivery. J Intraven Nurs. 1992;15(4):210–8.
Prizant BM, Wetherby AM, Rubin E, Laurent AC. The SCERTS model: a transactional, family-centered approach to enhancing communication and socioemotional abilities of children with autism spectrum disorder. Infants Young Child. 2003;16(4):296–316.
Goetz DR, Caron W. A biopsychosocial model for youth obesity: consideration of an ecosystemic collaboration. Int J Obes. 1999;23(S2):S58.
Byers JF. Holistic acute care units: partnerships to meet the needs of the chronically I11 and their families. AACN Adv Crit Care. 1997;8(2):271–9.
CAS Google Scholar
Law M, Darrah J, Pollock N, King G, Rosenbaum P, Russell D, Palisano R, Harris S, Armstrong R, Watt J. Family-centred functional therapy for children with cerebral palsy: an emerging practice model. Phys Occup Ther Pediatr. 1998;18(1):83–102.
Brady MT, Crim L, Caldwell L, Koranyi K. Family-centered care: a paradigm for care of the HIV-affected family. Pediatr AIDS HIV Infect. 1996;7(3):168–75.
Tyler DO, Horner SD. Family-centered collaborative negotiation: a model for facilitating behavior change in primary care. J Am Assoc Nurse Pract. 2008;20(4):194–203.
Brown K, Mace SE, Dietrich AM, Knazik S, Schamban NE. Patient and family–centred care for pediatric patients in the emergency department. CJEM. 2008;10(1):38–43.
Attharos T. Development of a family-centered care model for the children with cancer in a pediatric cancer unit. Thailand: Mahidol University; 2003.
Baker JN, Barfield R, Hinds PS, Kane JR. A process to facilitate decision making in pediatric stem cell transplantation: the individualized care planning and coordination model. Biol Blood Marrow Transplant. 2007;13(3):245–54.
Lyon ME, Garvie PA, Briggs L, He J, McCarter R, D'Angelo LJ. Development, feasibility, and acceptability of the family/adolescent-centered (FACE) advance care planning intervention for adolescents with HIV. J Palliat Med. 2009;12(4):363–72.
Beers LS, Cheng TL. When a teen has a tot: a model of care for the adolescent parent and her child: you can mitigate the health and educational risks faced by an adolescent parent and her child by providing a medical home for both. This" teen-tot" model of family-centered care provides a framework for success. Contemp Pediatr. 2006;23(4):47–52.
Callahan HE. Families dealing with advanced heart failure: a challenge and an opportunity. Crit Care Nurs Q. 2003;26(3):230–43.
Connor D. Family-centred care in practice. Nurs N Z. 1998;4(4):18.
Martin-Arafeh JM, Watson CL, Baird SM. Promoting family-centered care in high risk pregnancy. J Perinat Neonatal Nurs. 1999;13(1):27–42.
Tluczek A, Zaleski C, Stachiw-Hietpas D, Modaff P, Adamski CR, Nelson MR, Reiser CA, Ghate S, Josephson KD. A tailored approach to family-centered genetic counseling for cystic fibrosis newborn screening: the Wisconsin model. J Genet Couns. 2011;20(2):115–28.
Kavanagh KT, Tate NP. Models to promote medical health care delivery for indigent families: computerized tracking to case management. J Health Soc Policy. 1990;2(1):21–34.
Ainsworth F. Family centered group care practice: model building. In Child and youth care forum 1998 Feb 1 (Vol. 27, no. 1, pp. 59-69). Kluwer Academic Publishers-Human Sciences Press.
Ahmann E, Bond NJ. Promoting normal development in school-age children and adolescents who are technology dependent: a family centered model. Pediatr Nurs. 1992;18(4):399–405.
Grebin B, Kaplan SC. Toward a pediatric subacute care model: clinical and administrative features. Arch Phys Med Rehabil. 1995;76(12):SC16–20.
Kazak AE. Comprehensive care for children with cancer and their families: a social ecological framework guiding research, practice, and policy. Child Serv Soc Policy Res Pract. 2001;4(4):217–33.
Davison KK, Lawson HA, Coatsworth JD. The family-centered action model of intervention layout and implementation (FAMILI) the example of childhood obesity. Health Promot Pract. 2012;13(4):454–61.
Monahan DJ. Assessment of dementia patients and their families: an ecological-family-centered approach. Health Soc Work. 1993;18(2):123–31.
Reid Ponte PR, Peterson K. A patient-and family-centered care model paves the way for a culture of quality and safety. Crit Care Nurs Clin. 2008;20(4):451–64.
Ekman I, Swedberg K, Taft C, Lindseth A, Norberg A, Brink E, Carlsson J, Dahlin-Ivanoff S, Johansson IL, Kjellgren K, Lidén E. Person-centered care—ready for prime time. Eur J Cardiovasc Nurs. 2011;10(4):248–51.
Uijen AA, van de Lisdonk EH. Multimorbidity in primary care: prevalence and trend over the last 20 years. The European journal of general practice. 2008;14(sup1):28–32.
Cameron JI, Gignac MA. “Timing it right”: a conceptual framework for addressing the support needs of family caregivers to stroke survivors from the hospital to the home. Patient Educ Couns. 2008;70(3):305–14.
Download references
Acknowledgements
G. Naglie is supported by the George, Margaret and Gary Hunt Family Chair in Geriatric Medicine, University of Toronto.
We would like to thank and acknowledge the contributions of Jessica Babineau, Information Specialist at the Toronto Rehabilitation Institute - University Health Network, for providing guidance on the search strategy development, and conducting the literature search.
We would like to thank and acknowledge the contributions of Jazmine Que. and John Nguyen, Masters of Occupational Therapy Students- The University of Toronto, for reviewing subsets of the retrieved articles and extracted study data.
Author information
Authors and affiliations.
Rehabilitation Sciences Institute, Faculty of Medicine, University of Toronto, 500 University Avenue, Suite 160, Toronto, ON, Canada
Kristina M. Kokorelias & Jill I. Cameron
Dalla Lana School of Public Health, Institute for Work and Health, University of Toronto, 481 University Avenue, Suite 800, Toronto, ON, Canada
Monique A. M. Gignac
Department of Medicine and Institute of Health Policy, Management and Evaluation, University of Toronto, 3560 Bathurst Street, Room 278, Kimel Family Building, Toronto, ON, Canada
Gary Naglie
Department of Medicine, and Affiliated Scientist, Rotman Research Institute, Baycrest Health Sciences, 3560 Bathurst Street, Room 278, Kimel Family Building, Toronto, ON, Canada
Department of Occupational Science and Occupational Therapy, Rehabilitation Sciences Institute, Faculty of Medicine, University of Toronto, 500 University Avenue, Suite 160, Toronto, ON, Canada
Jill I. Cameron
You can also search for this author in PubMed Google Scholar
Contributions
KMK and JIC conceptualised and designed the study. KMK, JIC, GN and MAMG contributed to the interpretation of the data and to the drafting of the initial and revised manuscripts. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Jill I. Cameron .
Ethics declarations
Ethics approval and consent to participate.
Not applicable
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:.
Search Strategy Example (Medline). (DOCX 13 kb)
Additional file 2:
Data Abstraction. (DOCX 90 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Kokorelias, K.M., Gignac, M.A.M., Naglie, G. et al. Towards a universal model of family centered care: a scoping review. BMC Health Serv Res 19 , 564 (2019). https://doi.org/10.1186/s12913-019-4394-5
Download citation
Received : 14 February 2019
Accepted : 01 August 2019
Published : 13 August 2019
DOI : https://doi.org/10.1186/s12913-019-4394-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Family centered care
- Family caregiving
- Patient-care
- Patient education
- Scoping review
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Nursing: Family Centered Care
Introduction.
The information should be accurate between the patient, family members, and the care providers to ensure that quality service is offered.
The care providers need to learn about family background and culture and traditions. This will enable them to create a conducive environment for the health care workers
Much attention can be given to patients in critical conditions if they are near their family members. They will also enjoy the freedom to follow their taste and preferences unlike in hospital-based care where the management determines the diet
It will also enable the care providers to identify the possible barriers that can hinder effective service delivery
It is different from the traditional health care system in that it involves both the patient and the family in deriving a solution to the medical problem (Sisterhen et al 2007, p2).
Literature review
The practice of FCC ensures that both the patient and family are considered as the units of health care (Mitchell, Burmeister, and Foster 2009, p3). The health assurance and well-being of the patients in a critical care environment are affected by the good relationships obtained through the partnership between the family and the professionals.
The strengths, culture, and traditions in a given family will directly impact how a patient relates to the family
These barriers could be those that prevent the patients and families from enjoying such services. They could be those preventing the care providers from effectively delivering their services, e.g. a strange culture and tradition
Sharing the information among the family, the patients, and the professionals will enable health assurance since an appropriate resolution can be made that suits everyone.
The care given under partnership will help reduce the burden that would be put on the health care providers.
There is a need to outline the kind of care that is to be given to the patient and give a description of the delivery process
There is also a need to examine the possible interventions that can be made to meet the needs of both the patients and their families
Family-centered care should be given the necessary precautions to achieve its desired objective. A well-delivered FCC shall ensure that the intended quality services are given to the patients and their families.
Fundamentals of FCC philosophy
There are various key elements of Family-centered care (Cooley & McAllister 1999, p120). The elements can be broadly grouped into these three categories. These are the fundamental principles that govern an effective family-centered care practice. Each of the parties involved should respect and recognize the roles that each has in providing the needed care ( Marshall et al 2002, p2). There should be no overdependence on one party and neither should a party, particularly the staff, consider it wrong for the other to be involved.
The information on the medical history of the patients as well as the economic needs of the family will greatly affect the course of treatment to be provided. Such information should therefore be welcomed by the hospital staff and the family should also be willing to provide it
The care, especially in an ICU environment, should be considered a collective responsibility that requires the services of both parties.
Learning Model
The learning model outlines how the learning process shall be conducted and what is required of the instructor and the learner
The learners should understand the necessities in a learning environment and ensure that they comply with such provisions.
