

Compassion Fatigue
Secondary Trauma, Vicarious Trauma
Reviewed by Psychology Today Staff
People whose professions lead to prolonged exposure to other people's trauma can be vulnerable to compassion fatigue, also known as secondary or vicarious trauma; they can experience acute symptoms that put their physical and mental health at risk, making them wary of giving and caring.
- Feeling Another’s Pain
- Compassion Fatigue in the General Public
- Treating Compassion Fatigue

Empathy is a valuable trait for the military, first responders, humanitarian aid workers, health care professionals, therapists, advocates for victims of domestic abuse , moderators of offensive online content, and journalists on the front lines of war and disaster. But the more such individuals open themselves up to others' pain, the more likely they will come to share those victims' feelings of heartbreak and devastation. This sapped ability to cope with secondary trauma can lead to total exhaustion of one’s mental and physical state.
Those who regularly experience vicarious trauma often neglect their own self-care and inner life as they struggle with images and stories that can’t be forgotten. Symptoms of compassion fatigue can include exhaustion, disrupted sleep, anxiety , headaches, stomach upset, irritability, numbness, a decreased sense of purpose, emotional disconnection, self-contempt, and difficulties with personal relationships.
Compassion fatigue can affect the most dedicated workers —people who continue to help by working extra shifts or foregoing days off, neglecting their own self-care. This can result from exposure to a single case of trauma, or from years of accumulated “emotional residue."
Burnout is not the same as compassion fatigue. Feeling drained from everyday stressors like work and childrearing results in burnout. Compassion fatigue is the strain of feeling for another’s pain. However, the symptoms are often similar for burnout .
To be more effective, studies have shown, some workers in helping professions may benefit from what’s known as “psychic numbing”—the ability to dial down one’s empathetic instincts while on the job, freeing up cognitive resources to find solutions to the problems in front of them rather than becoming paralyzed by the scope of need they see.
The understanding that exposure to the trauma of others could put people at risk has long been understood—historian Samuel Moyn has said, “Compassion fatigue is as old as compassion,” but the term was coined by historian Carla Joinson in 1992, and further defined and researched by psychologist Charles Figley, who describes it as “a state of exhaustion and dysfunction, biologically, physiologically and emotionally, as a result of prolonged exposure to compassion stress .”

A secondary definition of compassion fatigue refers to the experience of any empathetic individual who is acutely conscious of societal needs but feels helpless to solve them. People who actively engage in charity, or volunteering, may come to feel that they cannot commit any more energy, time, or money to the plight of others because they feel overwhelmed or paralyzed by pleas for support and that the world’s challenges are never-ending.
Evolutionary psychologists studying the development of human empathy suggest that we evolved to put our clan or family first and may struggle to extend our empathy to other groups. Some researchers even argue that empathy can fuel antisocial behavior such as aggression .
Research findings show that people tend to be more responsive to the needs of individuals rather than that of groups, or of the world as a whole. For this reason, charitable organizations have learned to focus their campaigns on how donors can help individual victims, not suffering groups.
Viewing violent news events on television or social media can also cause some people with high levels of empathy to experience symptoms similar to those of secondary trauma.
Soon after a catastrophe, an outpouring of assistance and support is extended to people affected by disaster. However, empathy starts to wear off quickly. This happens because we become fatigued when we are exposed continually to the suffering of others.

Hospitals, nursing and police unions, medical associations, correctional facilities , and other professional groups have become more aware of the effects of secondary trauma and now urge those in the helping professions to offset such fatigue.
We think someone else's problem is theirs, not ours. Yet we are all linked more than we realize. The more we bother to be a good influence in the world, the better the world will be—not just for others, but for us.
You can counteract such fatigue through regular exercise and healthy eating, a commitment to adequate rest and regular time off, and time in therapy . It also helps to set emotional boundaries without barricading yourself from the world.
People experiencing compassion fatigue may secretly self-medicate with alcohol , drugs, gambling, or food. Left unaddressed, compassion fatigue can develop into clinical depression or post- traumatic stress disorder.
Other techniques like mindfulness , meditation or yoga, and time with loved ones or in nature, or devoted to interests or hobbies outside of work have also been found to lessen the symptoms of compassion fatigue.
A 2015 study in the Journal of Continuing Education in Nursing argues for resilience training, a program designed to educate care workers about this type of fatigue and its risk factors. Such training teaches how to employ relaxation techniques and build social support networks to cope with symptoms that arise.

How exhaustion shapes identity, but we can reclaim agency over our lives. We can embrace renewal amidst fatigue.

Ancient wisdom offers a powerful lens for healthcare providers.

The "not good enough" mental narrative and the shameful feeling that comes with it are notable in people who have burnt out. Untamed, they can hinder one's recovery and growth.

What is the "payoff" waiting on the other side of grief and suffering? The most common response is resilience, but research shows it might be compassion.

January is often a time to reflect and set well-being intentions. For those already burnt out, this can be a daunting task. I hope these eight steps will set you up for success.

Burnout is a common problem. Individuals living with depression and anxiety may be at particularly high risk. Preventing burnout is easier than stopping it.
Learn 10 simple ways to charge your battery, avoid burnout, and remain connected to family, friends, colleagues, and patients during the holidays.

Psychotherapy is an incredibly meaningful profession. It draws on compassion and our values. Still, there are hazards of the job, including moral injury.

Seeing one's burnout through the lens of a blessing rather than shame is helpful toward recovery and growth. I share my burnout blessings in the hope it helps you to find yours.

Explore how evolving work cultures and historical contexts shape the current challenges in employee well-being and the multifaceted approach needed to combat burnout.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
Open Access is an initiative that aims to make scientific research freely available to all. To date our community has made over 100 million downloads. It’s based on principles of collaboration, unobstructed discovery, and, most importantly, scientific progression. As PhD students, we found it difficult to access the research we needed, so we decided to create a new Open Access publisher that levels the playing field for scientists across the world. How? By making research easy to access, and puts the academic needs of the researchers before the business interests of publishers.
We are a community of more than 103,000 authors and editors from 3,291 institutions spanning 160 countries, including Nobel Prize winners and some of the world’s most-cited researchers. Publishing on IntechOpen allows authors to earn citations and find new collaborators, meaning more people see your work not only from your own field of study, but from other related fields too.
Brief introduction to this section that descibes Open Access especially from an IntechOpen perspective
Want to get in touch? Contact our London head office or media team here
Our team is growing all the time, so we’re always on the lookout for smart people who want to help us reshape the world of scientific publishing.
Home > Books > Empathy - Advanced Research and Applications
From Empathy to Compassion Fatigue: A Narrative Review of Implications in Healthcare
Submitted: 20 July 2022 Reviewed: 25 August 2022 Published: 18 October 2022
DOI: 10.5772/intechopen.107399
Cite this chapter
There are two ways to cite this chapter:
From the Edited Volume
Empathy - Advanced Research and Applications
Edited by Sara Ventura
To purchase hard copies of this book, please contact the representative in India: CBS Publishers & Distributors Pvt. Ltd. www.cbspd.com | [email protected]
Chapter metrics overview
300 Chapter Downloads
Impact of this chapter
Total Chapter Downloads on intechopen.com
Total Chapter Views on intechopen.com
Evidence is clear regarding the importance of empathy in the development of effective relationships between healthcare professionals (HCPs) and patients in the delivery of successful healthcare. HCPs have pledged to relieve patient suffering, and they value the satisfaction felt from caring for their patients. However, empathy may lead to negative consequences for the empathiser. If there is a personal identification with the emotions of the distressed person, empathic concern may evolve into personal distress leading to compassion fatigue over time. A narrative review was used to explore the connection between empathy and compassion fatigue. A search of MEDLINE, PsychINFO and CINAHL resulted in 141 articles meeting the inclusion criteria. The results included in this chapter explore the practical implications of empathy in relation to compassion fatigue, examining the impact on HCPs as well as the potential risk factors and effective strategies to reduce compassion fatigue. The negative impact of compassion fatigue can have a severe impact on HCP well-being and can in turn impact the care received by the patient. Nevertheless, and despite existing effective strategies to support and manage those experiencing compassion fatigue, more needs to be done to prevent its development in HCPs.
- compassion fatigue
- healthcare profession
secondary traumatic stress
- vicarious trauma
Author Information
Jane graves.
- Western Sydney University, Sydney, Australia
Caroline Joyce
Iman hegazi *.
*Address all correspondence to: [email protected]
1. Introduction
1.1 empathy and compassion in the healthcare profession.
Compassion and respect for human dignity is enshrined in the codes of conduct for healthcare professionals (HCPs). Providing high-quality compassionate care is a fundamental aim of the helping professions and provides them with job satisfaction and a sense of value [ 1 ]. Being treated with compassion also has many patient benefits including increasing compliance with professional advice, improving satisfaction with services and enhancing health and quality of life [ 2 ]. Providing compassionate care requires kindness, empathy, and sensitivity [ 3 ].
Empathy refers to the capacity to understand and share the feelings of others such as pain, joy, fear, and other emotions [ 4 , 5 ]. Historically, emotional responses to patients were seen as threats to objectivity and doctors strived for detachment to be able to care, reliably, for all patients regardless of their personal feelings. Blumgart [ 6 ] recalls Sir William Osler’s “Aequanimitas” in his definition of ‘neutral empathy’ which states that a physician will do what needs to be done without feeling grief, regret, or other difficult emotions. Osler argues that by neutralising their emotions to the point that they feel nothing in response to patient suffering, physicians can ‘see into’ and, thereby, be able to ‘study’ the patient’s ‘inner life’ [ 7 ].
To avoid this conceived conflict between emotions and objectivity, ‘professional empathy’ was defined, on purely ‘cognitive’ basis, as “the act of correctly acknowledging the emotional state of another without experiencing that state oneself” [ 8 ]. This model of ‘detached concern’ assumes that knowing how the patient feels is no different from knowing that the patient is in a certain emotional state. However, the function of empathy is to recognise what it feels like to experience something, not merely to label emotional states [ 9 ]. Halpern [ 9 ] emphasises that patients sense when physicians are ‘emotionally attuned’ and that patients trust ‘emotionally attuned’ physicians and adhere better to their treatment.
In the clinical context, Stepien and Baernstein [ 10 ] combined the different definitions within the literature to put forward an expanded definition of empathy. This proposed definition includes four distinct dimensions: ‘ moral, emotive, cognitive, and behavioural’, all working in harmony to benefit the patient.
1.2 From empathy to compassion fatigue
Empathic perspective-taking is the level of empathy which most psychologists refer to when they speak of ‘empathy’. In this view, empathy is a cognitive state—dependent on imagination and mental attribution—combined with emotional engagement. A major manifestation of empathic perspective-taking is ‘targeted helping’ i.e., help and care based on a cognitive appreciation of the other’s specific need or situation [ 11 ]. The emotional component in providing care and support to people in distress can, over time, deplete the caregiver’s emotional resources engendering ‘compassion fatigue’; which is characterised by feelings of indifference to the suffering of others [ 12 ]. Joinson [ 13 ] in 1992 described compassion fatigue as a form of ‘occupational burnout’ experienced by those in the caring professions. Figley [ 14 ] then described compassion fatigue as ‘caregiver burnout’ and his 2002 model of compassion fatigue emphasised “the costs of caring, empathy, and emotional investment in helping the suffering” [ 15 ]. These ‘costs’ include the increased risk of mental and physical health problems in helping professionals [ 16 , 17 ]. Radey and Figley [ 12 ] suggest, “as our hearts go out to our clients through our sustained compassion, our hearts can give out from fatigue” (p. 207).
Compassion fatigue exists across a diverse range of healthcare professional groups, disciplines, and specialties [ 18 , 19 , 20 ]. Close to 7% of professionals who work with traumatised individuals exhibit emotional reactions that are similar to symptoms of post-traumatic stress disorder (PTSD). This is not only seen in the healthcare sector, where it has been demonstrated in physicians, psychotherapists, and nurses—especially those working with critically ill children, in oncology and in trauma care [ 21 , 22 , 23 , 24 ]—but also, beyond the hospital setting in first responders, emergency teams, social workers, police officers, migration workers, and those working with the homeless [ 25 , 26 , 27 , 28 , 29 ].
Levels of compassion fatigue have increased over the last decade [ 30 ]. More recently, compassion fatigue has become a significant concern during the COVID-19 crisis which has intensified the feelings of burnout, and compassion fatigue in healthcare workers, especially those working in specific COVID-19 units and in emergency departments, leaving no mental space for clinicians to experience authentic clinical empathy [ 31 , 32 , 33 , 34 ]. Recent pooled subscale scores indicate average to high levels compassion fatigue across a diverse healthcare practitioner groups [ 18 ]. For nurses, compassion fatigue rates are currently reported as just above 50% [ 35 ].
2. Aim of this chapter
The aim of this narrative review is to describe and synthesise the literature to explore the associations between empathy and compassion fatigue, and the impact of the latter in the healthcare profession. Also, to examine screening and management strategies of compassion fatigue in HCPs and deduce a conclusion from the evidence.
3. Methodology
We conducted a narrative review using the process described by Green et al. [ 36 ] to present objective conclusions based upon previously published literature that we have comprehensively reviewed. We opted for a narrative overview as narrative reviews can often serve to provoke thought and controversy and may be an excellent venue for presenting philosophical perspectives in a balanced manner [ 36 ].
3.1 Identifying relevant studies
We determined the search strategy through team discussions and pilot explorations of the different databases. We searched MEDLINE (Ovid), APA PsycINFO (EBSCOhost), and CINAHL Plus using the Boolean/Phrase (Empathy AND (‘Compassion Fatigue’ OR ‘Vicarious Trauma’) AND Health). We conducted the search during May and June of 2022 and included literature published between 2003 and 2022, including articles published online ahead of print. Initial search recovered 290 results from MEDLINE, 112 from CINAHL Plus, and 215 from PsycINFO.
3.2 Study selection
EndNote X9 (Clarivate Analytics, Philadelphia, PA, USA) was used to download the bibliographic details of studies yielded from the database searches and duplicates were deleted. Researchers screened article titles and abstracts to determine eligibility for full-text review based on relevance to the research topic. After this initial screening, all researchers read full texts of articles to determine eligibility for inclusion.
Inclusion criteria: The literature review included full text empirical research, which described empathy and compassion fatigue in healthcare workers, published in the English language in academic peer-reviewed journals over the last 20 years.
Exclusion criteria: Studies which covered other forms of vicarious trauma and post-traumatic stress, and studies which explored compassion fatigue in other professions, e.g., police officers, chaplaincy, caregivers, and migration agents, were excluded from this review.
Figure 1 shows a flowchart indicating the search and selection process. Following screening and full-text review, 92 articles were included in this literature review. Subsequent to the full text review, additional related references reported in the 92 examined articles were inspected, and those satisfying the inclusion criteria (n = 49) were also included in this literature review as secondary sources, leading to a total of 141 studies included in this review.

