Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic

RELATED TOPICS
INTRODUCTION
Diagnosis and management of face and brow presentations will be reviewed here. Other cephalic malpresentations are discussed separately. (See "Occiput posterior position" and "Occiput transverse position" .)
Prevalence — Face and brow presentation are uncommon. Their prevalences compared with other types of malpresentations are shown below [ 1-9 ]:
● Occiput posterior – 1/19 deliveries
● Breech – 1/33 deliveries
Cephalic venipuncture
ISSN 2398-2942
Contributor(s) :
- Sheilah Robertson
Introduction
Requirements, preparation, further reading.
- Good sample collection technique is vital to obtain a blood sample of adequate quality for analysis.
- Peripheral veins, eg cephalic and saphenous, often detrimental → slow blood flow → sample artefacts (hemolysis and microclots.)
- Collection of blood for analysis.
- Administration of intravenous drugs +/- fluids Fluid therapy .
- Simple technique (unless difficult animal).
- Straightforward technique for intravenous drug administration.
Disadvantages
- No real advantages over jugular venipuncture Jugular venipuncture for blood collection.
Alternative techniques
- Jugular venipuncture Jugular venipuncture which gives rapid, unobstructed flow of blood.
- Placement of cephalic catheter Cephalic catheterization .
Subscribe To View
This article is available to subscribers. try a free trial today or contact us for more information., publications, refereed papers.
- Recent references from PubMed and VetMedResource .
Register now to access this article free of charge
Receive one free article when you register..
- Hidden Free Article URL --> -->
- First Name *
- Last Name *
- Telephone Number: *
- I am a: * Please Select Student Nurse/Technician Veterinarian Vet School Faculty Pet Owner Other
- Country Select Afghanistan Åland Islands Albania Algeria American Samoa Andorra Angola Anguilla Antarctica Antigua & Barbuda Argentina Armenia Aruba Ascension Island Australia Austria Azerbaijan Bahamas Bahrain Bangladesh Barbados Belarus Belgium Belize Benin Bermuda Bhutan Bolivia Bosnia & Herzegovina Botswana Bouvet Island Brazil British Indian Ocean Territory British Virgin Islands Brunei Bulgaria Burkina Faso Burundi Cambodia Cameroon Canada Canary Islands Cape Verde Caribbean Netherlands Cayman Islands Central African Republic Ceuta & Melilla Chad Chile China Christmas Island Clipperton Island Cocos (Keeling) Islands Colombia Comoros Congo - Brazzaville Congo - Kinshasa Cook Islands Costa Rica Croatia Cuba Curaçao Cyprus Czechia Côte d’Ivoire Denmark Diego Garcia Djibouti Dominica Dominican Republic Ecuador Egypt El Salvador Equatorial Guinea Eritrea Estonia Eswatini Ethiopia Falkland Islands (Islas Malvinas) Faroe Islands Fiji Finland France French Guiana French Polynesia French Southern Territories Gabon Gambia Georgia Germany Ghana Gibraltar Greece Greenland Grenada Guadeloupe Guam Guatemala Guernsey Guinea Guinea-Bissau Guyana Haiti Heard & McDonald Islands Honduras Hong Kong Hungary Iceland India Indonesia Iran Iraq Ireland Isle of Man Israel Italy Jamaica Japan Jersey Jordan Kazakhstan Kenya Kiribati Kosovo Kuwait Kyrgyzstan Laos Latvia Lebanon Lesotho Liberia Libya Liechtenstein Lithuania Luxembourg Macao Madagascar Malawi Malaysia Maldives Mali Malta Marshall Islands Martinique Mauritania Mauritius Mayotte Mexico Micronesia Moldova Monaco Mongolia Montenegro Montserrat Morocco Mozambique Myanmar (Burma) Namibia Nauru Nepal Netherlands New Caledonia New Zealand Nicaragua Niger Nigeria Niue Norfolk Island North Korea North Macedonia Northern Mariana Islands Norway Oman Pakistan Palau Palestine Panama Papua New Guinea Paraguay Peru Philippines Pitcairn Islands Poland Portugal Puerto Rico Qatar Romania Russia Rwanda Réunion Samoa San Marino Saudi Arabia Senegal Serbia Seychelles Sierra Leone Singapore Sint Maarten Slovakia Slovenia Solomon Islands Somalia South Africa South Georgia & South Sandwich Islands South Korea South Sudan Spain Sri Lanka St. Barthélemy St. Helena St. Kitts & Nevis St. Lucia St. Martin St. Pierre & Miquelon St. Vincent & Grenadines Sudan Suriname Svalbard & Jan Mayen Sweden Switzerland Syria São Tomé & Príncipe Taiwan Tajikistan Tanzania Thailand Timor-Leste Togo Tokelau Tonga Trinidad & Tobago Tristan da Cunha Tunisia Turkey Turkmenistan Turks & Caicos Islands Tuvalu U.S. Outlying Islands U.S. Virgin Islands Uganda Ukraine United Arab Emirates United Kingdom United States Uruguay Uzbekistan Vanuatu Vatican City Venezuela Vietnam Wallis & Futuna Western Sahara Yemen Zambia Zimbabwe
We hope your free content was what you wanted
For continued access, sign up today and get:.
Instant access to the knowledge of 1,100+ leading veterinarians
Over 28,000 per reviewed articles, images, videos, sounds, diagnostic trees
More than 1,100 client factsheets
On the veterinary diagnosis and treatment of your choice of species: dogs, cats, rabbits, exotics, horses and cattle.
Starting at:
Interested in more great content?
Sign up today..
On the veterinary diagnosis and treatment of your choice of species: dogs, cats, rabbits, exotics, horses and cattle
How can we help you today?
- Radiology Key
Fastest Radiology Insight Engine
- BREAST IMAGING
- CARDIOVASCULAR IMAGING
- COMPUTERIZED TOMOGRAPHY
- EMERGENCY RADIOLOGY
- FETAL MEDICINE
- FRCR READING LIST
- GASTROINTESTINAL IMAGING
- GENERAL RADIOLOGY
- GENITOURINARY IMAGING
- HEAD & NECK IMAGING
- INTERVENTIONAL RADIOLOGY
- MAGNETIC RESONANCE IMAGING
- MUSCULOSKELETAL IMAGING
- NEUROLOGICAL IMAGING
- NUCLEAR MEDICINE
- OBSTETRICS & GYNAECOLOGY IMAGING
- PEDIATRIC IMAGING
- RADIOGRAPHIC ANATOMY
- RESPIRATORY IMAGING
- ULTRASONOGRAPHY
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Thoracic Key
- Veterinary Medicine
- Gold Member
- iOS/Android App
Asynclitism: Clinical and Intrapartum Diagnosis in Labor
Fig. 6.1 Palpation of the fetal sagittal suture, with vaginal exploration, in eutocic labor with fetal head synclitic Fig. 6.2 Palpation of the posterior and anterior fontanel of the synclitic fetal head, through the vagina, during eutocic labor When neither of the parietal bones precedes the sagittal suture, the head is synclitic (Fig. 6.3 ). If the anterior parietal bone precedes the sagittal suture, there is an anterior asynclitism (Fig. 6.4 ). When the posterior parietal bone precedes the sagittal suture, there is a posterior asynclitism (Fig. 6.5 ) [ 3 ]. Fig. 6.3 Sagittal section of the pelvis and abdomen in labor with the fetus in cephalic presentation ( a ) in posterior asynclitism, ( b ) in anterior asynclitism Fig. 6.4 Palpation of the fetal head sagittal suture during vaginal digital examination, during labor, in left occiput position, transverse, with anterior asynclitism Fig. 6.5 Palpation of the anterior fontanel via the vaginal digital examination, during labor, in left occiput transverse position, with posterior asynclitism In 1858, Smith [ 2 ] reported that in a left occiput anterior (LOA) position, the right side of the cranium is considerably lower than that of the left, so that the most depending part of the cranial surface is the protuberance of the right parietal bone. This lateral depression was called the “obliquity of the head.” When assessing the fetal head at the level of the pelvic inlet in LOA position, the bulging of the right parietal bone is felt through the walls of the anterior portion of the cervix. This is the point with which the finger comes