The Adult Learning Theory
The Adult Learning Theory assumes that the learners are very mature people, and who have gained some knowledge in the past. The basics are therefore not very necessary
Interactive learning enables the instructor to identify what the learners are not getting correctly and make clarification appropriately.
The adult learners often have other engagements and it will be very necessary that the learners, as well as the instructor, keep time.
There is a need to have penalties for non-compliance with the learning principles like time management. Specify the consequences of lateness and stress on the dangers of being a passive learner
Interventions to Meet the Needs of the Patients
A patient in a critical condition may lose the courage to ever get better. Words of encouragement from the family members may not sound like truth to such a patient who may have been bedridden for long or underwent amputation in the leg. The nurses are responsible for restoring this lost confidence in the patients
In a situation where there are conflicts in the course of action to be taken about the patient’s care, the nurses should have an upper say to protect the patient. This is because they understand the physiological needs of the body better than the families do
Interventions to Meet the Needs of the Families of the Patient
An important need by the family that should be addressed is the assurance that their patient would recover (Gavaghan & Carroll 2002, p3). The nurses should help the families in identifying their strengths and weaknesses and the possible causes of barriers that can be encountered in providing FCC services. The next move is to assist them to develop these strengths while attempting to alleviate the weaknesses
The assessment of how the family understands the physiological and physical bodily mechanisms will enable the nurses to make an appropriate decision in response to the information that is obtained from the family.
The family of the patient is often interested in knowing the condition of the patient and whether an improvement is recorded or not Gavaghan & Carroll 2002, p3).
Teaching the family the normal physiological functioning of the body will enable them to make an informed decision. They shall be taking a course of action whose purpose and ultimate consequences are well known to them.
The family members should be aware of the important role that they should play in ensuring that their patient receives quality care services.
The beliefs and culture in a given area can affect the people’s perception of the practice of FCC. The nurses should therefore examine such cultural practices and educate the families on the dangers of being stuck to them, especially in a situation that requires crucial medical attention.

Barriers to the Family-Centered Care
The delivery of family-centered care has several challenges that it faces and still allows for the adoption of the traditional system of care. Some of these obstacles stem from within the healthcare center while others are from the families of the patients
The factors could be obstacles to either the professionals who would wish to provide quality services or to the patients and families who would want to obtain the quality services.
Barriers to the patient and family
In practicing family-centered care, there may be a resolution that the family members be close to the patient if the latter has to be hospitalized. The space that is available in the hospital may not allow for that, hence this shall be a barrier.
The infrastructural facilities in the hospital, as well as the entire region, will greatly affect the delivery of family-centered care services. If the patients are being nursed at home, poor conditions of the roads may not allow the professionals who have limited time to assess the patients’ progress effectively. Other facilities like water and electricity will greatly affect the necessary care given to the patients, especially in critical conditions.
Some professionals find it professionally unethical to involve the opinions of the patients and their families in addressing the issues that concern the patient’s health. The patients and family needs will thus not be considered in decision making posing challenges to an effective FCC
The patients and families are maybe not aware of the need to have such a kind of care system. They then adopt the traditional system that it is the professional who knows what to do and should be fully responsible for the steps to be taken.
They may also be unaware of the services even though they may be practiced in a given center.
Lack of enough resources in the patients family can be of absolute threat to effective family-centered care
Barriers to the Professionals
The ratio of physicians to patients is growing smaller and smaller with the increasing number of patients that need attention. The average physician time per patient is thus a scarce resource that may not allow for family-centered care. Financial constraints may also not allow for the physicians to effectively deliver the services at home.
Barriers on the Professionals Cont’
A care provider would be positively willing to practice FCC, however, if such a program is not supported by the management then the professional may not effectively deliver the services. It is the responsibility of the management of a health institution to ensure that such services are instituted and supported
The nurses should be conversant with the cultural beliefs and practices in a given community from which the patient hails. Some communities do not believe in medical treatment. An important guideline is to help the family and patient understand and appreciate the effectiveness of health care systems (MacDougall 2007, p1)
A care provider may fail to collaborate with a given family due to the conflicting cultural beliefs and practices that exist between them
The data about the lab results, admission and discharge dates, and chart reviews are not easy to keep in practice family-centered care. This will eventually pose a problem when attempting to evaluate how such practices progress to make the necessary improvements.
Creating Conducive Environment
Creating a conducive environment for the delivery of family-centered care is mainly concerned with the management of the health institution. They are the interventions that the staff need to make to ensure the effective delivery of FCC (Bowden & Greenberg 2009, p10) They need to have a positive attitude towards the service.
They should do away with what is referred to as ‘latent conditions’ characterized by the poor environment with the administration not intending to make changes (Reiling, Hughes & Murphy n.d, p1).
The expansion of accommodation facilities will allow for more members of the family to be present at the patient’s bedside when there is a need for it.
Alternating the visiting hours will also allow for more members of the family to be present at a patient’s bedside during the visiting time.
The family members who are accommodated to support their patient should be provided with incentives to make him feel at home. Involvement in the activities like sports will enable the family to overcome the stress of nursing their beloved member
The conferences shall enlighten the family on the health matters and enable them to make an informed decision concerning their patient’s needs.
Consistent means of communication will ensure that the family and the hospital are in touch all the time. Any emergency case can then be dealt with immediately.
The family needs to be introduced into the institution. They should be made to feel part of the institution for whatever period it will turn out to be.
It is important to understand that the families that shall be met come from different cultural backgrounds. The nurses should be conversant with the cultures and allow them as long as they are consistent with the regulations of the institution on such issues. Religious culture should not be discouraged since a kind of divine intervention is often required in a critical health condition
It is however important to note that some families may have uncontrolled emotions that may distort the whole practice if they are tolerated (York 2004, para8).
The independent body will easily identify the needs of the family and advise the hospital on the necessary course of action
Expansion of the hospital staff will increase the time that a nurse will have for each of his/her patients.
Evaluation of Family-Centered Care Practices
Evaluation of how the practice of Family-centered care is necessary after such a system has been adopted (Hanson & Randall, 1999, para.1).
It is an integrated process that requires drawing information from various sources and involving the families with ICU patients. The information should be drawn from different sources and over a long period.
The purpose for Evaluation of FCC Practices
In as much as it might appear as a test to the performance of the nurses, evaluation of Family-Centered care can be advantageous if properly carried out. The evaluation mainly focuses on the practices that are going on currently and can help in identifying the possible reinforcements to be made
Much of the patient and family needs will be identified only in an evaluation process. The kinds of questions that are often designed relevant to the objectives of evaluation enable the care providers to learn more about the needs of their patients
The exercise will also enable the care providers to learn how their services are perceived in the given area by different groups of an individual.
Assessing the progress that the practices have shown can be a good indicator of performance and often cultivates in the spirit of hard work in the care providers. The poor result is supposed to alert them to have the required corrective measures.
Role of an Acute Care PNP in FCC. A case study
The role that an acute care pediatric nurse practitioner has is very essential in family-centered care. Diabetes is often a disorder caused by abnormal synthesis of sugar. The amount of sugar to be consumed is therefore restricted by a medical specialist
It is important to understand the medical history of a patent as this may help the nurse and the physician to quickly identify the cause of the problem
The period that the wound had taken to dry out was essential as it gave a hint on the possible cause of this ailment
Hemophilia is a blood disorder where blood takes too long to clot following a deficiency in clotting factors. The kind of diagnosis done to a hemophiliac is not the same as that given to a bleeding non-hemophiliac, the latter requires weaker clotting agents. The first physician had not enquired into this possibility
The fact that John’s father was a hemophiliac gives a possibility that he could be a hemophiliac as well.
The bacterium Clostridium tetani is a rapidly multiplying species and gets into the body through a wound. It invades the muscles there as it fights its way into the nervous system
It is important to understand the extent that an infection has gone. Diagnosis will often depend on the stage that disease is in when it is reported for medication
It is important to have an open consultation between the patient, family, and medical practitioners. It is also important to examine first the patient and family’s understanding of the health problem that has been identified and the necessary course of action.
Do not forget to get the patient’s point of view especially in a critical situation like an amputation.
The PNP intervened here to meet the family needs of the mother. This mother had a career that could not allow her to attend to her son in the hospital. Her other children were still in the educational institution while the father had died two years before. They were very free to share their information, which is an integral part of family-centered care (Kitchen 2005, p2). The nurse offered to take John as her own even after the arrival of John’s aunt. This was particularly necessary because John had no immediate family member. In a critical situation where he had undergone an amputation, he needed to receive support, comfort, and assurance from a specialist. He had to be close to a care provider (Davidson 2009, para10).
The mother needed to leave her number so that she would be consulted during emergencies. John also required special meals following the previous directions from the physician.
Both John and her aunt were provided with the necessary and conducive environment that allowed for quick recovery. This would see him be discharged two weeks before the anticipated period.
The care that has been traditionally adopted does not provide for the consideration of the needs of the patients and families. It gave a lot of dependence on the health care specialists, and the families were in many cases denied their roles as the primary care providers.
It is important to consider the needs of the patients and families to provide a full health care service. The hospital staff should not consider it as an intrusion by the family if the latter are intervening, rather they should share the emerging information to be able to adopt the appropriate treatment procedures.
All the parties should adhere to the philosophies involved in the FCC practices. Both the family and the hospital staff need to recognize and respect the role that each of them has in providing the necessary care services. They should collaborate by sharing the necessary information regarding the medication history of the patient as well as the economic status of the family. This can often determine the appropriate measures to be taken. The care provider should be considered as teamwork requiring the participation of both the family and the hospital staff.
Putting family-centered care into practice: a response to the adaptive practice model. Developmental and Behavioral Pediatrics , 20 (2), 120-122.
Bowden, V. and Greenberg, C. (2009) Children and Their Families: The Continuum of Care . 2 nd ed. Philadelphia: Lippincott Williams & Wilkins.
Cooley, W. C., & McAllister, J. W. (1999). Putting family-centered care into practice: a response to the adaptive practice model. Developmental and Behavioral Pediatrics , 20 (2), 120-122.
Davidson, J. E. (2009). Family-centered care: meeting the needs of patients’ families and helping families adapt to critical illness. Critical Care Nurse, 29(3), 28-34. Web.