Flow diagram showing records identified from databases and the screening and selection process.
3.3 Collating, summarising, and reporting results
Authors read and objectively evaluated each of the 141 articles. They recorded how each article relates to the objectives of this narrative review. The authors are all HCPs, a chiropractor, psychologist, and a physician. This expertise in the area was useful in interpreting the literature but the authors were careful not to incorporate predispositions or biases by having multiple discussions throughout the review process.
The connection between empathy and compassion fatigue
The impact of compassion fatigue in healthcare
The detection and assessment of compassion fatigue
Management of compassion fatigue in healthcare professionals
HCPs are continually exposed to stressful events in their day-to-day work including frequent encounters with: (a) death and dying, (b) grieving families, (c) personal grief, (d) traumatic stories, (e) observing extreme physical pain in patients, (f) strong emotional states such as anger and depression, and (g) emotional and physical exhaustion [ 37 , 38 , 39 ]. Over time, high levels of stress can lead to burnout [ 39 , 40 ]. Burnout, a much-researched topic in the helping professions, has been defined as “a syndrome composed of emotional exhaustion, depersonalization, and reduction of personal accomplishments” [ 41 ]. Burnout may also lead to negative self-concept, negative attitudes about work, and a loss of caring about work-related issues [ 38 ].
Compassion fatigue, a construct similar to burnout, is a topic that has emerged in the literature in recent years [ 42 , 43 , 44 ]. Radley and Figley [ 12 ] define compassion as a “deep sense or quality of knowing or an awareness [among helping professionals] of the suffering of another coupled with the wish to relieve it” (p. 207). Compassion fatigue, a possible effect of long-term demonstrations of compassion, is defined as “a deep physical, emotional, and spiritual exhaustion accompanied by acute emotional pain” [ 45 ]. Compassion fatigue is thought to be a result of long exposure to the suffering of others, listening to descriptions of traumatic events experienced by others, little to no emotional support in the workplace, and poor self-care [ 12 ].
4.1 The connection between empathy and compassion fatigue
Compassion is an essential component of patient care provided by health professionals [ 46 ]. The care-giving relationship is founded on empathy and a critical characteristic of compassion fatigue is a loss or lack of empathy [ 47 , 48 ].
4.1.1 Temporary lapses in empathy
Temporary lapses in empathy are not uncommon in professional intervention and can have a variety of causes, ranging from experiences in the professional’s own life to reactions to clients’ situation [ 49 , 50 ]. Most clinicians experience them from time to time, and they rarely arouse major distress. There are reports of self-perceived lapses of empathy among emergency workers who provide services in the acute phase of the disaster and psychotherapists engaged in long-term psychotherapeutic relationships that started before and continued during and after the disaster. Many experience the conflict of ‘attention-to-self versus attention-to-client’ as temporary and normal for the situation. Reports by these professionals suggest that their lapses in availability and empathy cause them distress by impairing their self-esteem and fostering feelings of guilt, shame, and inadequacy [ 51 , 52 ].
Baum [ 53 ] suggests that the source of much of the widely reported distress among clinicians is an intra-psychic conflict between two conflicting psychological needs: the need to distance themselves from their clients and their need to raise their self-esteem, especially in experienced professionals whose anxiety is doubly intensified by their prior experiences. Much of the identity and self-esteem of helping professionals is anchored in their ability to be empathic, present, and containing towards those they help. The conflict from the fact that distancing helps the professionals to cope but reduces their ability to empathise with their clients, can lead to feelings of guilt, shame, and self-reproach.
Empathy is seen as comprising affective and cognitive components, whereas compassion is defined in terms of affective and behavioural elements. More specifically, compassion is perceived as comprising both of ‘feelings for’ the person who is suffering and a desire to act to relieve the suffering. The desire to act is distinct from the act itself [ 54 , 55 ].
Compassion fatigue involves a decline in one’s energy, desire, and/or ability to love, nurture, care for, or empathise with another’s suffering [ 56 , 57 , 58 ]. These critical defining attributes were used to develop a theoretical definition: “Compassion fatigue is the physical, emotional, and spiritual result of chronic self-sacrifice and/or prolonged exposure to difficult situations that renders a person unable to love, nurture, care for, or empathize with another’s suffering” [ 59 ].
4.1.2 Compassion fatigue and burnout
Compassion fatigue is strongly correlated with burnout [ 21 , 60 , 61 , 62 ]. Whilst stress and exhaustion are critical attributes of both concepts [ 21 , 60 ] the experience is of being in a ‘tired’ state in burnout and being in a ‘drained’ state in compassion fatigue [ 60 ] and thus devoid of ones resources [ 14 , 60 ].
Wynn [ 60 ] performed a comparative concept analysis examining the terms ‘burnout’ and ‘compassion fatigue’ using Walker and Avant methodology. The ability to recognise both concepts is pivotal in helping to establish strategies that support healthcare workers cope and achieve optimal occupational health. Wynn noted that burnout can be an antecedent of compassion fatigue. The important difference is that burnout as a precursor may be more readily responsive than compassion fatigue to restorative strategies such as time away from the work environment and behaviour modification [ 14 , 60 ]. If not addressed in its early stages compassion fatigue can permanently alter the compassionate ability of the individual [ 63 ]. Thus compassion fatigue may be considered to be a consequence of ongoing burnout in healthcare and indicate a further decline in the wellbeing of the healthcare professional.
The development of compassion fatigue is understood to be a cumulative and progressive process [ 64 ] Whist the development is cumulative, the onset of the experience compassion fatigue for the healthcare worker is a rapid one [ 35 , 65 ]. Comparatively burnout, a larger overarching construct, is experienced as a slowly progressing disorder and is associated with working in burdensome organisational environments [ 65 ]. Thus, in burnout conflict associated with the employer-employee relationship, and in compassion fatigue the conflict is primarily an internal one which is associated with the relationship between the healthcare professional and their patient [ 60 , 66 ].
4.1.3 Vicarious trauma and secondary traumatic stress
Meadors et al. [ 67 ] investigated the relationships between the terms associated with secondary traumatization using a correlational design. They established that there is a significant overlap between compassion fatigue, secondary traumatic stress (STS), and burnout, but that each of the concepts also had significant unexplained variance which suggests that there were differences between the concepts ( Table 1 ).
Definition of compassion fatigue and related terms.
Adapted from [ 67 ].
Secondary traumatization (ST) occurs as a natural consequence of caring between two people: one who has been traumatised and the other who is affected by the first’s traumatic experience [ 70 , 71 ]. Empathy and exposure are central in the development of ST [ 72 ] and can alter the way in which the healthcare worker experiences self, others, and the world [ 73 ].
The potential for ST begins with exposure to a client’s experience that is sufficient to evoke an arousal or emotional response [ 71 , 74 ]. Vulnerability to the client’s experience may be heightened by pre-existing conditions (risk factors) that produce greater sensitivity to the elements in the client’s situation leading to one’s absorption of the suffering itself [ 70 ]. The vicarious experiencing of the feelings, thoughts, or attitudes of another may result in the development of empathy, or the emotional connection that occurs through listening and bearing witness to graphic depictions of traumatic events. While bearing witness to the client’s suffering, the healthcare worker is susceptible to responses or reactions that may be physiological, behavioural, emotional, and/or cognitive in nature. Figley describes this as the “cost of caring” for those in emotional pain [ 71 ]. Alternate discussions such as those by Ledoux contest the notion of a ‘ cost to caring’ and propose that compassion fatigue occurs when ‘ care is obstructed’ [ 54 ].
Osland [ 75 ] reported that dietitians in high-risk workloads reported higher levels of STS than those with low-risk workloads, those in smaller facilities reported higher STS than larger facilities, and that working for >5 years as a dietitian was associated with higher rates of STS and burnout than in those working for <5 years. Those who perceived greater levels of support reported lower rates of burnout and higher rates of compassion satisfaction.
Zeidner et al. [ 47 ] examined the role of some personal and professional factors in compassion fatigue among health-care professionals. Research participants included 182 healthcare professionals who completed an assessment battery measuring compassion fatigue, emotion management, trait emotional intelligence, situation-specific coping strategies, and negative affect. Major findings indicate that self-reported traits ‘emotional intelligence’ and ‘ability-based emotion management’ are inversely associated with compassion fatigue; ‘adaptive coping’ is inversely related to compassion fatigue. Furthermore, problem-focused coping appeared to mediate the association between trait emotional intelligence and compassion fatigue. These findings highlighted the role of emotional factors in compassion fatigue among health-care professionals [ 47 ].
Rayner et al. [ 76 ] examined STS and related factors of empathetic behaviour and trauma caseload among 190 social workers and psychologists. Approximately 30 percent of participants met the criteria for a diagnosis of STS. Results indicated that there was a significant interaction between caseload trauma and personal trauma history on STS. Similarly, empathy alone was not directly related to changes in STS, yet the trauma in caseload effect on STS was moderated by empathy. A personal history of trauma was found to be related to increased levels of STS. However, contrary to expectation of prior research, empathy contributed to a reduction in STS, meaning that lower empathy levels were associated with a higher risk of developing STS.
Hubbard et al. [ 77 ] demonstrated consistency between the five key concepts of ST discussed in the literature, i.e., exposure, vulnerability, empathic engagement, reaction, and transformation. The analysis revealed a dynamic, fluid process in which the energy of the nurse, client, and environment were integrated and part of a diverse whole [ 78 ]. The dynamic nature of the nurses’ experiences created a “kaleidoscope of potentialities” [ 78 ], the outcome of which was either a positive or a negative trajectory. This revealed a new aspect of the dimension of alteration/transformation, which was the identification of a positive outcome during the ST process. These results suggest the importance of further research to assess the role and value of reflective supervision for HCPs and how this may enhance their personal and professional resilience.
4.2 Risk factors for compassion fatigue
Risk factors for the development of compassion fatigue include the intensity of the patient setting as healthcare professionals who care for traumatised individuals in critical care environments are at greater risk of acquiring compassion fatigue [ 20 ]. Engaging with the patients loved ones also places the healthcare professional at risk, particularly if the interactions involve conflict [ 20 ]. Other factors that place the professional at risk including undertaking difficult discussion with patients and families such as breaking bad or uncertain news to patients and their families. A lack of perceived managerial support compounds the risk [ 20 , 65 ] and working more hours perpetuates emotional exhaustion in providers [ 79 ].
Personal factors also appear to play a role in the risk of the development of compassion fatigue. Those who have less experience working as a healthcare professional are at greater risk [ 20 , 80 ] as are those with less maturity [ 80 ] or those who have not acquired a higher level of education or qualification in their profession [ 35 , 46 ].
Poor coping strategies and difficulty with emotional regulation also place providers at greater risk. These include being unable to process feelings in relation to trauma and caring for those who are impacted by suffering [ 20 , 47 ]. Being unable to identify effective coping mechanisms, adapt, manage emotion and develop one’s emotional intelligence [ 20 , 47 ]
There is some indication that one’s personality may also play a role and people with high sensitivity may be more vulnerable to compassion fatigue. People with an increased ability to perceive others feelings may have stronger emotional and physiological reactivity [ 81 ] and thus be more prone to compassion fatigue [ 82 ]. This may be compounded by the contract between the quality of care the healthcare professional may want to provide with what they are actually able to achieve [ 80 ].
Negative life events and pre-existing mental illnesses such as anxiety or depression have been found to increases a person’s susceptibility for compassion fatigue [ 18 ]. Similarly coexisting physical and emotional stress increases levels of existing compassion fatigue [ 80 ].
Certain workplace conditions and events are more likely to trigger the onset of compassion fatigue [ 60 ]. These include continuous and intense contact with patients, exposure to high levels of stress, exposure to suffering and work which requires a high use of self [ 83 ].
4.3 The impact of compassion fatigue
Compassion fatigue negatively impacts the healthcare professional, the patient, the organisation, and the healthcare system [ 19 ].
4.3.1 Impact on the healthcare professional
In order to support patient autonomy healthcare providers practice patient centred care. This care requires genuine engagement and an empathetic approach making exposure to patient trauma and suffering unavoidable for the health care professional [ 79 ].
4.3.1.1 Signs of compassion fatigue
Indicators of compassion fatigue frequently cited in the literature include exhaustion [ 14 , 60 ], reduced capacity for self-care [ 13 , 60 ], ineffective coping, poor judgement [ 83 ], inability to function [ 63 , 83 ], loss of empathy [ 60 , 83 ] and depersonalisation of patients [ 83 ].
4.3.1.1.1 Exhaustion
The experience of the depth of exhaustion has a number of descriptors in the literature. These include a include feelings of weariness [ 63 , 64 ] emptiness, of being drained [ 14 , 60 ] and a ‘profound fatigue of mind and body’ [ 80 ]. People with compassion fatigue feel completely depleted of one’s “biological, psychological, and social resources” [ 14 ] such that they have nothing more to give [ 14 , 60 ]. The individual wants to rest although concerningly rest does not result in increased energy levels or a sense of rejuvenation [ 14 , 60 ]. Individuals may try various attempts to replenish and yet the feeling of exhaustion remains [ 14 , 60 ].
4.3.1.1.2 Reduced capacity for self-care
In 1992 Joinson described compassion fatigue as the reduced capacity to self-care as a result of the sustained fatigue acquired by caring for others [ 13 ]. Recent synthesised descriptions of the experience of compassion fatigue include being left so physically and mentally exhausted and drained by patient care that the provider lacks empathy and is unable to cope [ 60 ].
4.3.1.1.3 Ineffective coping
Ineffective coping is a critical indicator of the occurrence of compassion fatigue [ 13 , 60 ]. When healthcare professionals are no longer able to recover from a depleted state despite using coping strategies the result is ineffective coping [ 60 ]. Coping strategies that may have worked successfully in the past become no longer effective [ 60 ]. Recovery from the stress and exhaustion of providing patient care [ 60 ], is no longer possible. Emotional responses may include feeling emotionally overwhelmed [ 63 , 84 , 85 ] and potentially experiencing an emotional breakdown [ 15 , 20 , 63 ].
4.3.1.1.4 Inability to function
Inability to function may be experienced as a diminished ability [ 15 ] or reduced endurance and output [ 63 , 83 ], leading to a diminished or ineffective work performance [ 13 , 63 , 83 ]. The experience of trauma-based symptoms, in addition to significant exhaustion results in a deterioration of function [ 63 ]. The compassionate energy required to care for patients has been consumed over time is distinguished beyond the point of possible replenishment. An inability to compassionately care for patients moves beyond the work environment and leads to an inability to function which impacts all aspects of the professionals life [ 63 ].
4.3.1.1.5 Loss of empathy
Whilst attempting to employ coping strategies to manage the stress of caregiving a loss of empathy occurs. In response to the relentless overwhelming stress and resultant exhaustion of care-giving a deep psychological shift occurs [ 60 , 86 ]. Health professionals lose their sensitivity to and understanding of the patient’s needs. The professional is no longer able to comprehend the patient’s perspectives or recognise their thoughts and feelings [ 60 , 86 ]. Thus patient experiences are no longer relatable and the health professional experiences compassion fatigue [ 60 , 86 ]. Factors that inhibit sustained energy and perpetuate compassion fatigue include time constraints, burnout [ 87 ] and caring for high-stakes patients [ 60 ]. Health professionals with their own personal history of trauma are also at greater risk of acquiring compassion fatigue [ 88 ] due to their sensitivity to secondary traumatic stress [ 76 ]. As a consequence of their empathy loss, the healthcare professional appears indifferent [ 14 , 15 ], unresponsive [ 63 ], callous [ 15 , 84 , 89 ] and unable to share in or alleviate the patients suffering [ 15 ].
4.3.1.1.6 Depersonalisation
Depersonalisation is a sense of detachment from oneself in which individuals perform tasks in a robotic fashion without emotion. It presents as a coping mechanism used to manage exhaustion [ 90 ] and to avoid the feelings of distress that may arise when a person is experiencing compassion fatigue. Whilst the response does not arise from a lack of empathy for the patient [ 60 ] the depersonalisation coping mechanism once triggered in the professional results in a lack human feelings or emotions in the work place. Consequently, this translates to a lack of human feelings in how the professional provides care, which results in substandard care [ 83 ]. The serious implications of depersonalisation in healthcare professionals arises when the lack of emotion in self, results in the professional viewing the patient as also inert or an ‘object’ and approaches the patient with an attitude of indifference [ 90 ].
Depersonalisation is a maladaptive coping mechanism seen in both burnout and compassion fatigue and occurs when individuals detach from their feelings and emotions in order to be able to function and complete work-related tasks [ 60 ]. Yet the severity of depersonalisation experienced in compassion fatigue leads the provider to view the patient as an ‘object’ [ 90 ] and the provider is no longer able to respond to the humanity within the patient. This emotionally dissociated approach sharply contrasts with anticipated patient expectations.
4.3.1.2 Symptoms of compassion fatigue
Compassion fatigue is a significant risk factor for well-being [ 20 , 25 ]. Compassion fatigue impacts ones physical and mental health [ 63 , 64 ] and leading to an array of potentiation indicators including psychological, physical, spiritual, and social symptoms [ 86 ]. As the condition progresses the professional experiences an increase in the scope and severity of symptoms [ 63 ]. For example the individual may experience physical symptoms of burnout, reduced work performance and physical complaints, the intellectual effects of impaired concentration, emotional effects of breakdown, the social symptoms of indifference towards patients and desire to quit, the spiritual effects of disinterest in introspection and dysfunctional coping behaviours [ 63 ].
4.3.1.2.1 Physical symptoms
Physical symptoms may include health complaints, intellectual effects and fatigue [ 15 , 63 ]. Health complaints may include gastrointestinal conditions and stomach pain, and headaches, including migraine [ 20 , 83 , 91 ]. Sleep disturbance is frequently cited [ 20 , 65 , 91 , 92 ] and people may be at greater risk of accidents [ 15 , 83 ]. Intellectual effects include impaired ability to concentrate [ 13 , 14 , 15 , 63 ], poor judgement [ 20 ] and disorganisation [ 63 , 89 ]. Fatigue may manifest as weariness [ 63 , 85 ] lack of energy [ 13 , 15 , 63 , 85 , 89 ] loss of strength [ 63 , 85 ] loss of endurance [ 63 , 85 ] and power of physical recovery [ 63 ] Complications of fatigue include weight gain or weight loss [ 83 ].
4.3.1.2.2 Psychological impact
The psychological impact of compassion fatigue is well established in the literature and manifests as stress, burnout [ 13 ], intrusive and pervasive thoughts [ 65 , 91 ] anxiety [ 13 , 63 , 64 ], and depression [ 13 , 20 , 60 , 63 , 64 , 65 ]. Compassion fatigue has been found to have a moderate correlation with anxiety and depression [ 93 ].
4.3.1.2.3 Emotional impact
The emotional impact of a loss of compassion is typically one of devastation for those in healthcare professions [ 13 ]. Compassion for others drives workplace motivation to serve and alleviate suffering [ 54 ]. People in nurturing roles are rewarded for putting others needs ahead of their own [ 13 ], and ethically a drive to nurture others connects with the ideal archetype of those in caring professions and a societal sense of social justice [ 54 ].
Emotional exhaustion and its consequential impact on one’s personal life are the most frequently reported emotional effects of compassion fatigue [ 20 , 94 ]. A person’s capacity to communicate with others is impaired and this extended into personal relationships. Individuals feel emotionally distressed or bereft and may well experience an emotional breakdown [ 15 , 60 , 63 , 65 , 80 , 83 ].
Indicators of compassion fatigue may include fluctuations in emotional states [ 91 , 92 ] or mood swings [ 20 ]. Impacted healthcare professionals may feel emotionally overwhelmed [ 63 , 84 , 85 ], irritable [ 14 , 20 , 63 , 64 ] angry, fearful, out of control [ 13 ]. or apathetic [ 13 , 63 , 84 ]. Ones outlook is likely to become negative [ 60 ] and people experience ‘work related dreads’. [ 91 ] Healthcare professionals are no longer able to feel empathy for those in their care or respond compassionately. They have an inability to share in, or alleviate suffering [ 15 ] and may respond with indifference [ 14 , 15 ], callousness [ 15 , 84 , 89 ] or be unresponsiveness [ 63 ] to patients at times when they previously would have been empathetic.
Spiritual effects include a lack of spiritual awareness and disinterest in introspection [ 15 , 63 , 85 ] which has the potential to result in poor judgement [ 15 , 63 ] cynical humour and dysfunctional coping behaviours such an increased consumption of alcohol, unhealthy food or pornography [ 91 ]. The impact is a loss of self-worth [ 95 ] which may be compounded by weight gain or loss [ 83 ] and its emotional impact.
4.3.2 The impact of compassion fatigue on patients
Patient care is negatively impacted by compassion fatigue and this impact is recognisable to patients. Health professionals effected by compassion fatigue experience a decreased ability to feel empathy and hence lack meaning in their work [ 20 , 96 ]. which results in substandard care [ 20 , 83 , 96 ]. The stress of the working environment is palpable to patients and is identifiable as a consequence of poor-quality care [ 60 , 97 ]. Patients depend on health professionals to alleviate the stress, anxiety and fear associated with their illness [ 90 ]. When patients sense the impact of compassion fatigue they question the quality and appropriateness of care which in turn escalates patient stress [ 60 ].
The relationship between the healthcare professional and the patient becomes compromised. The trauma response associated with compassion fatigue results in reduced or decreased workplace engagement [ 21 ] and avoidance of particular situations or patients [ 96 ]. The ultimate consequence of compassion fatigue and burnout is poor patient outcomes [ 60 ]. Indeed significant concerns arise regarding the potential for increased medical errors and patient safety [ 21 , 64 , 83 ].
4.3.3 The impact of compassion fatigue on organisations and the healthcare system
Staff who are experiencing compassion fatigue have reduced job satisfaction [ 21 ] and reduced efficiency levels resulting in reduced service quality [ 98 ]. Patient satisfaction levels are lower in institutions where job satisfaction and burnout levels are reduced [ 97 ]. Poor patient satisfaction levels result in reduced patient recommendation rates of same facility to family and friends [ 60 , 97 ].
Relationships with co-workers become negatively impacted [ 20 , 96 ] when a person is impacted by compassion fatigue. If working with colleagues who are equally exhausted and apathic [ 13 ] productivity and workplace morale decline [ 95 ]. The result is a poor work environment with lower levels of productivity, patient satisfaction and patient care outcomes [ 21 ]. Compassion fatigue is triggered by the ongoing use of empathy while caring for those who are suffering and the effect of a poor work environment [ 18 , 99 ]. Thus, the cycle of compassion fatigue perpetuates.
As staff fatigue, the rates of sick leave increase [ 83 ]. More staff members experience an intensifying desire to leave their workplace, profession [ 15 , 24 , 60 ] and specialty [ 80 ]. Compassion fatigue and burnout result in workplace imbalances [ 24 , 60 ] with higher rates of staff turnover [ 95 ], and attrition and eventually, workforce dropout [ 98 ]. Staff turnover rates are particularly volatile in in high-stakes environments [ 100 ] such as oncology and emergency medicine. Staff seek alternate employment opportunities in an attempt to combat excessive workplace stress. As turnover rates increase, the stress in the workplace intensifies as remaining staff attempt to continue short staffed [ 60 ].
Compounding the impact of compassion fatigue is the perception that indicators of a poor working environment, such as increased rates of absenteeism, reduced service quality, low levels of efficiency are being ignored by the organisation and healthcare system [ 18 , 98 ]. Concerns include the conclusion by staff that administrators do not consider caregiver stress when allocating tasks [ 13 ]. The impact of compassion fatigue is intensified when management fail to provide workplace acknowledgement, fail to provide opportunities for peer support and appear not to value work-life balance [ 80 ]. When the workplace culture is not addressed with opportunity for employee training, and a shift towards a compassionate organisational culture [ 65 ] staff in healthcare will continue to experience moderate to high levels of compassion fatigue.
As a consequence of the negative impact on productivity, job satisfaction and staff turnover, compassion fatigue also impedes workplace focus on patient safety [ 21 ] and thus has the potential to lead to an increase in medical errors and diminished patient outcomes [ 21 ]. Healthcare professionals experiencing burnout and compassion fatigue are more prone to medical error [ 83 ] as a result of compassion fatigue symptoms including exhaustion [ 14 , 60 ] and a diminished work performance [ 13 , 63 , 83 ].
In addition to the potential harm to patients and families, compassion fatigue related medical error has the potential to result in legal, reputational and economic loss, for individual healthcare providers [ 101 ]. The economic impact of an institution impacted by compassion fatigue staff turnover, patient dissatisfaction and concerns regarding medical error and patient safety is institutional financial loss [ 64 , 102 , 103 , 104 ]. Compassion is valued by patients and healthcare professionals alike and both patients and professionals raise concerns regarding a widespread and escalating lack of compassion in healthcare systems [ 30 , 101 ].
4.4 Detection and assessment of compassion fatigue
Compassion fatigue is commonly measured using the Professional Quality of Life Scale (ProQOL) [ 105 , 106 ]. The self-score scale is a freely available to measure the negative and positive effects of caring and helping others who have experiences significant trauma or suffering.
The Compassion Fatigue Self-Test (CFST) was originally developed to measure compassion fatigue [ 107 ]. The CFST measures the level of risk of an individual to developing compassion fatigue. The scale included 40 items, divided into two subscales, compassion fatigue and job burnout; 23 items measure compassion fatigue and 17 items burnout. Using a five-point scale, respondents are asked to indicate how frequently a situation or particular characteristic is true of themselves (1 = rarely/never, 2 = at times, 3 = not sure, 4 = often, 5 = very often). On the subscale compassion fatigue, scores of 26 or below, indicate being at an extremely low risk, a score between 27 and 30, low risk, between 31 and 35 moderate risk, scores between 36 and 40 high risk and scores between 41 and above, indicate an extreme high risk of compassion fatigue. Scores on the subscale for burnout below 36 indicated an extremely low risk, between 37 and 50 moderate risk, 51–75 indicates high risk, and scores between 76 and 85 indicated an extremely high risk of burnout. The reported internal consistency alphas are reported to be between .86 to .94 [ 108 ]. The scale has been widely used in a variety of settings and has adequate reliability and validity [ 69 ]. The measure was specifically developed to measure both direct and indirect trauma making it a widely applied measure [ 108 ].
The CFST scale was revised and re-developed [ 106 ] into the Professional Quality of Life (ProQOL). The revised scale included an additional subscale to measure compassion satisfaction. The three subscales total 30 items, using a six-point scale (0 = never, 1 = rarely, 2 = a few times, 3 = somewhat, 4 = often, 5 = very often). Respondents are asked about their thoughts, feelings and behaviour at work. The first of the three sub-scales measures compassion satisfaction, a higher score on this scale represents a greater satisfaction as a caregiver and helping others. The second subscale, measures burnout and feelings of hopelessness at not being able to do a good job, and the third subscale measures compassion fatigue/secondary traumatic stress. A higher score on this subscale represents high levels of compassion fatigue/secondary traumatic stress. Each subscale includes 10 items, and the subscale scores cannot be combined to calculate a total score. The ProQOL scale improved on the psychometric properties of the CFST scale [ 105 , 106 ]. The scale with the additional subscale measuring compassion satisfaction incorporates the more positive and psychologically protective aspect of caring, capturing the rewarding and gratifying aspects of caring [ 105 , 106 ]. The Cronbach’s α values reported by Stamm for these scales were .82 for compassion satisfaction, .71 for burnout, and .78 for compassion fatigue [ 105 ]. The ProQOL is free to use and is readily available, as are guidelines for interpreting the results from the scale.
4.5 Management of compassion fatigue in healthcare professionals
Figley [ 70 ] believed to manage compassion fatigue in health professional a multifaceted approach is required that includes prevention, assessment and minimising the consequences. The impacts of compassion fatigue are far reaching for both the individual health professional and organisations. Helping protect healthcare professionals from developing compassion fatigue and managing those experiencing high levels of job burnout and secondary traumatic stress can be done through self-care, evidence-based interventions and creating organisations that are better able to support and protect their workers. By protecting health professionals ensures high quality patient care. Over the past few decades’ interventions have been developed to help reduce symptoms of compassion fatigue. Self-care techniques that can be used to help reduce the risk of developing compassion fatigues and managing the risks of providing compassionate care to patients and clients have been developed and promoted among health care professionals. Organisations also play a role in helping reduce the risk to their workers through better training, ongoing support and creating a support environment that recognises the risks to their staff.
4.5.1 Interventions for compassion fatigue
Interventions have been developed to both prevent and manage compassion fatigue in healthcare professionals. The strategies have included education interventions and developing skills such as resilience [ 109 ]. The Accelerated Recovery Program (ARP) is a program developed to reduce compassion fatigue, including secondary traumatic stress and burnout in healthcare professionals. The ARP was originally developed in 1997 [ 110 ], based on Figley’s work on compassion fatigue (1995). The main aim of the program is to build resilience skills to prevent compassion fatigue. The program duration is 5 weeks, consisting of a weekly 90–120-minute training sessions. A full assessment is undertaken in the first session, along with a discussion exploring the symptoms participants are experiencing. In the second session treatment goals and a timeline is discussed using self-visualisation techniques. The third session focuses on reframing and reprocessing the trauma experienced using eye movement desensitisation and reprocessing therapy and reviewing self-regulation strategies for managing situations. The fourth session incorporates video-dialogue techniques to enable the individuals to supervise themselves through the development of externalisation techniques. In the final session, closure and aftercare are addressed with the use of Pathways to recovery that include skill acquisition; self-care; connection with others; and internal conflict resolution. The program works by developing a person’s self-awareness of compassion fatigue and practicing regular self-care activities [ 110 ]. The ARP primarily focused on mental health and trauma workers [ 110 ] but its potential to be effective in reducing compassion fatigue among nurses and other healthcare profession is growing [ 24 ]. Evidence supports the use of the ARP to reduce compassion fatigue among health care professionals [ 24 , 111 , 112 ]. An adaptation of the ARP that reduced the training into a single four-hour session reported a similar significant reduction in compassion fatigue [ 113 ].
The Compassion Fatigue Resiliency program (CFRP) was based on the concepts of the ACP [ 110 ]. The program is a five-week formalised program to educate participants about compassion fatigue, the factors that contribute to it and the effects of chronic stress. The program interventions aim to reduce the effects of compassion fatigue with participants taking part in small group activities that allow them to build resilience through self-regulation, intentionality, self-validation, connection and self-care.
Evidence supports the effectiveness of the CRRP to reduce secondary traumatic stress by providing nurses with the ability to manage intrusive thoughts [ 24 ]. The program aids greater relaxation enabling individuals to better manage perceive threats, enabling them to manage chronic stress through self-regulation [ 114 ]. The benefits of the CFRP have been reported for healthcare providers in reducing the symptoms of compassion fatigue [ 115 , 116 , 117 ].