in contact with the most depending part of the head. If the finger is passed in to the cervical os, the sagittal suture is felt crossing the field of the os in an oblique direction. The sagittal suture divides the os unequally, and a larger portion of the middle and upper part of the right parietal bone is included within the ring of the os more than the left. It is this middle and upper portion of the right parietal bone which is felt in making a vaginal examination at this time. The earlier the digital examination is made, the sagittal suture will be found to be more markedly oblique or approaching the transverse direction. The fetal occiput rotates 45° clockwise (from the fetal point of view) from the oblique diameter at the level of the pelvic inlet to the AP diameter in the mid and lower pelvis in its progression in the birth canal. In emerging form of the pelvis, the obliquity of the head is almost as great as at its entrance, the right parietal bone being still lower than the left. The head does not emerge either with the occipital or parietal protuberance foremost, the part which escapes first being a point between the two, namely, the upper and posterior part of the right parietal bone, named parietal eminence or tuber parietale (Fig. 6.6 ) [ 4 ]. Fig. 6.6 Parietal bone different portion of the outer surface [ 4 ], with permission ( left ). Fetal skulls and fetal head diameters, in the circumference are reported the sub-occiput-bregmatic diameter (9,5 centimetres). This diameter to allow the normal engagement of fetal head in the medpelvis, and perform the head asynclitism in distocic labor ( rigth ) Any fetal head position may be associated with asynclitism, and Table 6.1 shows the different kind of asynclitism in all the occiput positions. Table 6.1 The table represents the various forms of asynclitism in the anterior occipital positions of the fetal head To diagnose asynclitism, it is first necessary to determine the position of the fetal occiput with respect to the maternal pelvis. The side to which the occiput is positioned will indicate the laterality of the asynclitism. In an anterior asynclitism, the presenting parietal bone will be opposite to which side it is rotated toward. Conversely, the presenting parietal bone in a posterior asynclitism is the same side to which the occiput is rotated. This holds true regardless of the occiput being positioned anteriorly, posteriorly, or transversely (Fig. 6.7 ). Fig. 6.7 Vaginal digital examination in left occiput transverse with posterior asynclitism. The exploring fingers will palpate the sagittal suture closer to the symphysis Moderate degrees of asynclitism though are the rule in normal labor, and specifically the fetal head in occiput anterior engages with an anterior asynclitism. If it is pronounced enough, it can be responsible of many complications in the maternal and fetal care during the intrapartum period, the most common of which are arrest disorders of the fetal head during descent in the birth canal, even with an otherwise normal size pelvis. The most common etiologies of an excessive nonphysiologic asynclitism may be the peculiar maternal bony pelvic anatomy (Fig. 6.8a–c ), the tone of the pelvic musculature, and the force and consistency of uterine contractions. During the vaginal digital examination, if the sagittal suture is felt to be curving anteriorly (Naegele’s obliquity, Fig. 6.9a, b ) or posteriorly (Litzmann’s obliquity, Fig. 6.10a–d ), such cranial asymmetry increases the diameter of fetal cranium and can lead to dystocia. Fig. 6.8 ( a ) Posterior asynclitism in the flat basin (or obliquity of Naegale phenomenon), with overlapping of the cranial bones, which is a phenomenon of adaptation to the commitment and progression of the fetal head. ( b ) Sellheim theory according to which an egg-shaped body can pass through a cylinder of a size smaller than its transverse diameter, if it breaks down into two parts which are arranged obliquely. ( c ) The molding phenomenon of fetal cranial bones is well visualized by translabial US, especially in the head up. The overlapping of the cranial bones is a positive sign for the performance prediction of spontaneous delivery Fig. 6.9 ( a ) Ultrasound evaluation of posterior asynclitism with translabial longitudinal section, ( b ) Ultrasound evaluation of posterior asynclitism with transabdominal sagittal section Fig. 6.10 ( a ) Fetal head vertex presentation, in the right occiput transverse position with posterior asynclitism. ( b ) Draw representing ultrasonographic evaluation of fetal posterior asynclitism. ( c ) Ultrasound image of fetal posterior asynclitism: midline ( ML ), thalamus ( TH ), and orbit ( O ). ( d ) Posterior asynclitism in right occipital transverse position, displayed by ultrasound (the thicker line passing through the sagittal suture relative to the small line that indicates the degree of asynclitism) Most of the time anterior asynclitism is not diagnosed unless attention is placed to the hollow of the maternal sacrum [ 5 ]. The posterior pelvis feels empty unless the fetal head is at a low station. Failure of the sacral hollow to be occupied by the fetal head is suggesting of a higher fetal head station than what the initial palpation of the presenting part may suggest. As understandable, the presence of asynclitism becomes a very important factor in the already subjective and unreliable diagnosis of correct fetal head station [ 6 , 7 ]. Generally, diagnosis of asynclitism is made subjectively in an indirect way, i.e., when labor slows down or fetal head progression in the birth canal stops. Ultrasound has recently been used as a more objective tool in supporting and validating the clinical diagnosis of asynclitism [ 8 – 12 ]. Different sonographic approaches including transabdominal, transperineal, and transvaginal, both in 2D and 3D, have been utilized in the determination of fetal position based on such landmark as the fetal orbits, cerebellum, midline echo of the brain, and occiput (Fig. 6.11 ) [ 10 , 13 – 18 ]. Fig. 6.11 Perfect synclitism in left occiput anterior position by transabdominal ultrasound ( panel a ), transperineal ultrasound ( panel b ), and transvaginal ultrasound ( panel c ) 6.2 Asynclitism in the Occiput Posterior (OP) Position The occiput posterior position has been easily diagnosed by ultrasound by both approach, transabdominal and transperineal examinations [ 14 , 18 ]. The orbits are an easily identified marker in the fetal head, and they will be directly under the symphysis in the case of direct OP position (Fig. 6.12 ) or toward the upper portion of the right inferior ramus of the pubis, in left occiput position (LOP) or toward the upper portion of the left inferior ramus of the pubis, and in right occiput position (ROP). If the asynclitism is also present, only one orbit will be visualized by ultrasound, the so-called squint sign [ 10 ]. In case of LOP position, the only visualization of the right anterior orbit will be called anterior asynclitism (Fig. 6.13 ), whereas the only visualization of the left posterior orbit will be called posterior asynclitism. The same definitions will be used in case of ROP, where the anterior orbit is the left (Fig. 6.14 ) and the posterior is the right. The OP and OT shows different degrees of asynclitism, anterior or posterior (Fig. 6.15 ) and the “squint sign”, using transabdominal sonography.
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:

Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.

Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.

Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death

Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Normal Normal and Abnormal First Trimester Exam Normal Fetal Ultrasound Biometry Fetal Heart Ultrasound Determining Fetal Situs Fetal Urinary System Umbilical Cord CNS Critical Anatomy CNS Embryology and Early Development CNS Later Development CNS Ultrasound Brain Anatomy
- Fetal Anomalies Fetal Heart Fetal Chest Fetal Colon Fetal Central Nervous System Facial Clefts Skeletal Dysplasia Genetic Markers
- Doppler Editorial Board Fetal Doppler Middle Cerebral Artery Doppler
- Fetal/Maternal Conditions Transvaginal Ultrasound Fetal Anemia Interventions Preterm Labor Placenta and Umbilical Cord
- Twins Key Views Twins: Videos Diamniotic Dichorionic and Diamniotic Monochorionic Twins Monochorionic Monoamniotic Twins Twin to Twin Transfusion Syndrome Fetal Growth Restriction Twin Reversed Arterial Perfusion Conjoined Twins
- Video Topics
- Access CMEs
- Other Links Topics A-Z Links CME Videos Upload Your Case Editorial Board
- Take A Free Tour
- Free Videos
- Editorial Board

Determining Normal Fetal Situs (Situs Solitus)
One of the first steps in obtaining cardiac views is to determine how the fetus is oriented within the uterus and to determine the right and left side of the abdominal contents versus the right and left side of the heart and thoracic contents. This is not as easy as it might seem since the fetal left side can be on the maternal right and the opposite can be true.
In summary, situs refers to the right and left orientation of fetal organs. For example situs solitus is the normal left to right axis arrangement in the fetus with the stomach and spleen on the left side of the body, and the liver and gallbladder on the right side.

Visual Summary of Normal Fetal Situs
Below are steps required to determine situs related to cephalic or breech presentation, and whether the spine or back is up (anterior) or down (posterior).
1. Determine the lie of the fetus:
A. Is the fetus head first with the head in front of the ultrasound screen? This could also be termed cephalic or vertex presentation. B. Is the fetal feet or bottom first with the head behind the screen? This could also be termed footling or breech presentation. C. Determine whether the spine or back is anterior (back up) or posterior (back down).
2. Obtain a transverse cut of the thorax to demonstrate a 4-chamber view. The left atrium is nearest the spine and the cardiac axis points to the left.
Detailed Method to Determine Fetal Situs
1. Define within the uterus the presentation of the fetus (generally vertex or breech; less often the presentation is oblique or transverse.).
2. Determine whether the fetal spine is parallel or transverse to the maternal spine. In sagittal view, if the fetal and maternal spine are parallel, the fetus is in longitudinal lie. When the fetal spine is perpendicular to the maternal spine, the fetus is in a transverse lie.
3. Determine the position of the fetal left side. The fetal left side will be as follows: A. With respect to the maternal abdomen, the fetal left side is anterior and near to the ultrasound transducer. B. With respect to the posterior uterine wall, the fetal left side is posterior and farthest from the transducer. C. With respect to the right uterine wall, the fetal left side will be on the maternal right. D. With respect to the left uterine wall, the fetal left side will be on the maternal left.
4. Obtain a transverse view of the abdomen and define the fetal stomach which is positioned in the left side of the fetal abdomen.
5. Obtain a 4-chamber view of the heart by obtaining a transverse view of the thorax. The left atrium and descending aorta are nearest to the spine and the cardiac axis points to the left.
6. Finally, ascertain if the stomach and heart are in their correct respective locations, i.e., the stomach is on the left side and the cardiac axis points to the left.
7. Place a transverse image of the fetal abdomen and heart side by side and validate that the left side of the fetal abdomen (stomach near to the spine) is concordant with the left side of the fetal heart (left atrium and descending aorta near to the spine). This is done by displaying a side by side comparison of a transverse view through the fetal stomach and a 4-chamber cardiac view.

Above. Normal ultrasound orientation for situs solitus.
Right Hand Rule of Thumb: Introduction
In their article “Sonographic definition of the fetal situs,” Bronshtein, Gover, and Zimmer [ 1 ] describe a “right hand rule of thumb” to define fetal situs during transabdominal scanning, and a “left hand rule of thumb” for transvaginal scanning.