Gsavaghan, S. R., & Carroll, D. L. (2002). Families of critically ill patients and the effect of nursing interventions. Dimensions in Critical Care Nursing, 21(2), 64-71. Web.
Hanson, J. L., & Randall, V. F. (1999). Evaluating and improving the practice of family-centered care. Pediatric Nursing, 25(4), 445-449. Web.
Johnson, B. H. (2000). Family-centered care: four decades of progress. Family Systems and Health, 18, 137-156.
Kitchen, B. (2005). Family-centered care. Journal for Specialists in Pediatric Nursing, 10(2), 93-97. Web.
MacDougall, d. (2007). Incorporate family members in the care of ICU patients: New Guidelines Provide First Evidence-Based Standards. Web.
Marshall, M., Fleming, E., Gillibrand, W., and Carter, B (2002). Adaptation and negotiation as an approach to care in pediatric diabetes specialist nursing practice: a critical review. Web.
Mitchell, M., Chaboyer, W., Burmeister, E., & Foster, M. (2009). Positive effects of a nursing intervention on family-centered care in adult critical care. American Journal of Critical Care, 18(2), 543-552. Web.
Reiling, J., Hughes, R. & Murphy, M. (n.d). The Impact of Facility Design on Patient Safety. Web.
Sisterhen, L. L., Blaszak, R. T., Woods, M. B., & Smith, C. E. (2007). Defining family-centered rounds. Teaching and Learning in Medicine, 19(2), 319-322.
York, N. L. (2004). Implementing a family presence protocol option. Dimensions of Critical Care Nursing, 23(2), 84-88.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Whose centre is it anyway? Defining person-centred care in nursing: An integrative review
Amy-louise byrne.
Central Queensland University School of Nursing, Midwifery and Social Science, Townsville, Queensland, Australia
Adele Baldwin
Clare harvey, associated data.
All relevant data are within the manuscript and its Supporting Information files.
The aims of this literature review were to better understand the current literature about person-centred care (PCC) and identify a clear definition of the term PCC relevant to nursing practice.
Method/Data sources
An integrative literature review was undertaken using The Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline, Scopus and Pubmed databases. The limitations were English language, full text articles published between 1998 and 2018 within Australian, New Zealand, Canada, USA, Europe, Ireland and UK were included. The international context off PCC is then specifically related to the Australian context.
Review methods
The review adopted a thematic analysis to categorise and summarise themes with reference to the concept of PCC. The review process also adhered to the Preferred Reporting System for Meta-Analysis (PRISMA) and applied the Critical Appraisal Skills Programme (CASP) tools to ensure the quality of the papers included for deeper analysis.
While definitions of PCC do exist, there is no universally used definition within the nursing profession. This review has found three core themes which contribute to how PCC is understood and practiced, these are People , Practice and Power . This review uncovered a malalignment between the concept of PCC and the operationalisation of the term; this misalignment was discovered at both the practice level, and at the micro, meso and micro levels of the healthcare service.
The concept of PCC is well known to nurses, yet ill-defined and operationalised into practice. PCC is potentially hindered by its apparent rhetorical nature, and further investigation of how PCC is valued and operationalised through its measurement and reported outcomes is needed. Investigation of the literature found many definitions of PCC, but no one universally accepted and used definition. Subsequently, PCC remains conceptional in nature, leading to disparity between how it is interpreted and operationalised within the healthcare system and within nursing services.
Introduction
Healthcare is changing, for both providers and recipients of care, with ongoing challenges to traditional roles and power balances. The causative factors of changes to the way healthcare is provided are complex, but one contributing factor is easier access to healthcare information and better-informed populations [ 1 ] whereby people as healthcare consumers have access to healthcare information through multiple media. On the surface, consumers are no longer seen as passive recipients of care, but rather as valuable and active members of the healthcare team. The concept of Person-Centred Care (PCC) is used to describe a certain model for the role of the patient within the healthcare system and the way in which care is provided to the patient [ 2 , 3 ]. Globally, there is continued advocacy for person-centred, individualised care [ 4 ], with the contemporary term for PCC being frequently presented in healthcare discourse, and frequently associated with the safety and quality of healthcare service provision [ 5 , 6 ]. Indeed, partnering with consumers within a person-centred framework is now a fundamental requirement for Australian healthcare services, meaning that they cannot achieve accreditation without demonstration of PCC [ 7 ]. Hence, PCC is now seen in healthcare service strategy and models of care, designed to support the voice of the patient and the role of the healthcare service in engaging with patients [ 6 ]. PCC also forms part of the Australian nursing professional standards [ 8 ] yet is paradoxically described as an ‘extra’ to nursing practice [ 9 ], taking a back seat to nursing tasks and errands that make up the day to day regime of the nurse.
Despite the discourse around PCC, and the requirements of PCC within healthcare, there appears to be no universally accepted definition of the term. This leaves the concept open to interpretation and potential confusion, particularly when personnel, in this case nurses, attempt to operationalise it. This review investigated the meaning of PCC with reference to nurses across different practice settings and specialities. To further facilitate the understanding [ 10 ] and theory development of the concept of PCC, this review adopted an integrative review methodology [ 11 ].
In the late 1950’s and 60’s, PCC, and care for the entire self was first described in the context of psychiatry, such as in Rogers’ ‘On becoming a person’ [ 12 ]. Patient-centred medicine was a term first coined by psychoanalyst Michael Balint. Balint was instrumental in the education of general practitioners around psychodynamic factors of patients and challenged the traditional illness-orientated model [ 13 ]. Balint’s challenge extended beyond the traditional healthcare model to include both the physical and psychosocial as part of the practitioner’s role. Balint explained; “Here , in additional to trying to discover a localized illness or illnesses , the doctor also has to examine the whole person in order to form what we call an ‘overall diagnosis . ’ The patient , in fact , has to be understood as a unique human-being . ” [ 13 p269].
The idea of caring for the whole person, and the divide between traditional medical practice and the psychosocial needs of the patient was discussed by Engle in 1977. He wrote; “The dominant model of disease today is biomedical…It assumes disease to be fully accounted for by deviations from the norm of measurable biological (somatic) variables . It leaves no room within its framework for the social , psychological , and behavioural dimensions of illness . ” [ 14 p379]. The biopsychosocial model proposed provided a new basis for care which included care of the mind and body. Over the succeeding years, this model of care and the notion of patient centre care continued to evolve, with many iterations of the term moving with the changing climate of healthcare systems.
PCC gained significant traction through the Institute of Medicines (IOM) 2001 report ‘Crossing the Quality Chasm: A New Health System in the 21 st Century’ [ 15 ] as a key element of quality healthcare. The IOM provided one of the first contemporary definitions, stating that PCC “encompasses qualities of compassion , empathy and responsiveness to the needs , values and expressed preferences of the individual patient” [ 15 p48]. The World Health Organization continues to advocate for integrated care that is in tune with the patient’s wants and needs through the framework on Integrated People-Centred Care. This includes the vision that “all people have equal access to quality health services that are co-produced in a way that meets their life course needs” . [ 5 ] This framework aims to improve engagement of people and communities, strengthen governance and accountability, reorientate the model of healthcare, and coordinate services across sectors [ 5 ], seeing people as important contributors and decision makers over their own care.
More recently, the Australian Commission on Safety and Quality in Health Care (ACSQHC) defines PCC as an “innovative approach to the planning , delivery , and evaluation of health care … [involving] mutually beneficial partnerships among health care providers , patients , and families . ” [ 2 p13]. Thus, PCC has become an integral element of care from a quality, planning and practice level, and therefore appears prominently in Australian healthcare service discourse and associated models of care, often presented as an underpinning philosophy for the way in which nursing care is provided [ 3 ]. The concept of PCC continues to evolve, notably in the change to ‘person’ rather than ‘patient’ in recognition of the whole person, not simply the disease process. Other variables such as Family-centred care are used more in the context of aged care and paediatrics [ 16 , 17 ].
As the term has become more common in healthcare discourse, frameworks have emerged to allow the term to be operationalised into practice. There are several person-centred nursing frameworks including the Senses [ 18 ], VIP [ 19 ], 6 C’s [ 20 ], The Burford Model [ 21 ] and McCormack and McCance’s framework [ 22 ]. These frameworks describe elements such as attributes of staff, methods of interactions, coordination of care and services, the care environment and consideration of outcomes of care. These examples provide insight into attempts to operationalise PCC, into individual practice and healthcare service provision.
Nurses are the healthcare professionals who spend the most time with people and are therefore in a position to act as their advocates, with nursing staff managing the continuity of care [ 23 ]. This review seeks to investigate the meaning of person-centred nursing practice, and acts as a starting point for a wider study into the concept of PCC for people with long term conditions. Consumers of healthcare navigate a complex and fragmented system, with fragmentation leading to patients feeling lost, and a decrease in the quality of services offered [ 24 ]. This places even greater importance on a partnership between provider and receiver, particularly in the face of increasing chronicity/complexity of care. Within this fragmented and complex system, the patient must always remain at the centre of their care. Hence, there is a need for a robust definition to ensure PCC is more clearly operationalised and care delivered is designed around the needs of the patient, rather than trying to make the patient fit within the system.
This review uses the term person rather than patient in recognition of the person as a whole. Where clarity is required, the term healthcare consumer is used; a term frequently used in Australia.
The aim of this literature review was to understand better from the literature how nurses operationalise the definition of PCC.
Search questions
This literature review sought to answer the following questions:
- Is there a commonly/generally accepted definition for PCC that is used by nurses?
- How do nurses operationalise PCC in practice?
Search strategy
An integrative literature review was conducted using the terms Person Cent* Care OR Patient Cent* Care AND Nurs* AND Definition OR Meaning OR understanding OR Concept. The search was expanded to include similar terms and concepts such as patient/person-centredness and personalisation. A major subject heading of ‘patient centred care’ was used within the searches. This review is positioned within the nursing discipline; therefore, articles were included if they were specific to nursing or if they included nursing texts in the review. English language, full text articles published between 1998 and 2018 were included. Publications from Australia and New Zealand, Canada, USA, Europe, UK and Ireland were included to gain an understanding of PCC in the western context. The Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline, Scopus and Pubmed databases were searched. This search is registered with PROSPERO (ID number 148778) and was completed in March 2019. While the search strategy includes international literature, this will be related back to the Australian context, in order to understand how PCC operates within Australia.