To improve the resilience of military healthcare professionals and reduce compassion fatigue the Army’s Care Provider Support Program (CPSP) was developed. During one-hour sessions, healthcare providers are educated to be able to assess themselves for compassion fatigue and identify when they need to take action. The program activities focus on developing self-awareness through group discussion and interactive participation, along with providing education on stress and resilience. Support for the intervention significantly reducing burnout was demonstrated by Weidleich et al. [ 118 ]. However, although a decrease in secondary trauma was reported this was not significant [ 118 ].
Overall, the usefulness of formal intervention programs developed to target reducing compassion fatigue have been reported in a number of healthcare professionals. Although, there is only limited evidence to support the effectiveness of the CPSP. Despite the evidence to support the use of these intervention programs provided in this section, due to the nature of health care settings it is not always practical or cost effective to run these programs for staff. Staff would be expected to attend these programs in their own time and the financial impact to organisations with other competing costs make these types of interventions unfeasible.
4.5.2 Self-care
Organisational resources may not be available or sufficient to address compassion fatigue in employees, therefore promoting self-care can be an effective way to support staff. Self-care interventions are commonly prescribed for health professions experiencing compassion fatigue. Successfully managing compassion fatigue can be done by developing strategies that enhance awareness and provide thoughtful self-care [ 119 ]. There are numerous self-care strategies that can be adopted and utilised by healthcare professionals.
Strategies and techniques that can be used to reduce the risk of compassion fatigue involve looking after general wellbeing, including diet, exercise and sleep. Evidence supports maintaining a healthy diet and getting the recommended amount of physical exercise help regulates mood [ 120 ] and reduce the risk of compassion fatigue [ 121 ]. Regular sleep also plays an important role in regulating mood. Sleep deprivation is associated with decrease cognitive performance and increases the risk of low mood such as anxiety and anger [ 122 ].
Nurturing the self can be done using a number of different techniques. Developing and practicing self-compassion can increase a person psychological wellbeing and assist professionals to better respond to the difficulties experienced in their jobs [ 123 , 124 ]. Self-care interventions developed aim to help healthcare professionals achieve work-life balance by developing coping skills to maintain both emotional and physical health [ 125 ], along with maintaining healthy social networks and participating in activities to promote relaxation such as meditation and mindfulness [ 126 , 127 ]. Other self-care activities that can be adopted to help to support emotional wellbeing involve creative writing [ 128 ]. Strategies have included the use of writing poems to explore difficulties with emotional connection [ 129 ], or the use of creative cafes to reaffirm the core values involved in nursing [ 130 ].
4.5.3 Peer support programs
Peer support programs can be effective strategies to support healthcare professionals to help mitigate compassion fatigue. Encouraging individuals to utilise their social support networks has a protective quality, by providing opportunities to process traumatic experiences at work [ 131 ]. Chambers [ 132 ] developed the Care for Caregivers program for physicians, nurses and other frontline staff. The staff were trained in peer support techniques that covered active listening, normalising emotions, reframing situations, sharing stories and offering ideas of coping mechanisms. The program was reported as being well utilised by staff members, especially those dealing with patients experiencing trauma or patient death. Within 2 years of the program running staff surveys reported an increase in feeling adequately supported by the hospital from 16% to 86%, helping change the workplace culture to being more emphatic [ 132 ].
4.5.4 Protection through training
Preventing healthcare from the risks of developing compassion fatigue can be included in training programs. There are ways in training healthcare professionals to equipped them with strategies to help protect them from developing compassion fatigue. For example, trauma therapists utilising evidence-base practices when treating their clients had significantly decreased amounts of compassion fatigue and burnout compared to specialists not using evidence-based practices [ 133 ]. This demonstrates the use of evidence-based practices to prevent the negative outcomes of compassion fatigue therefore improving both the therapists and clients experience of therapy [ 133 , 134 ]. A study by Deighton [ 135 ] reported the exposure to the clients traumatic event was not as important in therapists developing compassion fatigue as the therapist’s t ability to help the client work through their trauma [ 135 ]. Being able to identify possible strategies to be better equipped to deal with exposure to clients’ traumas can reduce the impact on healthcare professionals.
4.5.5 Culture change in healthcare facilities
Organisations can help mitigate the effects of compassion fatigue experienced by their employees. Organisations need to assess whether and to what extent compassion fatigue is a concern of their workers to be able to start to address the problem [ 136 ]. Prevention is recommended as the first line of defence against compassion fatigue [ 137 ]. Organisations should provide regular education and training around the importance of building employees self-care routines [ 138 ]. The Hospital, University Pennsylvania, is an example of an organisation that has provided their own wellness programs to support their staff. A Centre for Nursing Renewal was developed to minimise the ill effects of compassion fatigue and promote wellness among its staff [ 139 ]. The centre offered relaxation, meditation, yoga, group exercise classes, along with other classes and spaces to support nurses emotional and physical wellbeing. The centre assisted in creating a culture where nurse leaders were increasing awareness of nurses experiencing compassion fatigue and burnout and could therefore encourage staff to engage in discussion and renewal practices such as exercise, talking, reflection and getting adequate rest [ 139 ].
Staff wellness programs and initiatives have been implemented and trialled in other health care providers organisations. These programs range in the types of resources provided, include from professional counselling, employee health screening, role modelling, mentor program, o providing healthy snacks and relaxation. These types of programs offered by organisations and led by trained professional can help reduce compassion fatigue [ 119 , 128 ]. These include employee health screening, role modelling, mentor program and staff retreats.
Staff wellness programs and initiatives have been implemented and trialled in other organisations. These programs range in the types of resources provided and included professional counselling, employee health screening, role modelling, mentor program, staff retreats, providing healthy snacks and relaxation. These types of programs were offered by organisations and led by trained professional can help reduce compassion fatigue [ 116 , 125 ].
More practical strategies that could be provided from an organisational level include providing adequate staffing levels, having good leadership support and experienced staff [ 140 ]. By creating workplaces where it is encouraged to acknowledge that providing emphatic care to patients in difficult situations can cause compassion fatigue is a response of caring, can help to address the phenomenon [ 66 ]. At an organisational level demonstrating compassion is genuinely appreciated through celebrating staff acts of compassion [ 136 ] can help make staff feel valued and supported. Providing staff with personal development opportunities promoting psychological wellbeing [ 141 ], along with debriefing after stressful events could promote healing [ 140 ]. Organisations can play a major role in supporting staff provide the best patients care in a safe and nurturing environment.
5. Limitations of this review
While every attempt was made to search the appropriate databases for articles systematically, it is important to note that this is not a systematic review. The search was limited to three major databases: MEDLINE (Ovid), APA PsycINFO (EBSCOhost), and CINAHL Plus using the Boolean/Phrase (Empathy AND (“Compassion Fatigue” OR “Vicarious Trauma”) AND Health). Two main limitations influenced the studies identified by the database search; the first was not including the term “Secondary Traumatic Stress” as an alternative to “Vicarious Trauma” in the search terms, and the second was limiting the search to literature published between 2003 and 2022 and missing essential articles published in the 90s. These dates were initially selected due to the escalation in volume of relevant publications during that timeframe. Fortunately, these limitations were identified by the authors during the review process and were corrected by including all relevant secondary sources which retrieved the essential articles before 2003 in addition to studies examining Secondary Traumatic Stress.
6. Conclusion
Empathy and compassion are fundamental aspirations for HCPs as they provide them with job satisfaction, a sense of value, as well as greatly benefiting their patients. However, caring and supporting people in distress can, over time, lead to compassion fatigue which negatively impacts the healthcare professional, the patient, the organisation, and the healthcare system. Although there are clear risk factors, identifying tools and effective strategies to support and manage those experiencing compassion fatigue, compassion fatigue in HCPs continues to grow reaching alarming levels over the last decade. Further research is needed to quantify the escalation and impact of compassion fatigue, and in a broader array of healthcare professionals. Exploration of the unique impact of loss of compassion beyond the experience of burnout is also an area requiring an enhanced understanding.
We propose that organisations implement regular screening and targeted support for at-risk individuals. More practical strategies could be provided from an organisational level to prevent the development of compassion fatigue in HCPs and support staff to provide the best patient care in a safe and nurturing environment. Ensuring a positive work culture, which includes peer support programs, is a managerial responsibility. Evidence supports the use of formal intervention programs such as CFRP and the ARP to be effective in reducing compassion fatigue, yet these programs required the HCP to commit a substantial amount of time, usually outside of their working day. For the benefits of these programs to reach HCP, shorter programs preferably accessible during work hours could be incorporated. Future research should focus on identifying components of these programs that could be adapted into modified shorter training sessions that could become part of ongoing professional development.
Crucially, we propose that ensuring adequate staffing levels be a key responsibility of management and, therefore, we advise the meticulous implementation of quality assurance, evaluation, and formal reporting of staffing ratios.
Acknowledgments
This study was supported by the School of Medicine at University of Western Sydney University, Australia.
Conflict of interest
The authors declare no conflict of interest.
A special thank you to the medical librarians at Western Sydney University for their literature search and Endnote support.
Nomenclature and abbreviations
healthcare professionals or providers
post-traumatic stress disorder
secondary traumatization
- 1. Roney LN, Acri MC. The cost of caring: An exploration of compassion fatigue, compassion satisfaction, and job satisfaction in pediatric nurses. Journal of Pediatric Nursing. 2018; 40 :74-80
- 2. Kinman G, Grant L. Enhancing empathy in the helping professions. In: Psychology and neurobiology of empathy. Nova Biomedical Books; 2016. pp. 297-319
- 3. Cole-King A, Gilbert P. Compassionate care: The theory and the reality. Journal of Holistic Healthcare. 2011; 8 (3):30
- 4. Hein G, Singer T. I feel how you feel but not always: The empathic brain and its modulation. Current Opinion in Neurobiology. 2008; 18 (2):153-158
- 5. Hoffman ML. Chapter 4—Varieties of empathy-based guilt. In: Bybee J, editor. Guilt and Children. San Diego: Academic Press; 1998. pp. 91-112
- 6. Blumgart HL. Caring for the patient. The New England Journal of Medicine. 1964; 270 :449-456
- 7. Osler W. Aequanimitas: With Other Addresses to Medical Students, Nurses and Practitioners of Medicine. Philadelphia: P. Blakiston's Son & Co.; 1920. p. 475
- 8. Markakis K, Frankel R, Beckman H, Suchman A. Teaching empathy: It can be done. Annual Meeting of the Society of General Internal Medicine; April 29–May 1; San Francisco, California. 1999
- 9. Halpern J. What is clinical empathy? Journal of General Internal Medicine. 2003; 18 (8):670-674
- 10. Stepien KA, Baernstein A. Educating for empathy. A review. Journal of General Internal Medicine. 2006; 21 (5):524-530
- 11. de Waal FB. The antiquity of empathy. Science. 2012; 336 (6083):874-876
- 12. Radey M, Figley CR. The social psychology of compassion. Clinical Social Work Journal. 2007; 35 (3):207-214
- 13. Joinson C. Coping with compassion fatigue. Nursing (Jenkintown, Pa). 1992; 22 (4):116-121
- 14. Figley CR. Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in those Who Treat the Traumatized. New York: Brunner/Mazel; 1995
- 15. Figley CR. Compassion fatigue: Psychotherapists' chronic lack of self care. Journal of Clinical Psychology. 2002; 4 (11):1433-1441
- 16. Adams RE, Boscarino JA, Figley CR. Compassion fatigue and psychological distress among social workers: A validation study. American Journal of Orthopsychiatry. 2006; 76 (1):103-108
- 17. Bourassa DB. Compassion fatigue and the adult protective services social worker. Journal of Gerontological Social Work. 2009; 52 (3):215-229
- 18. Cavanagh N, Cockett G, Heinrich C, Doig L, Fiest K, Guichon JR, et al. Compassion fatigue in healthcare providers: A systematic review and meta-analysis. Nursing Ethics. 2020; 27 (3):639-665
- 19. Peters E. Compassion fatigue in nursing: A concept analysis. Nursing Forum (Hillsdale). 2018; 53 (4):466-480
- 20. Sorenson C, Bolick B, Wright K, Hamilton R. Understanding compassion fatigue in healthcare providers: A review of current literature. Journal of Nursing Scholarship. 2016; 48 (5):456-465
- 21. Bleazard M. Compassion fatigue in nurses caring for medically complex children. Journal of Hospice and Palliative Nursing: JHPN: The Official Journal of the Hospice and Palliative Nurses Association. 2020; 22 (6):473-478
- 22. Osofsky JD. Perspectives on helping traumatized infants, young children, and their families. Infant Mental Health Journal. 2009; 30 (6):673-677
- 23. Katz A. Compassion in practice: Difficult conversations in oncology nursing. Canadian Oncology Nursing Journal. 2019; 29 (4):255-257
- 24. Potter P, Deshields T, Berger JA, Clarke M, Olsen S, Chen L. Evaluation of a compassion fatigue resiliency program for oncology nurses. Oncology Nursing Forum. 2013; 40 (2):180-187
- 25. Kinman G, Grant L. Emotional demands, compassion and mental health in social workers. Occupational Medicine. 2020; 70 (2):89-94
- 26. Lemieux-Cumberlege A, Taylor EP. An exploratory study on the factors affecting the mental health and well-being of frontline workers in homeless services. Health & Social Care in the Community. 2019; 27 (4):e367-ee78
- 27. Pietrantoni L, Prati G. Resilience among first responders. African Health Sciences. 2008; 8 (Suppl. 1):S14-S20
- 28. Tehrani N. Compassion fatigue: Experiences in occupational health, human resources, counselling and police. Occupational Medicine. 2010; 60 (2):133-138
- 29. Turgoose D, Glover N, Barker C, Maddox L. Empathy, compassion fatigue, and burnout in police officers working with rape victims. Traumatology. 2017; 23 (2):205-213
- 30. Xie W, Chen L, Feng F, Okoli CTC, Tang P, Zeng L, et al. The prevalence of compassion satisfaction and compassion fatigue among nurses: A systematic review and meta-analysis. International Journal of Nursing Studies. 2021; 120 :103973
- 31. Anzaldua A, Halpern J. Can clinical empathy survive? Distress, burnout, and malignant duty in the age of Covid-19. Hastings Center Report. 2021; 51 (1):22-27
- 32. Becker J, Dickerman M. Impact of narrative medicine curriculum on burnout in pediatric critical care trainees. Critical Care Medicine. 2021; 49 (1 Suppl. 1):473
- 33. Carver ML. Another look at compassion fatigue. Journal of Christian Nursing: A Quarterly Publication of Nurses Christian Fellowship. 2021; 38 (3):E25-EE7
- 34. Ruiz-Fernández MD, Ramos-Pichardo JD, Ibáñez-Masero O, Cabrera-Troya J, Carmona-Rega MI, Ortega-Galán ÁM. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. Journal of Clinical Nursing. 2020; 29 (21-22):4321-4330
- 35. Zhang YY, Han WL, Qin W, Yin HX, Zhang CF, Kong C, et al. Extent of compassion satisfaction, compassion fatigue and burnout in nursing: A meta-analysis. Journal of Nursing Management. 2018; 26 (7):810-819
- 36. Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: Secrets of the trade. Journal of Chiropractic Medicine. 2006; 5 (3):101-117
- 37. DiTullio M, MacDonald D. The struggle for the soul of hospice: Stress, coping, and change among hospice workers. American Journal of Hospice and Palliative Medicine®. 1999; 16 (5):641-655
- 38. Keidel GC. Burnout and compassion fatigue among hospice caregivers. American Journal of Hospice and Palliative Medicine®. 2002; 19 (3):200-205
- 39. Payne N. Occupational stressors and coping as determinants of burnout in female hospice nurses. Journal of Advanced Nursing. 2001; 33 (3):396-405
- 40. O'Halloran TM, Linton JM. Stress on the job: Self-care resources for counselors. Journal of Mental Health Counseling. 2000; 22 (4):354
- 41. Jenaro C, Flores N, Arias B. Burnout and coping in human service practitioners. Professional Psychology: Research and Practice. 2007; 38 (1):80
- 42. Bride BE, Figley CR. The fatigue of compassionate social workers: An introduction to the special issue on compassion fatigue. Clinical Social Work Journal. 2007; 35 (3):151-153
- 43. Figley CR. Compassion Fatigue: Toward a New Understanding of the Costs of Caring. Philadelphia, PA, US: Brunner/Mazel; 1995
- 44. Rourke MT. Compassion Fatigue in Pediatric Palliative Care Providers. Pediatric Clinics of North America. 2007; 54 (5):631-644
- 45. Pfifferling J-H, Gilley K. Overcoming compassion fatigue. Family Practice Management. 2000; 7 (4):39
- 46. Arkan B, Yılmaz D, Düzgün F. Determination of compassion levels of nurses working at a university hospital. Journal of Religion and Health. 2020; 59 (1):29-39
- 47. Zeidner M, Hadar D, Matthews G, Roberts RD. Personal factors related to compassion fatigue in health professionals. Anxiety, Stress & Coping: An International Journal. 2013; 26 (6):595-609
- 48. Lynch SH, Shuster G, Lobo ML. The family caregiver experience – Examining the positive and negative aspects of compassion satisfaction and compassion fatigue as caregiving outcomes. Aging & Mental Health. 2018; 22 (11):1424-1431
- 49. Goldblatt H, Buchbinder E. Challenging Gender Roles. Journal of Social Work Education. 2003; 39 (2):255-275
- 50. Gerson JI. The Development of Empathy in the Male Psychotherapist: A Researched Essay. Ohio, United States of America: The Union Institute; 1996
- 51. Kogan I. The role of the analyst in the analytic cure during times of chronic crises. Journal of the American Psychoanalytic Association. 2004; 52 (3):735-757
- 52. Batten SV, Orsillo SM. Therapist reactions in the context of collective trauma. The Behavior Therapist. 2002; 25 (2):36-40
- 53. Baum N. Trap of conflicting needs: Helping professionals in the wake of a shared traumatic reality. Clinical Social Work Journal. 2012; 40 (1):37-45
- 54. Ledoux K. Understanding compassion fatigue: Understanding compassion. Journal of Advanced Nursing. 2015; 71 (9):2041-2050
- 55. Tanner D. 'The love that dare not speak its Name': The role of compassion in social work practice. British Journal of Social Work. 2020; 50 (6):1688-1705
- 56. Coetzee SK, Klopper HC. Compassion fatigue within nursing practice: A concept analysis. Nursing & Health Sciences. 2010; 12 (2):235-243
- 57. Gilmore C. Compassion fatigue-what it is and how to avoid it. Kai Tiaki: Nursing New Zealand. 2012; 18 (5):32
- 58. Stewart DW. Casualties of war: Compassion fatigue and health care providers. Medsurg Nursing. 2009; 18 (2):91-94
- 59. Walker LO, Avant KC. Strategies for Theory Construction in Nursing. Prentice Hall Upper Saddle River, NJ: Pearson; 2005
- 60. Wynn F. Burnout or compassion fatigue? A comparative concept analysis for nurses caring for patients in high-stakes environments. International Journal for Human Caring. 2020; 24 (1):59-71
- 61. Zhang Y-Y, Zhang C, Han X-R, Li W, Wang Y-L. Determinants of compassion satisfaction, compassion fatigue and burn out in nursing: A correlative meta-analysis. Medicine (Baltimore). 2018; 97 (26):e11086
- 62. Sukut O, Sahin-Bayindir G, Ayhan-Balik CH, Albal E. Professional quality of life and psychological resilience among psychiatric nurses. Perspectives in Psychiatric Care. 2022; 58 (1):330-338
- 63. Coetzee SK, Klopper HC. Compassion fatigue within nursing practice: A concept analysis: Concept analysis of compassion fatigue. Nursing & Health Sciences. 2010; 12 (2):235-243
- 64. Stamm R, Lambert J, Garritano N, Miller J, Donnellan A. Advanced practice registered nurse subspecialty compassion satisfaction and compassion fatigue. The Journal for Nurse Practitioners. 2022; 18 (3):310-315
- 65. Slatten LA, Carson KD, Carson PP. Compassion fatigue and burnout: What managers should know. The Health Care Manager. 2020; 39 (4):181-189
- 66. Harris C, Griffin MTQ. Nursing on empty: Compassion fatigue signs, symptoms, and system interventions. Journal of Christian Nursing : A Quarterly Publication of Nurses Christian Fellowship. 2015; 32 (2):80-87
- 67. Meadors P, Lamson A, Swanson M, White M, Sira N. Secondary traumatization in pediatric healthcare providers: Compassion fatigue, burnout, and secondary traumatic stress. Omega: Journal of Death and Dying. 2009; 60 (2):103-128
- 68. Peebles-Kleiger MJ. Pediatric and neonatal intensive care hospitalization as traumatic stressor: Implications for intervention. Bulletin of the Menninger Clinic. 2000; 64 (2):257-280
- 69. Jenkins SR, Baird S. Secondary traumatic stress and vicarious trauma: A validational study. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies. 2002; 15 (5):423-432
- 70. Figley CR. Treating Compassion Fatigue. Routledge; 2002
- 71. Figley CR. Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in those Who Treat the Traumatized. Routledge; 2013
- 72. Sinclair HA, Hamill C. Does vicarious traumatisation affect oncology nurses? A literature review. European Journal of Oncology Nursing. 2007; 11 (4):348-356
- 73. Simon CE, Pryce JG, Roff LL, Klemmack D. Secondary traumatic stress and oncology social work: Protecting compassion from fatigue and compromising the worker's worldview. Journal of Psychosocial Oncology. 2005; 23 (4):1-14
- 74. Beck CT. Secondary traumatic stress in nurses: A systematic review. Archives of Psychiatric Nursing. 2011; 25 (1):1-10
- 75. Osland EJ. An investigation into the professional quality of life of dietitians working in acute care caseloads: Are we doing enough to look after our own? Journal of Human Nutrition and Dietetics: The Official Journal of the British Dietetic Association. 2015; 28 (5):493-501
- 76. Rayner S, Davis C, Moore M, Cadet T. Secondary traumatic stress and related factors in Australian social workers and psychologists. Health & Social Work. 2020; 45 (2):122-130
- 77. Hubbard GB, Beeber L, Eves E. Secondary traumatization in psychiatric mental health nurses: Validation of five key concepts. Perspectives in Psychiatric Care. 2017; 53 (2):119-126
- 78. Rogers ME. Nursing science and the space age. Nursing Science Quarterly. 1992; 5 (1):27-34
- 79. Huang Y-H, Kim H, Le M, Martinez J, Martin J, Maghen E, et al. Predictors and risk factors of compassion satisfaction, burnout, and compassion fatigue among OTs. The American Journal of Occupational Therapy. 2019; 73 (4_Supplement_1):7311505161-p1
- 80. Perry B, Toffner G, Merrick T, Dalton J. An exploration of the experience of compassion fatigue in clinical oncology nurses. Canadian Oncology Nursing Journal. 2011; 21 (2):91-97
- 81. Aron EN, Aron A, Jagiellowicz J. Sensory processing sensitivity: A review in the light of the evolution of biological responsivity. Personality and Social Psychology Review. 2012; 16 (3):262-282
- 82. Pérez-Chacón M, Chacón A, Borda-Mas M, Avargues-Navarro ML. Sensory processing sensitivity and compassion satisfaction as risk/protective factors from burnout and compassion fatigue in healthcare and education professionals. International Journal of Environmental Research and Public Health. 2021; 18 (2):611
- 83. Jenkins B, Warren NA. Concept analysis: Compassion fatigue and effects upon critical care nurses. Critical Care Nursing Quarterly. 2012; 35 (4):388-395
- 84. Benoit LG, Veach PM, LeRoy BS. When you care enough to do your very best: Genetic counselor experiences of compassion fatigue. Journal of Genetic Counseling. 2007; 16 (3):299-312
- 85. Thomas RB, Wilson JP. Issues and controversies in the understanding and diagnosis of compassion fatigue, vicarious traumatization, and secondary traumatic stress disorder. International Journal of Emergency Mental Health. 2004; 6 (2):81-92
- 86. Lynch SH, Lobo ML. Compassion fatigue in family caregivers: A Wilsonian concept analysis. Journal of Advanced Nursing. 2012; 68 (9):2125-2134
- 87. Rawal S, Strahlendorf C, Nimmon L. Challenging the myth of the attrition of empathy in paediatrics residents. Medical Education. 2020; 54 (1):82-87
- 88. Turgoose D, Maddox L. Predictors of compassion fatigue in mental health professionals: A narrative review. Traumatology. 2017; 23 (2):172-185
- 89. Mendenhall TJ. Trauma-response teams: Inherent challenges and practical strategies in interdisciplinary fieldwork. Families, Systems & Health. 2006; 24 (3):357-362
- 90. Lee H-F, Kuo C-C, Chien T-W, Wang Y-R. A meta-analysis of the effects of coping strategies on reducing nurse burnout. Applied Nursing Research. 2016; 31 :100-110
- 91. Howard H, Navega N. Pivotal events: 'I’m not a normal person anymore'—Understanding the impact of stress among helping professionals. Best Practices in Mental Health: An International Journal. 2018; 14 (2):32-47
- 92. Sansbury BS, Graves K, Scott W. Managing traumatic stress responses among clinicians: Individual and organizational tools for self-care. Trauma (London, England). 2015; 17 (2):114-122
- 93. Jo M, Na H, Jung Y-E. Mediation effects of compassion satisfaction and compassion fatigue in the relationships between resilience and anxiety or depression among hospice volunteers. Journal of Hospice and Palliative Nursing: JHPN: The Official Journal of the Hospice and Palliative Nurses Association. 2020; 22 (3):246-253
- 94. Mason VM, Leslie G, Clark K, Lyons P, Walke E, Butler C, et al. Compassion fatigue, moral distress, and work engagement in surgical intensive care unit trauma nurses: A pilot study. Dimensions of Critical Care Nursing. 2014; 33 (4):215-225
- 95. Showalter SE. Compassion fatigue: What is it? Why does it matter? Recognizing the symptoms, acknowledging the impact, developing the tools to prevent compassion fatigue, and strengthen the professional already suffering from the effects. American Journal of Hospice & Palliative Medicine. 2010; 27 (4):239-242
- 96. Lombardo B, Eyre C. Compassion fatigue: A nurse's primer. Online Journal of Issues in Nursing. 2011; 16 (1):3
- 97. McHugh MD, Kutney-Lee A, Cimiotti JP, Sloane DM, Aiken LH. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Affairs. 2011; 30 (2):202-210
- 98. Nimmo A, Huggard P. A systematic review of the measurement of compassion fatigue, vicarious trauma, and secondary traumatic stress in physicians. Australasian Journal of Disaster and Trauma Studies. 2013; 2013 (1):37
- 99. Circenis K, Millere I. Compassion fatigue, burnout and contributory factors among nurses in Latvia. Procedia, Social and Behavioral Sciences. 2011; 30 :2042-2046
- 100. Rushton CH, Batcheller J, Schroeder K, Donohue P. Burnout and resilience among nurses practicing in high-intensity settings. American Journal of Critical Care. 2015; 24 (5):412-420
- 101. Brito-Pons G, Librada-Flores S. Compassion in palliative care: A review. Current Opinion in Supportive and Palliative Care. 2018; 12 (4):472-479
- 102. Pereira-Lima K, Mata DA, Loureiro SR, Crippa JA, Bolsoni LM, Sen S. Association between physician depressive symptoms and medical errors: A systematic review and meta-analysis. JAMA Network Open. 2019; 2 (11):e1916097-e
- 103. Willard-Grace RMPH, Knox MMPH, Huang BBA, Hammer HMD, Kivlahan CMDM, Grumbach KMD. Burnout and health care workforce turnover. Annals of Family Medicine. 2019; 17 (1):36-41
- 104. Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. An official critical care societies collaborative statement: Burnout syndrome in critical care health care professionals: A call for action. American Journal of Critical Care. 2016; 25 (4):368-376
- 105. Stamm BH. The ProQOL Manual: The Professional Quality of Life Scale: Compassion Satisfaction, Burnout & Compassion Fatigue/Secondary Trauma Scales. Baltimore, MD: Sidran; 2005
- 106. Stamm BH. Measuring Compassion Satisfaction as Well as Fatigue: Developmental History of the Compassion Satisfaction and Fatigue Test. Treating Compassion Fatigue. Psychosocial Stress Series, no. 24. New York, NY, US: Brunner-Routledge; 2002. pp. 107-119
- 107. Figley CR. In: Figley CR, editor. Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in Those Who Treat the Traumatized. Vol. xxii. Philadelphia, PA, US: Brunner/Mazel; 1995. 268-xxii p
- 108. Bride BE, Radey M, Figley CR. Measuring compassion fatigue. Clinical Social Work Journal. 2007; 35 (3):155-163
- 109. Sinclair S, Raffin-Bouchal S, Venturato L, Mijovic-Kondejewski J, Smith-MacDonald L. Compassion fatigue: A meta-narrative review of the healthcare literature. International Journal of Nursing Studies. 2017; 69 :9-24
- 110. Gentry JE, Baranowsky AB. Treatment Manual for Accelerated Recovery from Compassion Fatigue. Toronto, Ontario, Canada: Psych Ink Resources; 1998
- 111. Robinson LK, Sterling L, Jackson J, Gentry E, Araujo F, LaFond C, et al. A secondary traumatic stress reduction program in emergency room nurses. SAGE Open Nursing. 2022; 8 :23779608221094530
- 112. Rajeswari H, Sreelekha BK, Nappinai S, Subrahmanyam U, Rajeswari V. Impact of accelerated recovery program on compassion fatigue among nurses in South India. Iranian Journal of Nursing and Midwifery Research. 2020; 25 (3):249
- 113. Flarity K, Gentry JE, Mesnikoff N. The effectiveness of an educational program on preventing and treating compassion fatigue in emergency nurses. Advanced Emergency Nursing Journal. 2013; 35 (3):247-258
- 114. Cohen-Katz J, Wiley SD, Capuano T, Baker DM, Shapiro S. The effects of mindfulness-based stress reduction on nurse stress and burnout, part II: A quantitative and qualitative study. Holistic Nursing Practice. 2005; 19 (1):26-35
- 115. Pfaff KA, Freeman-Gibb L, Patrick LJ, DiBiase R, Moretti O. Reducing the 'cost of caring' in cancer care: Evaluation of a pilot interprofessional compassion fatigue resiliency programme. Journal of Interprofessional Care. 2017; 31 (4):512-519
- 116. Aycock N, Boyle D. Interventions to manage compassion fatigue in oncology nursing. Clinical Journal of Oncology Nursing. 2009; 13 (2):183-191
- 117. Meadors P, Lamson A. Compassion fatigue and secondary traumatization: Provider self care on intensive care units for children. Journal of Pediatric Health Care. 2008; 22 (1):24-34
- 118. Weidlich CP, Ugarriza DN. A pilot study examining the impact of care provider support program on resiliency, coping, and compassion fatigue in military health care providers. Military Medicine. 2015; 180 (3):290-295
- 119. Nolte AG, Downing C, Temane A, Hastings-Tolsma M. Compassion fatigue in nurses: A metasynthesis. Journal of Clinical Nursing. 2017; 26 (23-24):4364-4378
- 120. Penedo FJ, Dahn JR. Exercise and well-being: A review of mental and physical health benefits associated with physical activity. Current Opinion in Psychiatry. 2005; 18 (2):189-193
- 121. Neville K, Cole DA. The relationships among health promotion behaviors, compassion fatigue, burnout, and compassion satisfaction in nurses practicing in a community medical center. The Journal of Nursing Administration. 2013; 43 (6):348-354
- 122. National Sleep Foundation. Sleep-Wake Cycle: Its Physiology and Impact on Health. 2006
- 123. Neff KD, Kirkpatrick KL, Rude SS. Self-compassion and adaptive psychological functioning. Journal of Research in Personality. 2007; 41 (1):139-154
- 124. Hall CW, Row KA, Wuensch KL, Godley KR. The role of self-compassion in physical and psychological well-being. The Journal of Psychology. 2013; 147 (4):311-323
- 125. Houck D. Helping nurses cope with grief and compassion fatigue: An educational intervention. Clinical Journal of Oncology Nursing. 2014; 18 (4):454-458
- 126. Hevezi JA. Evaluation of a meditation intervention to reduce the effects of stressors associated with compassion fatigue among nurses. Journal of Holistic Nursing. 2016; 34 (4):343-350
- 127. Owens RA, Alfes C, Evans S, Wyka K, Fitzpatrick JJ. An exploratory study of a 3-minute mindfulness intervention on compassion fatigue in nurses. Holistic Nursing Practice. 2020; 34 (5):274-281
- 128. Warren J, Morgan MM, Morris LB, Morris TM. Breathing words slowly: Creative writing and counselor self-care—The writing workout. Journal of Creativity in Mental Health. 2010; 5 (2):109-124
- 129. Groninger H. Palliative medicine fellows attend to compassion fatigue using John Stone’s ‘talking to the family’. Perspectives on Medical Education. 2015; 4 (2):83-85
- 130. Winch S, Henderson AJ, Kay M, Burridge LH, Livesay GJ, Sinnott MJ. Understanding compassion literacy in nursing through a clinical compassion café. The Journal of Continuing Education in Nursing. 2014; 45 (11):484-486
- 131. Killian KD. Helping till it hurts? A multimethod study of compassion fatigue, burnout, and self-care in clinicians working with trauma survivors. Traumatology. 2008; 14 (2):32-44
- 132. Chambers RS. Developing a peer support program to mitigate compassion fatigue in health care: A quality improvement project. Iowa Nurse Reporter. 2021; 4 (4):19
- 133. Craig CD, Sprang G. Compassion satisfaction, compassion fatigue, and burnout in a national sample of trauma treatment therapists. Anxiety, Stress & Coping: An International Journal. 2010; 23 (3):319-339
- 134. Kadambi MA, Ennis L. Reconsidering vicarious trauma: A review of the literature and its' limitations. Journal of Trauma Practice. 2004; 3 (2):1-21
- 135. Deighton RM, Gurris N, Traue H. Factors affecting burnout and compassion fatigue in psychotherapists treating torture survivors: Is the therapist's attitude to working through trauma relevant? Journal of Traumatic Stress. 2007; 20 (1):63-75
- 136. Hofmann PB. Addressing compassion fatigue. The problem is not new, but it requires more urgent attention. Healthcare Executive. 2009; 24 (5):40-42
- 137. Tjeltveit AC, Gottlieb MC. Avoiding the road to ethical disaster: Overcoming vulnerabilities and developing resilience. Psychotherapy: Theory, Research, Practice, Training. 2010; 47 (1):98
- 138. Paiva-Salisbury ML, Schwanz KA. Building compassion fatigue resilience: Awareness, prevention, and intervention for pre-professionals and current practitioners. Journal of Health Service Psychology. 2022; 48 (1):39-46
- 139. Romano J, Trotta R, Rich VL. Combating compassion fatigue: An exemplar of an approach to nursing renewal. Nursing Administration Quarterly. 2013; 37 (4):333-336
- 140. Al-Majid S, Carlson N, Kiyohara M, Faith M, Rakovski C. Assessing the degree of compassion satisfaction and compassion fatigue among critical care, oncology, and charge nurses. The Journal of Nursing Administration. 2018; 48 (6):310-315
- 141. Why emergency nurses are said to succumb to “burnout” while other nurse specialties are said to succumb to “compassion fatigue”; is there a difference? Journal of Emergency Nursing. 2019; 45 (1):4-5
© 2022 The Author(s). Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3.0 License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Continue reading from the same book
Published: 22 March 2023
By Bruce W. Newton
130 downloads
By Sara Ventura and Alison Jane Martingano
171 downloads
By Neil E. Grunberg and Erin S. Barry
310 downloads
What Is Compassion Fatigue? 24 Causes & Symptoms Explained