Right Hand Rule of Thumb: Cephalic, supine, back down

Left. The sonographer’s right hand represents the fetus with the thumb pointing to the fetal left. The palm of the hand is anterior, or represents the ventral or face surface of the fetus. The fetus is therefore face up, back down, and the thumb points to the fetal left.
Right. Again, the imaginary fetus is back down with the stomach and cardiac axis pointing to the left. (Ignore color scheme of fetal heart and vessels.)

Right Hand Rule of Thumb: Cephalic, prone, back up
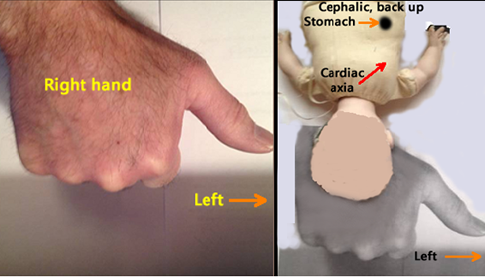
Left. The sonographer’s right hand represents the fetus with the thumb pointing to the fetal left. The top of the hand (dorsal surface or prone position) represents back up.
Right. The imaginary fetus is back up with the stomach and cardiac axis pointing to the fetal left.

Right Hand Rule of Thumb: Breech, supine, back down
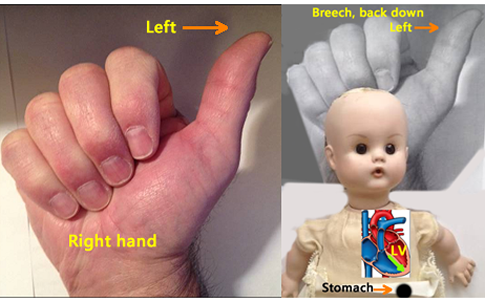
Left. The sonographer’s right hand represents the fetus with the thumb pointing to the fetal left. The palm of the sonographer’s hand is anterior, or represents the ventral surface of the fetus. The fetus is therefore face up, back down, and the thumb points to the fetal left.
Right . The imaginary fetus is back down with the stomach and cardiac axis pointing to the left. (Ignore color scheme of fetal heart and vessels).

Right Hand Rule of Thumb: Breech, prone, back up

Right . The imaginary fetus is back up with the stomach and cardiac axis pointing to the fetal left side.