Data extraction
The framework, from Whittemore and Knafl [ 11 ], describes a comprehensive review, identifying the maximum number of eligible primary sources and requires the researcher to explicitly justify decisions made in the sampling. Using this framework, a total of 1817 articles met the search terms, highlighting the volume of literature available on the concept of PCC. Table 1 provides the scope of inclusions and exclusions. From this, 255 articles were selected for review.
After removal of duplicates, 203 articles were subjected to full review. A further refined strategy excluded Key Performance Indicators (KPI), service measures, assessment tools and validations as the goal was defining the term, rather than to assess how it is measured; these represented a large proportion of the articles within the search. A total of 44 articles were subjected to quality review. To ensure adequate rigour, reliability and relevance, all articles were evaluated against the Critical Appraisal Skills Programme (CASP) systematic and qualitative review checklists [ 25 , 26 ] by the lead author and reviewed by a senior researcher on the team. The relevance of the papers and the quality of the reviews/articles themselves was appraised. All articles were appraised against the aims of this review. Following this, a total of 17 articles were included in the final review. Fig 1 provides the summary for the search process while S1 File provides the PRISMA checklist.

Using the previously identified framework that allowed for data from diverse methods and approaches to be analysed and compared, a constant comparison method was used to convert data from different categories into patterns, themes and relationships. The data is thus displayed below in Table 2 to encompass the full depth of the concept and to provide new understanding, and its implications to practice [ 11 ]. Table 2 demonstrates the characteristics of the articles reviewed including their design methods, populations and findings.
This review set out to investigate if a universal definition of PCC for nursing exists and is used; what was uncovered was a deeper understanding of the concept and operationalisation of PCC, highlighting a malalignment between concept and reality. Three (3) core themes were identified in the review process, each of which is comprised of two (2) sub-themes. These three core themes of People , Practice , and Power , with the respective sub-themes are discussed are summarised in Table 3 .
Theme 1: People
Unsurprisingly, the most common threads in the literature about PCC relate to people and, consistent with the philosophy of PCC, is described as basic, human kindness and respectful behaviour [ 22 , 27 , 28 , 29 ]. The core theme of People comprises two sub-themes: Recognising uniqueness and Partnerships .
Recognising uniqueness
PCC, as the name suggests, is care that is considered and based on the individual person, who is the recipient of care. Prominent in the literature are the concepts of personhood, individuality and uniqueness [ 16 , 28 , 30 ]. Individuality, and the sense of self, understands that each person has their own unique wants, needs and desires [ 16 , 29 ] Personhood reinforces and values the complete person, with an understanding that illness affects the entire person [ 31 ]; an holistic consideration of the person that extends to family interventions and involvement [ 27 , 32 ] described as developing and maintaining trust within the family unit [ 33 , 34 ]. Uniqueness is central to this subtheme as recognition of the person as a unique being leads to unique and tailored care, based on the needs of the whole person [ 16 , 29 ].
Partnership
The literature discusses the need for a relationship between healthcare provider and healthcare receiver as a way of facilitating information, knowledge and decision making. The term ‘relationship’ is prominent in the literature including the terms therapeutic relationship [ 16 ], clinical relationship [ 35 ] and partnership [ 29 , 36 , 37 ]. This is described in the contexts of cohesive, cooperative teams [ 29 , 32 ], mutuality between provider and receiver [ 38 ], and the balance of power and the sharing of knowledge [ 16 ]. These themes are further developed through the practice of the nurse and are thus carried forward to the next theme, Practice.
Theme 2: Practice
PCC is a product of person-centred practice, particularly in the context of nursing. However, the ability to practice PCC is influenced by professional and system factors. The core theme of Practice is comprised of the sub-themes Doing and Space .
‘Doing’ refers to the complex interplay of professional attributes, behaviours and tasks that makes up the daily remit of the nurse; that is, the ‘doing’ of nursing is a combination of these things within the care environment. Personal attributes of nursing staff emerge as a common element in the literature related to PCC. The literature describes attributes such as communication, respect, values, empathy, compassion and non-judgemental behaviour [ 9 , 29 ]. Lusk and Fater [ 7 ] further describe such attributes as caring, faith and hope, trust, relationships, teaching, learning and listening. In describing a framework to facilitate the practice of person-centred care, McCormack and McCance [ 22 ] discussed professional competence, interpersonal skill, job commitment and professional insight. Others have extended this to include understanding vulnerability, fear, the patient identity [ 30 ] and highlight the need to recognise the person as competent to make decisions [ 31 ]. This view, centred on dignity and privacy and the moral and ethical behaviours of the nurse [ 16 , 28 ], facilitates the relationship and balance of power with the person. Delivering whole person care includes elements such as respect for the individual [ 16 ], and planning care that is based on individual needs [ 25 ]. In practice, this is described as the person being valued for their lived experience, life stories [ 9 , 16 ] and the continuation of self [ 34 ]. Kitson et al. [ 35 ] describe this as addressing both the physical and emotional needs of the person and alleviating anxiety.
The existing literature alludes to the idea of opening a space to practice PCC. The literature describes this as being flexible within the care, offering choice [ 9 , 31 ], and creating opportunities for people to engage [ 34 ]. Practicing PCC involves freely giving information to the person [ 36 ] and finding the time to listen and engage with them [ 36 , 39 ], which implies that PCC is a proactive way of delivering nursing care. Gachoud et al. [ 32 ] found that nurses see themselves as most important in delivering PCC, with Doctors playing a lesser role in PCC practice. This understanding creates a concept whereby nurses are pivotal in creating an environment in which the person can truly engage.
While PCC is an individual practice method, the environment within which nurses’ practice must be considerate and supportive of the delivery of PCC as a significant priority; a view supported by McCormack and McCance [ 22 ] in their description of organisational systems and leadership within PCC. Despite competing priorities and the associated tasks of daily practice, nurses must find and open a space to practice PCC as an essential element of the profession. Interestingly, PCC within the literature is often discussed as an addition to nursing tasks. Edvardsson et al. state that promoting PCC in aged care includes doing ‘little extras’ [ 9 p50], such as understanding the patient’s life story, making eye contact and using the person’s name. Marshall et al. found that nurses describe PCC as ‘making the effort’ and ‘going the extra mile’ [ 37 p2667], being helpful and timely with care and attention. Others describe making choices available [ 16 ], ascertaining priorities [ 27 ] and doing the ‘right’ thing [ 31 ].
Theme 3: Power
PCC as a concept is about balancing power between the provider and receiver of care. The notion of PCC is imbued with connotation of power, discussed in relation to all elements of the care and is intertwined in some way with all themes within this review. The sub-themes of Power are the Power over one’s care and the Power to practice PCC .
Power over one’s care
The idea of power balance is discussed in the literature and includes the sharing of knowledge [ 29 ], respect for decision making and individualised care based on these decisions [ 28 , 17 ]. Further to this is the notion of the person having ‘active’ involvement in the care process [ 22 , 35 ]. This is described through identification of the person’s strengths and reinforcing this through the care continuum [ 16 , 38 ]. In addition to this, the literature describes empowerment, promoting the sense of self efficacy [ 31 , 33 , 37 ], supporting the person to be as self-managing as possible [ 36 ] or to have a level of autonomy in their care. Here, the person holds the power in care planning and decision making throughout the care journey and there is a responsibility of knowledge transference and the maintenance of personal autonomy [ 35 ]. This is apparent in the literature through concepts such as control, rights, patient involvement and participation [ 27 , 33 , 35 ]. PCC, however, places importance on a marriage between provider and receiver as a process of sharing knowledge, rather being entirely self-governing, in which the provider (as the custodian of knowledge) has an obligation to impart knowledge.
The power to practice PCC
The need for care systems to be innovative and make a commitment to PCC comes through in the literature [ 22 ], as well as the need for the environment to allow for flexibility and to factor time and space to practice PCC [ 9 , 36 ]. This is a significant shift from the traditional biomedical model, whereby emphasis on personal choice [ 33 ] and partnerships [ 17 ] must be considered within all layers of the healthcare system. Barriers and enablers including workplace culture, leadership [ 22 ], policy and practice, organisational systems, environment [ 28 , 35 ], workload, and ward culture [ 37 ] were identified. The literature also included topics around cost [ 28 ], care coordination [ 28 , 33 ] and of course, outcomes of clinical care provided [ 27 , 29 , 30 ].
Jakimowicz et al. [ 30 ] noted the conflict between system standards, benchmarking and the provision of PCC in a time poor environment. Consistently, the literature discussed the idea of measuring PCC as a method of quantifying this important element of nursing practice amongst the myriad of measurable tasks nursing time is allocated to. The need and ability to measure PCC is cited as crucial for quality improvement of care [ 31 , 38 ]. This review excluded articles related to the measurement of PCC as the primary aim was to find how PCC was defined, however this was still very much a part of the discussion around the meaning and practice of PCC. Morgan and Yoder [ 31 ] discussed several measurement tools, finding them to align more with the effect of care rather than the care directly. Lawrence & Kinn [ 27 ] found that outcome measures used where often in line with the needs and requirements of clinicians, auditors and researchers, or hospital clinical outcomes [ 33 ], rather than with the goals of the patient. Outcomes vary from self-care, patient satisfaction, well-being and improved quality of care [ 28 , 31 , 38 ] to improved adherence and decreased hospitalisation [ 29 ]. This highlights competing priorities within the nursing profession and demonstrates that nursing time is conflicted between what they ‘should’ do and what they ‘must’ do, hence highlighting a nurses limited power to practice PCC in the context of the system standards.
The review demonstrates that the concept of PCC is indeed a method of providing care, or the way in which nurses deliver care. To be person-centred, the nurse must recognise the person as unique, form meaningful partnerships, open a space within the doing of their day to involve and engage with the person, allowing the person control and power of their care.