In a helping role, we get up close with the trauma and suffering of clients and patients to try to understand their perspective and resonate with their pain.
Compassion is a wonderful gift to those we help. It is the experience of deep empathy for a person suffering coupled with a desire to resolve their misfortune or remedy their pain (Figley, 2002b; Stamm, 2002).
Although compassion can be deeply rewarding, it can also come at a cost, particularly if we’re frequently exposed to others’ traumatic experiences in our role as helpers.
In this article, we’ll outline some symptoms of compassion fatigue, delve into how it begins, and provide real-life examples of compassion fatigue in the helping profession.
Before you continue, we thought you might like to download our three Stress & Burnout Prevention Exercises (PDF) for free . These science-based exercises will equip you and your clients with tools to manage stress better and find a healthier balance in your life.
This Article Contains
Compassion fatigue explained: 22 symptoms, what causes compassion fatigue, compassion fatigue vs burnout, 3 real-life examples of compassion fatigue.
- Fascinating Research Findings & Models
The Psychology of Vicarious Trauma
3 best books on the topic, self-care resources from positivepsychology.com, a take-home message.
Compassion fatigue is a form of stress or tension that arises from frequent contact with traumatized people, where we become preoccupied with the suffering or pain of others (Hunsaker, Chen, Maughan, & Heaston, 2015).
Compassion fatigue is a serious problem that can undermine a person’s mental and physical health and negatively affect their relationships and ability to care for others (Cocker & Joss, 2016).
Compassion fatigue can show itself in a range of symptoms and behaviors, such as:
- Diminished ability or interest to care for others
- Preoccupation with people you help
- Mental and/or physical exhaustion
- Anger and irritability
- Anxiety and/or depression
- Intrusive thoughts
- Sleep problems
- Being easily startled
- Hopelessness about helping work
- Hypervigilance
- Avoidance of certain activities, situations, or people you help
- Feeling like a failure as a helper
- Drops in productivity
- Emotional numbness
- Trouble separating personal and professional life
- A decreased capacity to experience sympathy and empathy
- Dysfunctional coping behaviors, e.g., misusing alcohol or drugs
- Taking more time off work
- Reduced decision-making ability
- Feeling disconnected
- Decreased satisfaction or enjoyment with work (Cocker & Joss, 2016; Clay, 2020; Stamm, 2010)
Compassion fatigue vs empathy fatigue
The terms compassion fatigue and empathy fatigue are occasionally used interchangeably. But this can confuse the issue slightly, as some models of compassion fatigue don’t agree on the role of empathy in the development of compassion fatigue.
According to Figley (2002a), without the ability to empathize, there is little room for compassion fatigue, because empathy is essential to helping work and experiencing the strains of caring. Empathic concern is our impetus to help those people that are suffering, for example, by providing our services as a therapist (Figley, 2002a).
Our empathic response toward clients and patients is how we try to remedy a client’s suffering and can lead us to share in their emotional responses. “Compassion stress” is the consequence of empathic responding and represents the ongoing desire to reduce the suffering of the client or patient (Figley, 2002a).
If compassion stress is severe and/or compounded by other life stresses, it can lead to compassion fatigue (Figley, 2002a), which can be emotionally overwhelming and make it more difficult to experience empathy (Clay, 2020).
However, a more recent model of compassion fatigue challenges the idea that it is empathy that makes us vulnerable to compassion fatigue (Coetzee & Laschinger, 2017). Instead, Coetzee and Laschinger (2017) suggest a lack of resources, the person’s response to the distress, and inadequate positive feedback make us susceptible to compassion fatigue. We’ll get into these models in more detail a little further on.