- Normal CNS Anatomy
- Fetal Situs
- Normal Fetal Ultrasound Biometry

All are web-based courses. Subscribe Today!
- Literature Reviews
- Terms of Use
Fastest Obstetric, Gynecology and Pediatric Insight Engine
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Fetal Situs
● INTRODUCTION The first step in the ultrasonographic evaluation of the fetus is the assessment of fetal visceral situs as some organs are arranged symmetrically and others, such as the abdominal and thoracic organs, are arranged asymmetrically ( 1 ). A clear definition of left and right sidedness in the body is noted since early embryogenesis. A good understanding of fetal situs is important during ultrasound examinations, as some fetal anomalies are associated with abnormal laterality of abdominal and/or thoracic organs. Evaluating the orientation and position of the fetal heart in the thorax and the anatomic relationship of the abdominal organs is part of the targeted fetal cardiac examination. Knowledge of the anatomic landmarks in the chest and abdomen can facilitate the routine cardiac screening examination and provide clues to the presence of cardiac abnormality ( 1 , 2 ). This chapter will focus on the fetal situs, including the anatomic orientation of the organs in the chest and upper abdomen. ● SEQUENTIAL SEGMENTAL ANALYSIS In evaluating fetal cardiac anatomy, a sequential segmental approach helps in the description of cardiac abnormalities in a clear and simple approach. For many years, pathologists and pediatric cardiologists have been using this approach to describe normal and abnormal hearts ( 1 , 3 , 4 ). In the sequential segmental approach, the cardiovascular system is divided into segments, and for each segment, the anatomy, the position, and the connection with the next segment are described. This sequential segmental analysis involves three anatomic regions: the atria, the ventricles, and the arterial trunks. Each anatomic region is also partitioned into a right- and left-sided component. Atrioventricular valves separate the atria from the ventricles, and the semilunar valves separate the ventricles from the arterial trunks. A fourth anatomic segment, systemic and pulmonary venous connections, should also be evaluated. The cardiac chambers are therefore recognized by their morphologic structures rather than their anatomic locations. The direction of blood flow also helps assess the atrioventricular and ventriculoarterial connections. Assessment of visceral situs and cardiac position, which is described in detail in this chapter, should be part of this sequential segmental approach ( 1 , 3 , 4 ). Table 6.1 presents the steps for the sequential segmental analysis in fetal cardiac evaluation. Detailed anatomic evaluation of cardiac chambers, valvular structures, arterial trunks, and venous systems will be presented in the following chapters. TABLE 6.1 Steps for Sequential Segmental Analysis in the Fetus 1. Identify visceral situs 2. Identify atrial arrangement (morphologic right and left atrium) 3. Identify atrioventricular (AV) connections (AV valves) 4. Identify ventricular arrangement (morphologic right and left ventricle) 5. Identify ventriculoarterial connections (semilunar valves) 6. Identify arterial trunk arrangement (aorta and pulmonary artery) 7. Identify systemic and pulmonary venous connections ● FETAL VISCERAL SITUS Assessment of the fetal thoracic and visceral situs is the initial approach to the sequential segmental analysis of the fetal heart by ultrasound ( 5 ). Heterotaxy syndrome commonly involves cardiac and abdominal anomalies, and thus focusing on the fetal heart without an evaluation of the upper abdomen often results in an incomplete diagnosis. Although the current method for the determination of fetal situs relies on the position of the stomach and heart in the abdomen and chest, respectively, careful attention should also be paid to the position of the aorta and inferior vena cava below the diaphragm ( 4 , 5 ) ( Fig. 6.1 ), the orientation of the umbilical vein with the portal sinus, the presence and position of the gallbladder, and when feasible the presence and location of the spleen. It is generally agreed that the positions of the aorta and inferior vena cava below the diaphragm are more reliable criteria for the determination of right or left isomerism than the location of the stomach in the abdomen. Technique 1. Locate the fetal head within the uterus and determine the presenting part (e.g., cephalic, breech) ( Fig. 6.2 ). 2. Determine the fetal lie within the uterus by obtaining a sagittal view of the fetal spine. (Longitudinal lie: when the fetal spine is parallel to the maternal spine; transverse lie: when the fetal spine is perpendicular to the maternal spine; oblique lie: when the fetal spine is oblique to the maternal spine.) 3. After establishing the exact position of the fetus with steps 1 and 2, determine the location of the fetal left side with regard to the maternal abdomen (fetal left side is anterior [closer to the transducer], posterior [closer to the posterior uterine wall], right lateral [closer to the maternal right uterine wall], left lateral [closer to the maternal left uterine wall]) ( Fig. 6.2 ). 