It is interesting to note that while the existing literature covers a wide variety of clinical areas, and patient and staff perspectives, there were indeed core common themes of PCC. Despite the core concepts associated with PCC taking on more importance within certain clinical areas; for example, continuation of self in aged care [ 9 , 34 ], patient advocacy for intensive care [ 30 ], or communication in stroke care [ 27 ], they are consistent across specialities with the themes building on one another. Perhaps the reason why PCC has been so widely accepted is that the characteristics are simple, kind, human interactions, valuing both the person and the care provider. While definitions of PCC exist, there is no one universally used definition of PCC in nursing practice, potentially compounding a degree of separation between practice and healthcare systems. The findings demonstrate a tension between the theory and the conceptualisation of PCC, and as a result, the operationalisation of the term at both the practice level and a wider healthcare service level.
At the practice level, the theory/practice gap for PCC was evident. The theory/practice gap includes elements of practice failing to reflect theory, perceptions of theory being irrelevant to practice, and ritualistic nursing practice. Consequences of the theory/practice gap can greatly influence nursing practice and collaboration [ 40 ]. In the context of PCC, the theory/practice gap is apparent in the challenge of translating the ideas of PCC into a concrete concept. It is of significance that PCC is seen as ‘extra’ or additional to nursing tasks when these professional behaviours are in line with the Australian Nursing Professional Standards [ 8 ], which requires that they are an intrinsic element of the nursing profession. In fact, to be a registered nurse in Australia one must demonstrate respect for the person as the expert, respect autonomy and “ share knowledge and practice that supports person-centred care” [ 8 ]. This highlights an important matter for consideration; why are core elements of PCC being viewed as ‘going the extra mile’ rather than a core competency for nurses? Certainly, from the perspective of the professional standards, PCC should not be the road less travelled, but rather the daily standard practice of nursing. One answer to this may be the task orientation of the contemporary nursing culture that sees nurses required to meet organisational time allocations for care [ 41 ]. Sharp, McAllister and Broadbent [ 42 ] uncovered a tension between PCC and nursing culture, finding that nurses were increasingly bogged down with tasks and processes, taking them away from the people that they provide nursing care for. These authors found that this led to a feeling of frustration and helplessness in nurses who appear to have accepted the culture of auditable, measurable activities and processes, particularly within the climate of organisational accreditation requirements. This activity-based nursing environment manifests in missed nursing care largely related to patient centred elements, e.g. discharge planning, communication within the healthcare team, absence of adequate patient education on key factors of care such as medication guidance, functional assessment and so on [ 43 , 44 ].
Further, it is apparent that the concept of PCC cannot be isolated from other philosophies of nursing practice and in fact, is embedded in other approaches to nursing care. For example, as outlined by Kim [ 45 ], nursing is defined by dimensions, rather than characteristics. If PCC is considered as a dimension, a complex, interwoven mix of characteristics, then it is possible to gain some concrete understanding of PCC in the context of all clinical areas. The five dimensions proposed by Kim reflect the ‘human’ side of nursing practice, and like the general interpretation of PCC, shows how human interactions, values and knowledge combine to provide care. Kim goes on to say that these dimensions vary with individual nurses and changing clinical situations; which seems to fit with the current confusion about PCC giving choice and decision-making power to patients. As found in this review, PCC attempts to balance the power between providers of care and receivers, giving choice and decision-making power. Yet the focus on nursing tasks and prioritisation of these tasks is evident, demonstrating the malalignment between concept and practice, where research has identified that the current task-oriented system of nursing does fail to meet the care needs of patients [ 46 ].
Nursing practice, however, is only one element of delivering PCC within the healthcare system. This disparity extends between the concept of PCC and its ability to exist within the current healthcare system itself, where time to care is explicitly rationed through budgets that do not allow for individualised person-centred care [ 47 ].
The notion of PCC is one centred on mutuality and a balance of power; a distinct move from the paternalistic biomedical model to a biopsychosocial model that is guided by the person, rather than the disease process. However, in current healthcare services, care is often system centred. That is, care is organised, funded and coordinated in a way that meets the needs of the system or service [ 28 , 33 ]. System fragmentation is understood to have significant influence on people accessing care, whereby people with long-term and complex conditions are most vulnerable to the negative impact from the lack of care coordination and cohesion [ 48 ].
In Australia, complex funding models are central to the concept of system fragmentation which begins at the Commonwealth and State funding levels [ 48 ], making it difficult for patients to navigate the system. System silos remain a significant issue for healthcare services and for the delivery of care, with Medicare models remaining fragmented for specialist services [ 49 ]. The States are the healthcare system managers, yet the federal government holds the responsibility of leading primary healthcare. This presents a challenge in provided collaborative and integrated services, particularly for those with long-term conditions [ 50 ]. The OECD highlight the importance of reducing system fragmentation in order to ‘Improve the co-ordination of patient care .’ [ 50 p1].
Indeed, system fragmentation leads to an increased ‘treatment burden’, whereby poor treatment coordination, ineffective communication and confusion about treatments can contribute to poor health outcomes and greater levels of cost, time, travel and medications for the person [ 51 ] Sav et al. [ 51 ] discuss the need for individualised and coordinated services across specialities as a requirement for reducing treatment burden. In addition to this, the Australian Charter of Healthcare Rights prescribes the rights of those seeking care in any Australian service and includes the right to access, respect, communication and participation [ 52 ]. Accreditation of healthcare services is conditional to evidence of multi-level partnerships with consumers of health. Positive partnerships (PCC) are clearly linked to improved access to care, which in turn leads to reports of positive experiences and better-quality healthcare. Of critical importance at an organisational and government level, the standards also describe this partnership as a mechanism for reducing hospital costs through improved rates of preventable hospitalisation and reducing hospital length of stay [ 7 ].
Potentially Preventable Hospitalisations (PPH) place considerable economic and resource burden on the healthcare system, with approximately 47% of PPH being attributed to long-term conditions [ 53 ]. Thus, reducing preventable hospitalisation is a measurable target for healthcare services under the National Healthcare Agreement as a way of controlling the escalating costs of care and maintaining sound fiscal management of public services [ 54 ]. In line with the ACSQHC standard Partnering with Consumers , PCC has been introduced to some services as a mechanism for improving communication between services and those with long term conditions. What is less clear, is how care tailored to the individuals wants and needs of the patient (PCC), exists within a system predominately focused on reducing variation and the associated costs of care. While the philosophy of PCC naturally fits within the care environment, understanding how effective it is, how the person is included and how outcomes important to the person are captured, take a lower precedent to the measure of reduced hospital costs, self-efficacy and reduced hospitalisation. Capturing what is important for the individual presents a difficult task for services providing population-based care.
These system wide constraints provide a considerable challenge to nurses in their attempts to operationalise the concept of PCC. Nursing, it seems, has become task orientated, a sentiment supported by Foe & Kitson who found that nurses are constrained by a ‘checklist’ mentality, whereby completing and documenting tasks is seen as more important than engaging with the person [ 55 p100]. These tasks and checklists align with the requirements of the National Standards for hospital accreditation. An example of this is the need to collect data on the use of invasive devices or the allocated time intervals in which screening (such as skin inspection and falls risk) must occur; for example within eight (8) hours of admission [ 7 ]. Indeed, policy and procedure for nursing practice reflect that of the need of accreditation and national policy requirements as opposed to the needs of individual people. While partnering with consumers is an important element of the standards [ 7 ], quantifying the way in which healthcare services and indeed nurses engage with patients is less clear. Kitson states ‘ Nursing theory , it would seem , has been limited by the profession’s ability to systematically document the complexity and richness of what happens when nurses and patients (and their careers) interact’ [ 35 p99], an issue it seems stemming from the fact that nursing interventions promoting person-centred, compassionate care are poorly described, with little to no consensus on the term, and interventions that do exist are poorly evaluated [ 56 ]. On top of this, nurses are generally not encouraged, nor enabled to reflect on practice in order to generate new insights and nursing practice [ 35 ]. Molina-Mula et al. [ 23 ], discuss the nursing profession as being the key to professional teamwork models, meeting the needs of patients and thereby increasing their personal decision-making capacity. However, it is possible that PCC is hindered by the level of professional autonomy, time and space afforded to nurses [ 57 ]. Indeed, the malalignment discussed herein, demonstrates that nurses may be hindered at higher levels of system compliance or difficulties in coordinating care services, which permeates nursing culture and ultimately nursing practice, limiting their ability to provide PCC that is individualised to the people seeking care.
Finally, while this review excluded articles related to the measurement and indicators of PCC, this is undoubtedly linked to its perceived meaning and how it is operationalised. This review demonstrates that the understanding of PCC is made up of how and where PCC appears in healthcare discourse and shows that PCC is potentially skewed by how it is(n’t) measured and the outcomes that are(n’t) reported as a product of PCC. This finding presents a framework within which further investigation of the concept of PCC (Meaning, Practice, Measures, Outcomes) within healthcare services could be undertaken. This proposed framework will be applied by the author to conduct further research into the role of PCC within nurse-led service for people with long-term conditions.
Implications for practice
This review highlights the dominant discourse around the concept of PCC yet uncovered the idea of malalignment between the rhetoric and the reality of the concept. Further exploration of the alignment between healthcare services and the goal of PCC may prove beneficial in ensuring the practice of PCC is fostered from all levels of the healthcare service. The above provides a rationale for why the definition of PCC should be provided, given that the concept is currently somewhat nebulous in nature. A consistent definition, with reference to all levels of the healthcare service including practice, will ensure that the concept stays true to the philosophy of compassionate and balanced care. Any definition provided should carefully consider how PCC is measured and prioritised within the healthcare system, which has the potential to move the concept from its current rhetorical nature, to a genuine commitment and priority of nurses and services. Lastly, the review provides a basis for the importance of nursing education and workforce development of the concept and the practice of PCC, given the apparent barriers that nurses may face in delivering PCC.
Limitations
This integrated review was limited to articles relating to the nursing profession and hence has excluded reviews on PCC in relation to other disciplines. Practice related elements such as procedure, service measures and outcomes of PCC were excluded from this review as the aim was to find a generalised way of defining the term. Furthermore, only one framework met the criteria of the search strategy and was included, there are however, several frameworks for PCC in nursing and hence some elements of PCC and their definitions may have been excluded.