When our job is to help others who are in distress or traumatized, we must adopt the perspective of the person who is suffering to empathize with them (Figley, 2002a).
By doing this, we are necessarily exposed to the emotional energy and trauma of the particular patient we are working with, which can lead to secondary traumatic stress (Figley, 2002b; Stamm, 2012).
Over time, we can also experience burnout and feel as though our helping work is not having a positive impact ( Stamm, 2012).
So, why do we continue to do compassionate work if it costs us?
According to Stamm (2012), we do it for compassion satisfaction – the positive and pleasurable experience of helping others that can be nourishing. You can experience compassion satisfaction and fatigue simultaneously, but when compassion fatigue overrides, it may undermine your ability to feel compassion satisfaction (Stamm, 2002; Bride, Radey, & Figley, 2007).
Download 3 Free Stress & Burnout Prevention Exercises (PDF)
These detailed, science-based exercises will equip you or your clients with tools to manage stress better and find a healthier balance in their life.
Download 3 Stress & Burnout Prevention Exercises Pack (PDF)
By filling out your name and email address below.
- Email Address *
- Your Expertise * Your expertise Therapy Coaching Education Counseling Business Healthcare Other
- Name This field is for validation purposes and should be left unchanged.
Burnout and secondary traumatic stress are both components of compassion fatigue, but these constructs are distinct from each other (Stamm, 2012; Cocker & Joss, 2016).
When we’ve been stressed for a long time, we can reach a state of physical, mental, and emotional exhaustion: burnout (National Health Service, n.d.). Burnout may have a range of causes, and it does not happen specifically after being exposed to another person’s trauma (Figley, 2002a; Middleton, 2015).
In contrast, secondary traumatic stress occurs when we’re unable to save someone from their suffering, and we become distressed and preoccupied with their pain (Cocker & Joss, 2016). The symptoms of secondary trauma can look very similar to post-traumatic stress disorder (Middleton, 2015).
Burnout builds up and takes hold gradually. The experience of secondary traumatic stress is typically fast, but it can contribute to the experience of burnout (Middleton, 2015; Stamm, 2012).