4. Obtain a transverse view of the fetal abdomen by rotating the transducer 90 degrees from the sagittal view of the lower thoracic spine. The fetal stomach is imaged in the left side of the abdomen, the descending aorta is posterior to the left, and the inferior vena cava is anterior to the right ( Figs. 6.1 and 6.3 ). In addition, the intrahepatic part of the umbilical vein is seen connecting with the left portal vein and portal sinus with an L-shape to the right ( Figs. 6.1 and 6.3 ). By sliding the transducer toward the fetal chest, a four-chamber view of the heart is imaged. Note that the apex of the heart is pointing toward the left side of the fetal chest ( Figs. 6.2 and 6.4 ). Determining that the stomach, descending aorta, and cardiac apex are located on the fetal left side and the inferior vena cava is located on the right side establishes normal visceral situs ( Figs. 6.1 and 6.3 ). Figure 6.1: Schematic drawing of a cross section of the upper abdomen for the assessment of the abdominal situs. The vertical line divides this plane into right and left. The right-sided structures include the gallbladder, the portal sinus, a large part of the liver, and inferior vena cava (IVC). The left-sided structures include the descending aorta, the stomach, and the spleen. Figure 6.3 is the corresponding ultrasound plane. Figure 6.2: Determining fetal situs in longitudinal lie: In A , the fetus is in a cephalic presentation with the fetal spine close to the left uterine wall, resulting in the right side being anterior and left side posterior. In B , the fetus is in a cephalic presentation with the fetal spine close to the right uterine wall, resulting in the left side being anterior and right side posterior. In C , the fetus is in a breech presentation with the fetal spine close to the left uterine wall, resulting in the left side being anterior and right side posterior. In D , the fetus is in a breech presentation with the fetal spine close to the right uterine wall, resulting in the right side being anterior and left side posterior. Note the corresponding transverse ultrasound planes of the chest and abdomen. Blue arrows point to fetal stomach, red arrows to the apex of the heart, and yellow arrows to the descending aorta. See text for details. Several methods for determining fetal situs during the ultrasound examination have been described. Cordes et al. ( 6 ) described a technique that involves orienting the transducer in a standardized way so that the fetal head is on the right side of the screen in a fetal sagittal plane as a starting point and then rotating the transducer 90 degrees in clockwise to obtain the caudocranial transverse views. Another method reported by Bronshtein et al. ( 7 ) is referred to as the right-hand rule for abdominal scanning and the left-hand rule for transvaginal scanning ( Fig. 6.5 ). The palm of the hand corresponds to the face of the fetus, and the examiner holds the hand according to the side of the fetal face; the fetal heart and stomach are shown by the examiner’s thumb. Figure 6.3: Axial view of the fetal abdomen in a fetus with situs solitus. Note the location of the liver, portal sinus (PS), and inferior vena cava (IVC) in right side (R); and the stomach (St) and descending aorta (Ao) in left side (L). The umbilical vein (UV) is located in the midline. Compare with Figure 6.1 . Figure 6.4: Schematic drawing of a cross section of the thorax at the level of the four-chamber view in a fetus with situs solitus. Note the position of the heart in the left chest with a normal cardiac axis of 45 degrees. See text for details. LA, left atrium; RA, right atrium; LV, left ventricle; RV, right ventricle; Ao, Aorta; L, left; R, right. Situs Solitus, Situs Inversus, and Situs Ambiguous Three types of visceral situs exist: situs solitus, situs inversus, and situs ambiguous ( Table 6.2 ). a.) Situs solitus refers to the normal arrangement of vessels and organs within the body ( Fig. 6.1 ). b.) Situs inversus, with an incidence of about 0.01% of the population, refers to a mirror-image arrangement of organs and vessels to situs solitus. Situs inversus is associated with a slight increase in the incidence of complex congenital heart disease (CHD), in the order of 0.3% to 5% ( 8 ), and with the presence of Kartagener syndrome in about 20% of the cases ( 9 ). Kartagener syndrome, with an autosomal recessive transmission, primarily involves ciliary dysfunction with recurrent respiratory infection and reduced fertility. c.) Situs ambiguous (heterotaxy), which refers to visceral malpositions and malformations different from situs solitus or inversus, is commonly associated with complex CHD, abnormalities in venous drainage, bowel malrotations and obstruction, and splenic, biliary, and bronchial tree abnormalities. The incidence of situs ambiguous has been estimated around 1 per 10,000 infants ( 10 ). Two types of heterotaxy exist: right isomerism and left isomerism. In right isomerism, also referred to as asplenia, both sides of the body show the right morphology; in left isomerism, also referred to as polysplenia, both sides of the body show the left morphology. Chapter 30 presents a detailed overview of heterotaxy and isomerism in the fetus. Figure 6.5: Determining fetal situs: A diagram of the fetus is presented in back posterior ( 1 and 3 ) and back anterior ( 2 and 4 ) positions. In transabdominal scanning, the ultrasound beam (S) is directed from top to bottom. The palm of the right hand represents the face of the fetus, and the fetal heart and stomach are on the same side of the examiner’s thumb. (Modified from Bronshtein M, Gover A, Zimmer EZ. Sonographic definition of the fetal situs. Obstet Gynecol. 2002;99( 6 ):1129–1130, with permission.)
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Fetal Cardiac Measurements and Reference Ranges
- Color Doppler in Fetal Echocardiography
- The Three-Vessel-Trachea View and Upper Mediastinum
- Three- and Four-Dimensional Ultrasound of the Fetal Heart
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What's a sunny-side up baby?