This review was performed with published literature only, with no investigation of grey literature undertaken. PCC is often discussed in healthcare service literature, including procedure, service profiles and service strategy. This information will undoubtedly have an impact on how nurses understand and practice PCC within their own area and within their service. This review was designed to investigate a universal definition of PCC as described in the literature and hence chose to limit this to an academic search. The practice of PCC from a policy to practice perspective perpetuates meaning and will be the subject of further research for the author.
This review was conducted as a starting point for the author’s research higher degree (PhD) studies, and hence the search strategy and quality processes were completed by one person. All elements of the review were discussed at length with academic supervisors to ensure adequate rigor and accuracy throughout the search, review and integrative process.
The concept of PCC is well known to nurses, yet ill-defined and operationalised into practice. Healthcare service policy and care provisions, and indeed nursing services, need a clear definition of PCC in order to work toward embedding it into practice and into models of care in a meaningful and genuine way. However, PCC is potentially hindered by its apparent rhetorical nature, and further investigation of how PCC is valued and operationalised through its measurement and reported outcomes will serve the philosophy of PCC well. Investigation of the literature found many definitions of PCC, but no one universally accepted and used definition. Subsequently, PCC remains conceptional in nature, leading to disparity between how it is(n’t)operationalised within the healthcare system and within nursing services. In light of the malalignment discovered within this review, a universal definition of PCC is not provided herein; instead, this review highlights the need for further investigation of PCC between the levels of the healthcare service (at the micro, meso and macro levels) and how this influences the critical work that nurses do in supporting people through their healthcare journey.
Supporting information
Funding statement.
The author(s) received no specific funding for this work. The publication is funded under the first authors Research Higher Degree (PhD) budget.
Data Availability
- PLoS One. 2020; 15(3): e0229923.
Decision Letter 0
PONE-D-19-26103
Whose Centre is it Anyway? Defining Person-Centred Care in Nursing
Dear Mrs Byrne,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
We would appreciate receiving your revised manuscript by Feb 16 2020 11:59PM. When you are ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter.
To enhance the reproducibility of your results, we recommend that if applicable you deposit your laboratory protocols in protocols.io, where a protocol can be assigned its own identifier (DOI) such that it can be cited independently in the future. For instructions see: http://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols
Please include the following items when submitting your revised manuscript:
- A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). This letter should be uploaded as separate file and labeled 'Response to Reviewers'.
- A marked-up copy of your manuscript that highlights changes made to the original version. This file should be uploaded as separate file and labeled 'Revised Manuscript with Track Changes'.
- An unmarked version of your revised paper without tracked changes. This file should be uploaded as separate file and labeled 'Manuscript'.
Please note while forming your response, if your article is accepted, you may have the opportunity to make the peer review history publicly available. The record will include editor decision letters (with reviews) and your responses to reviewer comments. If eligible, we will contact you to opt in or out.
We look forward to receiving your revised manuscript.
Kind regards,
Janhavi Ajit Vaingankar
Academic Editor
Journal Requirements:
When submitting your revision, we need you to address these additional requirements:
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at http://www.plosone.org/attachments/PLOSOne_formatting_sample_main_body.pdf and http://www.plosone.org/attachments/PLOSOne_formatting_sample_title_authors_affiliations.pdf
2. Please include the study type, Integrative Review, in the title. Please cite articles where those Integrative Review protocols are described in detail, and include sufficient information the methods to be understood independent of these references ( https://journals.plos.org/plosone/s/submission-guidelines#loc-materials-and-methods ).
3. We note you have included a table to which you do not refer in the text of your manuscript. Please ensure that you refer to Table 2 in your text; if accepted, production will need this reference to link the reader to the Table.
4. Please ensure that you refer to Figure 1 in your text as, if accepted, production will need this reference to link the reader to the figure.
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Yes
Reviewer #2: Yes
2. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #2: N/A
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: Praise to the authors for having written a good review highlighting seminal information on Person-Centered Care (PCC). The methodological approach is clear and appropriate. The approach used in the process of eligibility of studies included is also clear with a supporting table, however, it is not clear how quality appraisal using CASP was applied to the studies included.
Results: The results are presented concisely, clearly and make sense with respect to the aim of the review but could have been longer to elaborate on the characteristics of the papers included in the review.
Discussion: The discussion is good and linked to theory and practice. However, a higher level of discussion was needed here. There could have been a better debate highlighting the linkage or differentiating features of PCC from similar concepts such as patient centered care or patient and family centered care.
Conclusion: Very clear and linked to the study findings. The fact that authors attempted to highlight current literature on person centered care, this could have been more interesting if they could have highlighted the differences in terms of definition by the different scholars or institutions.
Advice for improvement of the manuscript: as this is an integrative review, it could offer more in the way of future direction for defining the concept of PCC.
Reviewer #2: This is an interesting paper that has the potential to inform policy change in the future. The review itself seems quite strong, however, the international/Australian focus needs more clarity. In the literature search strategy you have chosen to include multiple jurisdictions which have important differences in healthcare system functioning. However, in each section when you give examples they are only focused on the Australian context. While I understand that for the definition of PCC the inclusion of more broad context is helpful, consider carefully how the operationalization will be different in different jurisdictions and the policy/practice challenges. I suggest you either make it clear that this global review of definitions is only being applied to the Australian context, or diversify your examples throughout. This will also be important for the corresponding terminology that you use – the term consumer for example is rarely used in the Canadian healthcare context so it will be important early in the paper to define such terms and outline which contexts they are used and comparable terms in each of the other jurisdictions. Also related to terminology in Canada, we would refer only to the ‘healthcare system’, not the ‘health system’ as there is an acknowledgement that it is not about preventative health.
Here are some more minor changes throughout:
Introduction:
Page 3, line 47-49 “The concept of Person-Centred Care (PCC) is used to describe the role of the patient within the health system and the way in which care is provided to the patient [2,3].”
- This is to describe a certain model for the role of the patient – not the role of patients in general – this implies it is a way to describe patients in all care models
Page 3, line 52-58 – accreditation is based on jurisdiction – which jurisdiction are you referring to? Same with nursing professional standards.
Page 4, line 59 – healthcare not health
Page 4, line 63 – is this different nursing contexts as in hospitals vs community or different countries where they practice?
Background:
Page 5, line 84 – when was this report created? What happened between 1977 and 2000? Add a sentence here, likely wasn’t a 20-30 year period without any changes.
Page 5, line 86 – is this the first definition of PCC? It’s the first you mention as far as I can tell for this specific term, might be important to mention this if it is the first attempt to define it.
Line 89 – is this WHO framework? Unclear who’s framework – please specify
Line 94 – awkward “of their own care” consider changing to about their own care or over their own care.
Line 96-97 – this quote is cut a little awkwardly – consider adding a word in square brackets to make it flow better like [involving].
Line 98 – from not form
Again your aim and scope doesn’t specify an Australian context, rather an international application. Either make clear in the introduction that this paragraph about Australia’s ACSQHC is an example from the various jurisdictions. Potentially consider including an example from another country to support the international focus of the paper.
Paragraph starting line 104 seems disconnected from previous paragraph. Consider adding a sentence at the beginning that bridges and waiting until the second sentence to list examples of frameworks. Consider moving the sentence on 110 to this paragraph as it justifies the move from PCC in general to nursing frameworks specifically.
Line 114-116 – combine these 2 short sentences.
- The first aim – to better understand the literature – seems vague, can you be more specific here? Consider combining with the search question – ie the aim could be to understand better from the literature how nurses operationalize the definition.
Line 144 – you don’t specify you use this framework, make this clear
Figure 1 – are you missing the arrow from screening to eligibility?
How many papers are citing the same papers?
Consider creating a figure or table summarizing each of the themes and subthemes to allow a visualization of your results that is easier for readers to refer to.
Line 200 – ‘based’ not ‘base’.
Line 237 – take out the “the” before people.
Line 240 – need to define the term medical officer, either in this paragraph or as a footnote.
Line 281 – access to what?
Line 290 – if measuring PCC is important to the discussion and still part of the papers you reviewed it would be helpful to add a sentence or two here to justify why you didn’t include them.
Discussion:
Lines 302-305 – abrupt switch between these two sentences, consider a sentence in between moving from stating it’s a model of care to what the reader must assume is the definition that emerged from the review.
Line 325 – they are ‘an’ intrinsic element.
Line 330 – core business – consider core competency or another word that is more in line with healthcare and patient centredness.
Line 354 – this sentence seems unfinished – should it say “giving choice and decision-making power to patients”?
Line 360 – again should be healthcare system throughout.
Again this is an Australian example, consider diversifying or adding a second country example to make the argument that your paper has international scope.
Implications for practice:
Again this is another section to clarify the jurisdiction you are talking about and be careful about the suggestions you are making here and in the conclusion about policy and practice. It could be helpful to say that across the western countries included general things need to change and give a couple of specific examples in different countries.
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
Reviewer #1: Yes: Frank Kiwanuka
Reviewer #2: No
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files to be viewed.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email us at gro.solp@serugif . Please note that Supporting Information files do not need this step.
Submitted filename: PONE-D-19-26103_review.docx
Author response to Decision Letter 0
Thank you for the comprehensive feedback on the manuscript Whose Centre is it Anyway? Defining Person-Centred Care in Nursing; An Integrative Review. The valuable feedback has been considered and changes have been made as per the table below. Please find attached a revised copy of the manuscript with tracked changes and a complete copy with changes embedded. Once again, we thank you for your time and consideration and we look forward to your consideration of this new version.
Yours sincerely
Amy-Louise Byrne (Corresponding author)
Please see the rebuttal letter for a detail account of the changes made
Submitted filename: Response to Reviewers letter.docx
Decision Letter 1
PONE-D-19-26103R1
Whose Centre is it Anyway? Defining Person-Centred Care in Nursing: An Integrative Review
We would appreciate receiving your revised manuscript by Mar 20 2020 11:59PM. When you are ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
1. If the authors have adequately addressed your comments raised in a previous round of review and you feel that this manuscript is now acceptable for publication, you may indicate that here to bypass the “Comments to the Author” section, enter your conflict of interest statement in the “Confidential to Editor” section, and submit your "Accept" recommendation.