Nursing requires huge amounts of compassion and empathy to support those in pain, and although it can be extremely rewarding, it can also be a very emotionally demanding role.
One study found a greater distance between the care the nurses were able to provide and the quality of care they wanted to provide, as well as other physical and emotional stresses that made compassion fatigue worse (Perry, Toffner, Merrick, & Dalton, 2011). Work–life balance, colleague support, and acknowledgment were some factors that helped reduce it (Perry et al., 2011).
Low levels of manager support have predicted higher levels of burnout and compassion fatigue among emergency department nurses, whereas high levels of manager support contributed to greater compassion satisfaction (Hunsaker et al., 2015).
Social workers
Social workers frequently provide help to people who have experienced trauma, such as survivors of domestic violence or abuse . Following the September 11 terrorist attacks on the World Trade Center, researchers found that New York social workers who were exposed to clients who had been traumatized experienced secondary trauma themselves (Adams, Figley, & Boscarino, 2008).
Another study exploring the experiences of compassion fatigue among six social workers found that effective supervision and a supportive work environment played an important role in enhancing the social workers’ resilience (Kapoulitsas & Corcoran, 2015).
Foster carers
The role of foster carers is to offer children in public care a safe and loving home, and foster carers are often exposed to the early traumatic experiences of the children they look after (Bridger, Binder, & Kellezi, 2020).
A survey involving 187 British foster carers found high levels of burnout and secondary traumatic stress among the carers. Foster carers provide round-the-clock care, and not getting enough time off or away from caring was a consistent issue raised by the carers (Bridger et al., 2020).
Fascinating Research Findings & Models
Many models of compassion fatigue have been developed over the years, but one of the most influential was the Compassion Stress and Fatigue Model by Figley (1995, 2002a, 2002b).
The Compassion Stress and Fatigue Model
At the heart of it, Figley (1995, 2002a) proposes that empathy and emotional energy are essential for therapists (or helpers) to connect with others and to respond to their suffering effectively. Essentially, we need to be able to adopt the perspective of the person we’re helping to understand the best way to help them.
As a result, therapists are then directly exposed to the emotions of the person in pain and are motivated to remedy or decrease their suffering through their empathetic responses (Figley, 2002a).
When the therapist feels a continuing demand to reduce the client’s suffering, this can create compassion stress. This can negatively impact the therapist’s wellbeing unless they manage this stress through a sense of achievement or disengagement (Figley, 2002a).
With disengagement, the therapist actively distances themselves from the client’s suffering between sessions and puts effort into their own self-care . Obtaining a sense of achievement and satisfaction from helping work also requires therapists to have some awareness to understand the limits of their responsibility (Figley, 2002a).
A few other important factors that contribute to compassion fatigue include (Figley, 2002a):
- Prolonged exposure The feeling of responsibility for helping those in pain for a significant period of time—breaks and vacations are important to avoid this.
- Traumatic recollections Emotional memories that the client triggers for the therapist—these may reflect the therapist’s experiences of other clients who were especially difficult, demanding, or suffering greatly.
- Life disruption Any life event that disrupts your routine, schedule, or ability to manage and cope with your daily responsibilities.
Compassion Fatigue Model
The compassion fatigue model (Coetzee & Laschinger, 2017) aimed to build on previous models of compassion fatigue by weaving in the conservation of resources theory and growing research on the social neuroscience of empathy.
Ultimately, this model suggests that positive feedback, balanced resources, and reducing self-focused personal distress when working with those we help can mitigate compassion fatigue (Coetzee & Laschinger, 2017).
– Resources
The conservation of resources theory proposes that all caregivers have a certain balance of resources. The caregiver’s resource balance can be healthy or diminished for many reasons; for instance, they may have poor resources in their workplace, a lack of support at home, or low emotional energy (Coetzee & Laschinger, 2017).
– Resource appraisal
Your assessment of your resource balance will influence whether or not you see those you help as a threat to your resources and can influence whether your empathic focus is on yourself or the client (Coetzee & Laschinger, 2017).