What happens to your baby right after birth

How your twins’ fetal positions affect labor and delivery

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

Where to go next

- DAILY PRACTICE
- IMAIOS DICOM Viewer
- vet-Anatomy
- Breast imaging learning tool
- Blog News, opinions & thoughts of anatomy, medical imaging
Articles talking about IMAIOS and its products
What our users say about us
Our commitments
Get help with your subscription, account and more
- Contact us Other questions?

- Cephalic vein
Vena cephalica
There is no definition for this structure yet
Comparative anatomy in humans
Translations
Cookie preferences
IMAIOS and selected third parties, use cookies or similar technologies, in particular for audience measurement. Cookies allow us to analyze and store information such as the characteristics of your device as well as certain personal data (e.g., IP addresses, navigation, usage or geolocation data, unique identifiers). This data is processed for the following purposes: analysis and improvement of the user experience and/or our content offering, products and services, audience measurement and analysis, interaction with social networks, display of personalized content, performance measurement and content appeal. For more information, see our privacy policy .
You can freely give, refuse or withdraw your consent at any time by accessing our cookie settings tool. If you do not consent to the use of these technologies, we will consider that you also object to any cookie storage based on legitimate interest. You can consent to the use of these technologies by clicking "accept all cookies".
Cookie settings
When you visit IMAIOS, cookies are stored on your browser.
Some of them require your consent. Click on a category of cookies to activate or deactivate it. To benefit from all the features, it’s recommended to keep the different cookie categories activated.
These are cookies that ensure the proper functioning of the website and allow its optimization (detect browsing problems, connect to your IMAIOS account, online payments, debugging and website security). The website cannot function properly without these cookies, which is why they are not subject to your consent.
These cookies are used to measure audience: it allows to generate usage statistics useful for the improvement of the website.
- Google Analytics