Reviewer #1: (No Response)
2. Is the manuscript technically sound, and do the data support the conclusions?
3. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #1: N/A
4. Have the authors made all data underlying the findings in their manuscript fully available?
5. Is the manuscript presented in an intelligible fashion and written in standard English?
6. Review Comments to the Author
Reviewer #1: The authors have sufficiently responded to the previous comments and thanks for submitting the revision. However, they could consider expanding on the background by including more literature from other countries which have significantly contributed to literature person-centered care. Some suggestions, there is plenty of literature coming from the University of Gothenburg Center or Person centers care GPCC and Finland on this topic. This will reflect a global picture on the topic. Were there any assumptions that the authors made about including the countries specified?
7. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
Author response to Decision Letter 1
The feedback from the reviewers is appreciated. Please see the rebuttal letter for a response to the reviewers. No changes have been made to the manuscript on this third submission
Submitted filename: Response to Reviewers letter 2.docx
Decision Letter 2
19 Feb 2020
PONE-D-19-26103R2
Dear Dr. Byrne,
We are pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it complies with all outstanding technical requirements.
Within one week, you will receive an e-mail containing information on the amendments required prior to publication. When all required modifications have been addressed, you will receive a formal acceptance letter and your manuscript will proceed to our production department and be scheduled for publication.
Shortly after the formal acceptance letter is sent, an invoice for payment will follow. To ensure an efficient production and billing process, please log into Editorial Manager at https://www.editorialmanager.com/pone/ , click the "Update My Information" link at the top of the page, and update your user information. If you have any billing related questions, please contact our Author Billing department directly at gro.solp@gnillibrohtua .
If your institution or institutions have a press office, please notify them about your upcoming paper to enable them to help maximize its impact. If they will be preparing press materials for this manuscript, you must inform our press team as soon as possible and no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact gro.solp@sserpeno .
With kind regards,
Additional Editor Comments (optional):
Acceptance letter
25 Feb 2020
Dear Dr. Byrne:
I am pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please notify them about your upcoming paper at this point, to enable them to help maximize its impact. If they will be preparing press materials for this manuscript, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact gro.solp@sserpeno .
For any other questions or concerns, please email gro.solp@enosolp .
Thank you for submitting your work to PLOS ONE.
PLOS ONE Editorial Office Staff
on behalf of
Ms Janhavi Ajit Vaingankar
- Free Samples
- Premium Essays
- Editing Services Editing Proofreading Rewriting
- Extra Tools Essay Topic Generator Thesis Generator Citation Generator GPA Calculator Study Guides Donate Paper
- Essay Writing Help
- About Us About Us Testimonials FAQ
- Studentshare
- Family centred care
Family centred care - Essay Example
- Subject: Nursing
- Type: Essay
- Level: Masters
- Pages: 9 (2250 words)
- Downloads: 6
- Author: ivarussel
Extract of sample "Family centred care"
- Cited: 0 times
- Copy Citation Citation is copied Copy Citation Citation is copied Copy Citation Citation is copied
CHECK THESE SAMPLES OF Family centred care
Evidence relating to family issue, interprofessional working by health professionals to improve quality of health, theory of nursing models, delivering family centred care, importance of interprofessional working, participating with the health care team and meetings in relation to child protection, ethics and research in professional contexts, family-oriented program models and professional helpgiving practices.

- TERMS & CONDITIONS
- PRIVACY POLICY
- COOKIES POLICY
- Popular Professionals
- Design & Planning
- Construction & Renovation
- Finishes & Fixtures
- Landscaping & Outdoor
- Systems & Appliances
- Interior Designers & Decorators
- Architects & Building Designers
- Design-Build Firms
- Kitchen & Bathroom Designers
- General Contractors
- Kitchen & Bathroom Remodelers
- Home Builders
- Roofing & Gutters
- Cabinets & Cabinetry
- Tile & Stone
- Hardwood Flooring Dealers
- Landscape Contractors
- Landscape Architects & Landscape Designers
- Home Stagers
- Swimming Pool Builders
- Lighting Designers and Suppliers
- 3D Rendering
- Sustainable Design
- Basement Design
- Architectural Design
- Universal Design
- Energy-Efficient Homes
- Multigenerational Homes
- House Plans
- Home Remodeling
- Home Additions
- Green Building
- Garage Building
- New Home Construction
- Basement Remodeling
- Stair & Railing Contractors
- Cabinetry & Cabinet Makers
- Roofing & Gutter Contractors
- Window Contractors
- Exterior & Siding Contractors
- Carpet Contractors
- Carpet Installation
- Flooring Contractors
- Wood Floor Refinishing
- Tile Installation
- Custom Countertops
- Quartz Countertops
- Cabinet Refinishing
- Custom Bathroom Vanities
- Finish Carpentry
- Cabinet Repair
- Custom Windows
- Window Treatment Services
- Window Repair
- Fireplace Contractors
- Paint & Wall Covering Dealers
- Door Contractors
- Glass & Shower Door Contractors
- Landscape Construction
- Land Clearing
- Garden & Landscape Supplies
- Deck & Patio Builders
- Deck Repair
- Patio Design
- Stone, Pavers, & Concrete
- Paver Installation
- Driveway & Paving Contractors
- Driveway Repair
- Asphalt Paving
- Garage Door Repair
- Fence Contractors
- Fence Installation
- Gate Repair
- Pergola Construction
- Spa & Pool Maintenance
- Swimming Pool Contractors
- Hot Tub Installation
- HVAC Contractors
- Electricians
- Appliance Services
- Solar Energy Contractors
- Outdoor Lighting Installation
- Landscape Lighting Installation
- Outdoor Lighting & Audio/Visual Specialists
- Home Theater & Home Automation Services
- Handyman Services
- Closet Designers
- Professional Organizers
- Furniture & Accessories Retailers
- Furniture Repair & Upholstery Services
- Specialty Contractors
- Color Consulting
- Wine Cellar Designers & Builders
- Home Inspection
- Custom Artists
- Columbus, OH Painters
- New York City, NY Landscapers
- San Diego, CA Bathroom Remodelers
- Minneapolis, MN Architects
- Portland, OR Tile Installers
- Kansas City, MO Flooring Contractors
- Denver, CO Countertop Installers
- San Francisco, CA New Home Builders
- Rugs & Decor
- Home Improvement
- Kitchen & Tabletop
- Bathroom Vanities
- Bathroom Vanity Lighting
- Bathroom Mirrors
- Bathroom Fixtures
- Nightstands & Bedside Tables
- Kitchen & Dining
- Bar Stools & Counter Stools
- Dining Chairs
- Dining Tables
- Buffets and Sideboards
- Kitchen Fixtures
- Wall Mirrors
- Living Room
- Armchairs & Accent Chairs
- Coffee & Accent Tables
- Sofas & Sectionals
- Media Storage
- Patio & Outdoor Furniture
- Outdoor Lighting
- Ceiling Lighting
- Chandeliers
- Pendant Lighting
- Wall Sconces
- Desks & Hutches
- Office Chairs
- View All Products
- Designer Picks
- Side & End Tables
- Console Tables
- Living Room Sets
- Chaise Lounges
- Ottomans & Poufs
- Bedroom Furniture
- Nightstands
- Bedroom Sets
- Dining Room Sets
- Sideboards & Buffets
- File Cabinets
- Room Dividers
- Furniture Sale
- Trending in Furniture
- View All Furniture
- Bath Vanities
- Single Vanities
- Double Vanities
- Small Vanities
- Transitional Vanities
- Modern Vanities
- Houzz Curated Vanities
- Best Selling Vanities
- Bathroom Vanity Mirrors
- Medicine Cabinets
- Bathroom Faucets
- Bathroom Sinks
- Shower Doors
- Showerheads & Body Sprays
- Bathroom Accessories
- Bathroom Storage
- Trending in Bath
- View All Bath
- Houzz x Jennifer Kizzee
- Houzz x Motivo Home
- How to Choose a Bathroom Vanity

- Patio Furniture
- Outdoor Dining Furniture
- Outdoor Lounge Furniture
- Outdoor Chairs
- Adirondack Chairs
- Outdoor Bar Furniture
- Outdoor Benches
- Wall Lights & Sconces
- Outdoor Flush-Mounts
- Landscape Lighting
- Outdoor Flood & Spot Lights
- Outdoor Decor
- Outdoor Rugs
- Outdoor Cushions & Pillows
- Patio Umbrellas
- Lawn & Garden
- Garden Statues & Yard Art
- Planters & Pots
- Outdoor Sale
- Trending in Outdoor
- View All Outdoor
- 8 x 10 Rugs
- 9 x 12 Rugs
- Hall & Stair Runners
- Home Decor & Accents
- Pillows & Throws
- Decorative Storage
- Faux Florals
- Wall Panels
- Window Treatments
- Curtain Rods
- Blackout Curtains
- Blinds & Shades
- Rugs & Decor Sale
- Trending in Rugs & Decor
- View All Rugs & Decor
- Pendant Lights
- Flush-Mounts
- Ceiling Fans
- Track Lighting
- Wall Lighting
- Swing Arm Wall Lights
- Display Lighting
- Table Lamps
- Floor Lamps
- Lamp Shades
- Lighting Sale
- Trending in Lighting
- View All Lighting
- Bathroom Remodel
- Kitchen Remodel
- Kitchen Faucets
- Kitchen Sinks
- Major Kitchen Appliances
- Cabinet Hardware
- Backsplash Tile
- Mosaic Tile
- Wall & Floor Tile
- Accent, Trim & Border Tile
- Whole House Remodel
- Heating & Cooling
- Building Materials
- Front Doors
- Interior Doors
- Home Improvement Sale
- Trending in Home Improvement
- View All Home Improvement
- Cups & Glassware
- Kitchen & Table Linens
- Kitchen Storage and Org
- Kitchen Islands & Carts
- Food Containers & Canisters
- Pantry & Cabinet Organizers
- Kitchen Appliances
- Gas & Electric Ranges
- Range Hoods & Vents
- Beer & Wine Refrigerators
- Small Kitchen Appliances
- Cookware & Bakeware
- Tools & Gadgets
- Kitchen & Tabletop Sale
- Trending in Kitchen & Tabletop
- View All Kitchen & Tabletop
- Storage & Organization
- Baby & Kids

- View all photos
- Dining Room
- Breakfast Nook
- Family Room
- Bed & Bath
- Powder Room
- Storage & Closet
- Outdoor Kitchen
- Bar & Wine
- Wine Cellar
- Home Office
- Popular Design Ideas
- Kitchen Backsplash
- Deck Railing
- Privacy Fence
- Small Closet
- Stories and Guides
- Popular Stories
- Renovation Cost Guides