– Other focus
Adopting an other focus means we are empathizing with the client and see things from their viewpoint, while also knowing that there is a clear boundary between the self and the other (Coetzee & Laschinger, 2017).
When investing resources in helping others, Coetzee and Laschinger (2017) suggest that therapists will expect some resource gain from helping in the form of positive feedback, such as the outcome for the client or praise. If the therapist faces a negative outcome, such as a lack of recognition or failed treatment, this can lead to a sense of resource loss (Coetzee & Laschinger, 2017).
– Self-focus
The main difference between other- and self-focus is the lack of distinction between the self and other. Self-focus can lead to more distress for the therapist.
Self-focused propositional processing (controlled, voluntary, and “cognitive”) can lead the therapist to assess their own thoughts and feelings about the client and their suffering, which can sometimes be helpful and other times, lead to distress (Coetzee & Laschinger, 2017).
Self-focused experiential processing (automatic, involuntary, and associated with emotional resonance) is more problematic and can lead to distress for the therapist and motivate them to avoid or withdraw from the client (Coetzee & Laschinger, 2017).
How do we overcome compassion fatigue? With self-care and self-compassion.
While a hallmark of therapist-practitioner relationships is compassion, practitioners often fail to apply it to themselves (Coaston, 2017).
Therefore, an essential first step in overcoming compassion fatigue is tending to the self with kindness.
Being compassionate to the self might mean setting emotional boundaries, reducing one’s workload, letting colleagues know that we’re struggling, and even seeking professional help. Although it is difficult to be kind to ourselves when our clients need us, we know that we can’t be the best support if we feel vulnerable.
In saying this, overcoming compassion fatigue isn’t always about making massive changes. Sometimes simply connecting to our values of why we do this work can be crucial in combating and preventing compassion fatigue.
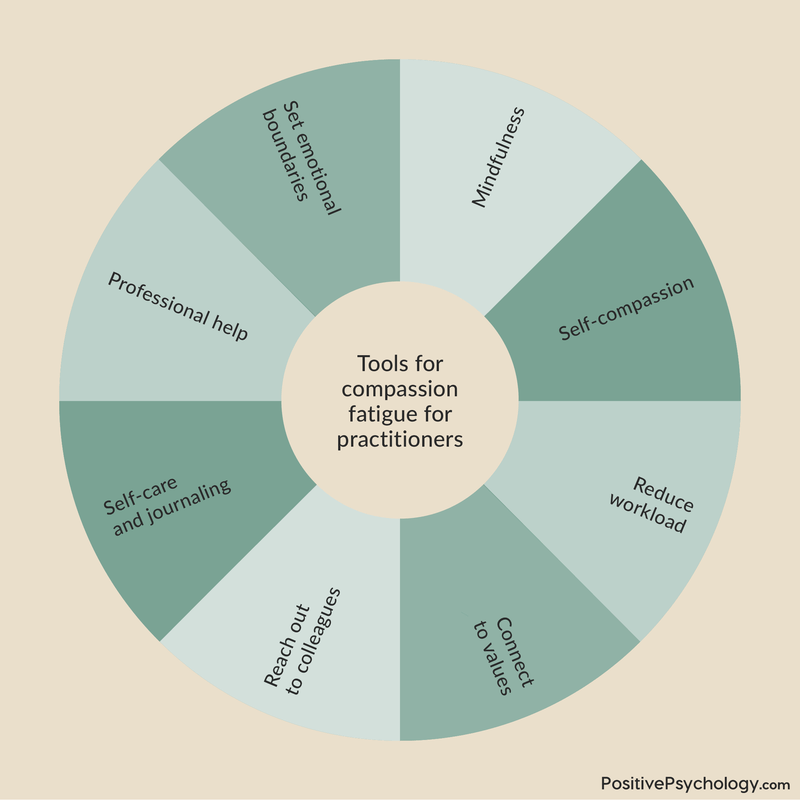
Compassion fatigue interventions
As well as getting enough support at work and enhancing opportunities for compassion satisfaction, some simple interventions may be helpful to reduce compassion fatigue.
– Trauma training
Specialized trauma training has been linked to lower compassion fatigue and higher compassion satisfaction, suggesting that being more knowledgeable about trauma may be a helpful buffer against trauma exposure (Sprang, Clark, & Whitt-Woosley, 2007).
– Self-care
This may seem like an obvious one, but it’s something many of us find hard to prioritize when caring for others. One study of hospice professionals found that those reporting a greater number of self-care strategies experienced lower burnout and compassion fatigue (Alkema, Linton, & Davies, 2008).
– Mindfulness
Research has found a positive relationship between mindfulness (attention awareness) and compassion satisfaction, and a negative relationship between mindfulness and secondary traumatic stress and burnout in people supporting the traumatically bereaved (Thieleman & Cacciatore, 2014).