IMAGES
VIDEO
COMMENTS
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin. The most common ...
Fetal presentation is a reference to the part of the fetus that is overlying the maternal pelvic inlet. The most common relationship between fetus and mother is the longitudinal lie, cephalic presentation. A breech fetus also is a longitudinal lie, with the fetal buttocks as the presenting part.
The fetus undergoes a series of changes in position, attitude, and presentation during labor. This process is essential for the accomplishment of a vaginal delivery. The presence of a fetal malpresentation or an abnormality of the maternal pelvis can significantly impede the likelihood of a vaginal delivery. The contractile aspect of the uterus ...
The vast majority of fetuses at term are in cephalic presentation. Approximately 5 percent of these fetuses are in a cephalic malpresentation, such as occiput posterior or transverse, face ( figure 1A-B ), or brow ( figure 2) [ 1 ]. Diagnosis and management of face and brow presentations will be reviewed here.
A cephalic presentation or head presentation or head-first presentation is a situation at childbirth where the fetus is in a longitudinal lie and the head enters the pelvis first; the most common form of cephalic presentation is the vertex presentation, where the occiput is the leading part (the part that first enters the birth canal). All other presentations are abnormal (malpresentations ...
Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left. This is called left occiput anterior or right ...
Veterinary anatomy atlas TRAINING. e-MRI MRI step-by-step, interactive course on magnetic resonance imaging QEVLAR App to prepare the Core Exam Breast imaging learning tool App to train reading breast tomosynthesis images COMMUNITY. e-Cases Imaging clinical cases zoo-Paedia
Breech birth is associated with a higher rate of short-term perinatal complications compared to cephalic birth [1,2]. For breech presentation at or near term, there are three options: external cephalic version (ECV), elective cesarean section, or trial of labor in breech (breech TOL). The evidence for the effectiveness of ECV to reduce breech vaginal and cesarean deliveries is strong [3-5 ...
View Cephalic venipuncture & more Canis resources at Vetlexicon. Over 28,000 peer-reviewed resources: Bovis, Equis, Felis, Lapis & Exotis. ... On the veterinary diagnosis and treatment of your choice of species: dogs, cats, rabbits, exotics, horses and cattle. Starting at: £40 /month.
11. CEPHALIC PRESENTATION • vertex or occiput presentation - occipital fontanel is the presenting part • Face presentation - face is foremost in the birth canal; fetal neck may be sharply extended so that the occiput and back come in contact. • • Sinciput presentation- fetal head partially flexed, with the anterior (large) fontanel, or bregma, presenting • Brow presentation -fetal ...
Vertex Presentation. A vertex presentation is the ideal position for a fetus to be in for a vaginal delivery. It means the fetus is head down, headfirst and facing your spine with its chin tucked to its chest. Vertex presentation describes a fetus being head-first or head down in the birth canal.
The meaning of CEPHALIC is of or relating to the head. How to use cephalic in a sentence.
Sagittal section of the pelvis and abdomen in labor with the fetus in cephalic presentation ( a) in posterior asynclitism, ( b) in anterior asynclitism. Palpation of the fetal head sagittal suture during vaginal digital examination, during labor, in left occiput position, transverse, with anterior asynclitism.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord. For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.
Detailed Method to Determine Fetal Situs. 1. Define within the uterus the presentation of the fetus (generally vertex or breech; less often the presentation is oblique or transverse.). 2. Determine whether the fetal spine is parallel or transverse to the maternal spine. In sagittal view, if the fetal and maternal spine are parallel, the fetus ...
Cephalic vein: This is a common site of insertion in lizards and is located running from medial to lateral in a proximal to distal direction across the antebrachium (Fig. 44.3).Using sterile techniques, a superficial transverse cut down, starting from the midmedial antebrachium to lateral, is performed. The vein is superficial; hence, an aggressive skin incision may easily damage the vessel.
Figure 6.2: Determining fetal situs in longitudinal lie: In A, the fetus is in a cephalic presentation with the fetal spine close to the left uterine wall, resulting in the right side being anterior and left side posterior.In B, the fetus is in a cephalic presentation with the fetal spine close to the right uterine wall, resulting in the left side being anterior and right side posterior.
Head first (called vertex or cephalic presentation) Facing backward (occiput anterior position) Spine parallel to mother's spine (longitudinal lie) Neck bent forward with chin tucked. Arms folded across the chest . If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not ...
cephalic presentation: [ prez″en-ta´shun ] that part of the fetus lying over the pelvic inlet; the presenting body part of the fetus. See also position and lie . breech presentation presentation of the fetal buttocks, knees, or feet in labor; the feet may be alongside the buttocks (complete breech presentation); the legs may be extended ...
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. ... This is called an external cephalic version, and it has a 58 percent success rate for turning breech babies. For more information, ...
Veterinary anatomy Cephalic vein Vena cephalica. Definition. There is no definition for this structure yet. Suggest a definition I agree herein to the cession of rights to my contribution in ...
Cephalic fetal presentation (1209182005); Cephalic presentation (1209182005) Definition A fetal position during delivery in which the head of the fetus descends into the maternal pelvis.