- Fence Installation Cost Guide
- Window Installation Cost Guide
- Discussions
- Design Dilemmas
- Before & After
- Houzz Research
- View all pros
- View all services
- View all products
- View all sales
- Living Room Chairs
- Dining Room Furniture
- Coffee Tables
- Home Office Furniture
- Join as a Pro
- Interior Design Software
- Project Management
- Custom Website
- Lead Generation
- Invoicing & Billing
- Landscape Contractor Software
- General Contractor Software
- Remodeler Software
- Builder Software
- Roofer Software
- Architect Software
- Takeoff Software
- Lumber & Framing Takeoffs
- Steel Takeoffs
- Concrete Takeoffs
- Drywall Takeoffs
- Insulation Takeoffs
- Stories & Guides
- LATEST FROM HOUZZ
- HOUZZ DISCUSSIONS
- SHOP KITCHEN & DINING
- Kitchen & Dining Furniture
- Sinks & Faucets
- Kitchen Cabinets & Storage
- Knobs & Pulls
- Kitchen Knives
- KITCHEN PHOTOS
- FIND KITCHEN PROS
- Bath Accessories
- Bath Linens
- BATH PHOTOS
- FIND BATH PROS
- SHOP BEDROOM
- Beds & Headboards
- Bedroom Decor
- Closet Storage
- Bedroom Vanities
- BEDROOM PHOTOS
- Kids' Room
- FIND DESIGN PROS
- SHOP LIVING
- Fireplaces & Accessories
- LIVING PHOTOS
- SHOP OUTDOOR
- Pool & Spa
- Backyard Play
- OUTDOOR PHOTOS
- FIND LANDSCAPING PROS
- SHOP LIGHTING
- Bathroom & Vanity
- Flush Mounts
- Kitchen & Cabinet
- Outdoor Wall Lights
- Outdoor Hanging Lights
- Kids' Lighting
- Decorative Accents
- Artificial Flowers & Plants
- Decorative Objects
- Screens & Room Dividers
- Wall Shelves
- About Houzz
- Houzz Credit Cards
- Privacy & Notice
- Cookie Policy
- Your Privacy Choices
- Mobile Apps
- Copyright & Trademark
- For Professionals
- Houzz vs. Houzz Pro
- Houzz Pro vs. Ivy
- Houzz Pro Advertising Reviews
- Houzz Pro 3D Floor Planner Reviews
- Trade Program
- Buttons & Badges
- Your Orders
- Shipping & Delivery
- Return Policy
- Houzz Canada
- Review Professionals
- Suggested Professionals
- Accessibility
- Houzz Support
- COUNTRY COUNTRY
Gardeners & Lawn Care Companies in Elektrostal'
Location (1).
- Use My Current Location
Popular Locations
- Albuquerque
- Cedar Rapids
- Grand Rapids
- Indianapolis
- Jacksonville
- Kansas City
- Little Rock
- Los Angeles
- Minneapolis
- New Orleans
- Oklahoma City
- Orange County
- Philadelphia
- Portland Maine
- Salt Lake City
- San Francisco
- San Luis Obispo
- Santa Barbara
- Washington D.C.
- Elektrostal', Moscow Oblast, Russia
Professional Category (1)
- Accessory Dwelling Units (ADU)
Featured Reviews for Gardeners & Lawn Care Companies in Elektrostal'
What types of services do gardeners and lawn care companies provide, questions to ask a prospective gardener or lawn care service:, business services, connect with us.

IMAGES
VIDEO
COMMENTS
Introduction. Family centered care is a practice incorporates the family of a patient to be part of intensive care. The family in this case is the patient's relatives or people that the patient considers closest to him. Mitchell et al refer to Family Centered Care as [an innovative approach to the planning, delivery, and evaluation of health ...
1. INTRODUCTION. Family‐centred care (FCC) has received increased attention in recent years outside of paediatric nursing, from which it originated (Cene et al., 2016).In paediatric wards the involvement of family members is almost standard; however, for hospitalized adults, care is shifting slowly to a more family‐centred approach.
The search identified 14,393 papers of which 55 met our criteria and were included. Family-centered care models are most commonly available for pediatric patient populations (n = 40). Across all family-centered care models, the consistent goal is to develop and implement patient care plans within the context of families.
Family Centered Care Family centred care mainly focus on involving family by partnership and collaboration with health care team for the well being of sick family member or child (Kuo, et al., 2012). In pediatric settings families play an important key role with nursing and other medical staff. It is widely excepted concept in most health care ...
As stated earlier, the focus was on theoretical papers and papers that included the word 'concept' and/or conceptual discussion. As family-centered care was found to be on group level, viewing the family as a unit, it will be described first followed by person- and child-centered care on an individual level.
coyne i., o'neill c., murphy m., costello t. & o'shea r. (2011) What does family-centred care mean to nurses and how do they think it could be enhanced in practice. Journal of Advanced Nursing67(12), 2561-2573.. Aim. This paper is a report of the qualitative findings of a multisite survey in seven children's units in Ireland.
Family-centered care has been recognized as being an integral part to patient health, satisfaction and health care quality (Kuo, et al, 2012). Family-centered care is implemented with the goal to increase partnerships between, families, patients and providers; and has been. 878 Words. 4 Pages.
sion. As family-centered care was found to be on group level, viewing the family as a unit, it will be described first followed by person- and child-centered care on an individual level. Family-centered Care Of the 14 articles (see Table 1), seven were systematic reviews that consisted of a Cochrane review of quantitative studies (Shields et al.,
The role of the nurse in family-centered care is viewed as a dynamic process arising out of a blending of appropriate cues inspired by the interaction of uniquely individual personalities. Climate and therapeutic use of the self have been much discussed in relation to the nurse's role. The concept of ombudsman represents a more innovative ...
Children's long- and short-term health and developmental outcomes can be improved when families are engaged and supported, and inform care planning. Family-centred care (FCC) underpins policy directions for universal, community-based, child and family health services in the early years, although its implementation in this context is poorly ...
) emerged in the early 1990s, designed by a New Zealand nurse, Anne Casey, working in the UK. It encompasses two principles: (a) that nursing care for a child in hospital can be given by the child or parents with support and education from the nurse; and (b) that family or parental care can be given by the nurse if the family is absent.
The information should be accurate between the patient, family members, and the care providers to ensure that quality service is offered. In only 3 hours we'll deliver a custom Nursing: Family Centered Care essay written 100% from scratch Get help. The care providers need to learn about family background and culture and traditions.
1 INTRODUCTION. Family-centred care (FCC) has received increased attention in recent years outside of paediatric nursing, from which it originated (Cene et al., 2016).In paediatric wards the involvement of family members is almost standard; however, for hospitalized adults, care is shifting slowly to a more family-centred approach.
To explore the perceptions of family-centred care among nurses and the family members of hospitalised children and investigate the facilitators of and barriers to the implementation of family-centred care in Malawi. Background. In Malawi, approximately 34% of children have long-term illnesses that require hospitalisation.
Other variables such as Family-centred care are used more in the context of aged care and paediatrics [16,17]. ... The relevance of the papers and the quality of the reviews/articles themselves was appraised. All articles were appraised against the aims of this review. ... Defining Person-Centred Care in Nursing; An Integrative Review. ...
The family plays a vital role in the nursing of the patient. Since the discovery of this fact, there has been vast interest on the topic of family-centered care. This essay examines the role of the nurse in planning a patient's discharge, and the considerations they have to make in order to ensure that family -centered care is made possible.
Keywords: philosophy; family-centered care; nurse; child 1. Introduction Family-Centered Care (FCC) as a philosophy is defined as a care provider that em-phasizes and involves the important role of the family, not only focusing on sick children but also healthy children.(Phiri et al., 2022). In the FCC concept, family members are con-
Search for more papers by this author. Suzanne Sheppard-Law BN, MPH (research), PhD, ... The ethnography has given shape to social understandings of busyness, the complexities of paediatric nursing and family-centred care. The culture of care changed in moments of busyness and transformed parent and nursing roles, expectations and collaborative ...
Industry: Remediation and Other Waste Management Services , Metal Ore Mining , Residential Building Construction , Iron and Steel Mills and Ferroalloy Manufacturing , Recycling, waste materials See All Industries, Iron ores, Metal ores, nec, Operative builders, Blast furnaces and steel mills Galvanized pipes, plates, sheets, etc.: iron and steel See Fewer Industries
See other industries within the Health Care and Social Assistance sector: Child Care Services , Community Food and Housing, and Emergency and Other Relief Services , Continuing Care Retirement Communities and Assisted Living Facilities for the Elderly , Home Health Care Services , Individual and Family Services , Medical and Diagnostic Laboratories , Nursing Care Facilities (Skilled Nursing ...
Find company research, competitor information, contact details & financial data for LEMMA, OOO of Elektrostal, Moscow region. Get the latest business insights from Dun & Bradstreet.
The Journal of Clinical Nursing publishes research and developments relevant to all areas of nursing practice- community, ... The systematic literature search yielded 30 theoretical papers; the results are outlined on a PRISMA flow diagram. ... While we know that family-centred care is widely endorsed and enhances well-being, there is a lack of ...
Search 14 Elektrostal' gardeners & lawn care companies to find the best gardener or lawn care service for your project. See the top reviewed local gardeners & lawn care services in Elektrostal', Moscow Oblast, Russia on Houzz.