But vicarious trauma is different from compassion fatigue and involves the changing of the helper’s schemas (mental frameworks or life beliefs) because of exposure to the traumatic experiences of others (Jenkins & Baird, 2002).
Learning about the trauma of others can trigger profound shifts in how a helper understands themselves or others, which can be very distressing (Jenkins & Baird, 2002).
Compared to secondary traumatic stress, vicarious trauma is less observable, happening below the surface, as the helper’s worldview is transformed. But distress and burnout symptoms can be common to both experiences (Jenkins & Baird, 2002).
As with secondary traumatic stress, vicarious trauma happens through empathic engagement with someone else’s trauma. But while secondary traumatic stress often happens rapidly, vicarious trauma builds up over time through repeatedly hearing about other people’s trauma (Jenkins & Baird, 2002).
Compassion fatigue is a complex and fascinating topic that is highly relevant to anyone in a caring role. If you’re keen to expand your library with compassion fatigue literature, here are some of our top picks:
1. Treating Compassion Fatigue – Charles R. Figley
Figley is one of the pioneers of traumatology research and theory, and this book is an extremely informative and comprehensive read for any trauma practitioner.
An impressive list of traumatology researchers have contributed to the book’s 11 chapters, which cover compassion fatigue theory, research, and treatment.
Find the book on Amazon .
2. Help for the Helper: The Psychophysiology of Compassion Fatigue and Vicarious Trauma – Babette Rothschild
This book delves into the psychophysiology of compassion fatigue and vicarious trauma and explores neurobiology, social psychology, folk psychology, and strategies for managing stress and burnout.
Rothschild is an internationally acclaimed expert in the treatment of trauma and a body-psychotherapist, and she has written numerous books, including the widely popular The Body Remembers series.
3. Surviving Compassion Fatigue: Help for Those Who Help Others – Beverly D. Kyer
Kyer is a clinical social worker and trauma specialist who has dedicated much of her life to helping others.
In this book, you’ll learn about her personal experience with compassion fatigue and how she overcame it.
This book has great practical appeal, as you’ll learn strategies and techniques to support your wellbeing and self-care while caring for those in need.
We all need a little help with self-care from time to time, and if you’re overdue for some time-out or time-off, take this as your cue to prioritize yourself. Below are some of our free self-care resources to help you get started.
- Self-Care Check-In This self-assessment uses ratings and reflection questions to help you determine how to better meet your self-care needs.
- Self-Care Checkup This worksheet helps you consider the frequency and quality of your self-care across five important life domains and includes a useful list of more than 40 self-care activities.
- My Self-Care Promise This worksheet helps you reflect on your unique needs, identify activities you find restorative, and promise to treat yourself kindly when self-care is needed.
If you’re looking for more science-based ways to help others manage stress without spending hours on research and session prep, this collection contains 17 validated stress management tools for practitioners. Use them to help others identify signs of burnout and create more balance in their lives.
Ultimately, you should also know how to prevent compassion fatigue, and our article on How to Prevent and Treat Compassion Fatigue + Tests is a good place to start.
17 Exercises To Reduce Stress & Burnout
Help your clients prevent burnout, handle stressors, and achieve a healthy, sustainable work-life balance with these 17 Stress & Burnout Prevention Exercises [PDF].
Created by Experts. 100% Science-based.
Many of us pursuing a career in the helping profession find great joy, meaning, and fulfillment in helping others.
But at the same time, offering compassion to those in need is a deeply emotional and resource-demanding process. Compassion fatigue comes in the form of secondary traumatic stress and burnout and can happen when being exposed to other people’s trauma.
Compassion satisfaction is a truly nourishing and pleasant experience that comes from helping others, which may help to stave off compassion fatigue. Having adequate resources to do your job and a supportive work environment, managing self-related distress, receiving positive feedback, and practicing self-care are other key factors that may help to reduce compassion fatigue.
Compassion fatigue can affect your mental and physical wellbeing and your ability to care for others. If you’re concerned that you may be developing compassion fatigue, it’s important to speak to someone and ask for support. As well as caring for others, you need to care for yourself too.
We hope you enjoyed reading this article. Don’t forget to download our three Stress & Burnout Prevention Exercises (PDF) for free .
- Adams, R. E., Figley, C. R., & Boscarino, J. A. (2008). The compassion fatigue scale: Its use with social workers following urban disaster. Research on Social Work Practice , 18 (3), 238–250.
- Alkema, K., Linton, J. M., & Davies, R. (2008). A study of the relationship between self-care, compassion satisfaction, compassion fatigue, and burnout among hospice professionals. Journal of Social Work in End-of-Life & Palliative Care , 4 (2), 101–119.
- Bride, B. E., Radey, M., & Figley, C. R. (2007). Measuring compassion fatigue. Clinical Social Work Journal , 35 (3), 155–163.
- Bridger, K. M., Binder, J. F., & Kellezi, B. (2020). Secondary traumatic stress in foster carers: Risk factors and implications for intervention. Journal of Child and Family Studies , 29 (2), 482–492.
- Clay, R. A. (2020, June 11). Are you experiencing compassion fatigue? American Psychological Association. Retrieved from https://www.apa.org/topics/covid-19/compassion-fatigue
- Coaston, S. C. (2017). Self-care through self-compassion: A balm for burnout. Professional Counselor, 7(3) , 285-297.
- Cocker, F., & Joss, N. (2016). Compassion fatigue among healthcare, emergency and community service workers: A systematic review. International Journal of Environmental Research and Public Health, 13(6) , 618.
- Coetzee, S. K., & Laschinger, H. K. (2017). Toward a comprehensive, theoretical model of compassion fatigue: An integrative literature review. Nursing & Health Sciences , 20 , 4–15.
- Figley, C. R. (Ed.). (1995). Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized . Brunner/Mazel.
- Figley, C. R. (2002a). Compassion fatigue: Psychotherapists’ chronic lack of self care. Journal of Clinical Psychology , 58 (11), 1433–1441.
- Figley, C. R. (2002b). Treating compassion fatigue . Brunner/Rutledge.
- Hunsaker, S., Chen, H. C., Maughan, D., & Heaston, S. (2015). Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. Journal of Nursing Scholarship , 47 (2), 186–194.
- Jenkins, S. R., & Baird, S. (2002). Secondary traumatic stress and vicarious trauma: A validational study. Journal of Traumatic Stress , 15 (5), 423–432.
- Kapoulitsas, M., & Corcoran, T. (2015). Compassion fatigue and resilience: A qualitative analysis of social work practice. Qualitative Social Work , 14 (1), 86–101.
- Kyer, B. D. (2016). Surviving compassion fatigue: Help for those who help others. Gatekeeper Press.
- Middleton, J. (2015). Addressing secondary trauma and compassion fatigue in work with older veterans: An ethical imperative. Journal of Aging Life Care , 5 , 1–8.
- National Health Service. (n.d). Stress and Burnout . Retrieved from https://www.practitionerhealth.nhs.uk/stress-and-burnout
- Perry, B., Toffner, G., Merrick, T., & Dalton, J. (2011). An exploration of the experience of compassion fatigue in clinical oncology nurses. Canadian Oncology Nursing Journal/Revue Canadienne de Soins Infirmiers en Encologie , 21 (2), 91–97.
- Rothschild, B. (2006). Help for the helper: The psychophysiology of compassion fatigue and vicarious trauma. W. W. Norton.
- Sprang, G., Clark, J. J., & Whitt-Woosley, A. (2007). Compassion fatigue, compassion satisfaction, and burnout: Factors impacting a professional’s quality of life. Journal of Loss and Trauma , 12 (3), 259–280.
- Stamm, B. H. (2002). Measuring compassion satisfaction as well as fatigue: Developmental history of the Compassion Satisfaction and Fatigue Test. In C. R. Figley (Ed.), Treating compassion fatigue (pp. 107–119). Brunner-Routledge.
- Stamm, B. H. (2010). The concise manual for the professional quality of life scale (2nd ed.). ProQOL.org.
- Stamm, B. H. (2012). Helping the helpers: Compassion satisfaction and compassion fatigue in self-care, management, and policy. In A.D. Kirkwood & B.H. Stamm (Eds.), Resources for community suicide prevention (pp. 1–4). Idaho State University.
- Thieleman, K., & Cacciatore, J. (2014). Witness to suffering: Mindfulness and compassion fatigue among traumatic bereavement volunteers and professionals. Social Work , 59 (1), 34–41.
Share this article:
Article feedback
What our readers think.
Thank you for sharing your article. Recent research from Tania Singer has shown that there is no such thing as Compassion Fatigue. You don’t get tired of being compassionate. You get “emphatic distress”. She has shown that empathy is not pro-social, that why we can get emphatic distress. This article above should be reviewed and corrected
Thank you for mentioning Tania Singer’s research which differentiates between empathic distress and compassion.
It’s important to acknowledge that “compassion fatigue” is a term historically used, particularly in healthcare, to describe emotional exhaustion from exposure to suffering. Singer’s research suggests that this term might be a misnomer, as it could be more closely related to empathy than compassion.
In light of this, our article could definitely benefit from incorporating or at least acknowledging these distinctions. It’s essential to adapt language and concepts as our understanding evolves. Thanks for bringing this to our attention.
Kind regards, Julia | Community Manager
Really insightful and useful article Helen, thank you. As a vet for 28 yrs and now a coach I hadn’t really stopped to look at compassion fatigue but all of it rings true. Times when your tank feels empty. Decisions to step away and recharge for long periods. Reliance on ways to relax like alcohol. Finally choosing to move away from a career that has both given and taken continuously, I get to find my joy in coaching others with a strong focus on positive psychology.
Dr. Helen Brown, that’s awesome information.
beautiful article. thank you.
Hello, I am an Office Manager in a Non-helper profession office. I have employees with mental and physical health issues and I am shocked to say, I believe I have compassion fatigue! With so many issues affecting these employees’, their work, our overall work environment and levels, and the continuing nature of all of these, I find I don’t want to listen, or even hear about these issues, to the point of avoidance (not appropriate)! What happened to my empathy? As we come out of the pandemic, what advice and resources are available for us “regular” office workers dealing with compassion fatigue and burnout? Thank you for any assistance.
I’m sorry to hear you’re experiencing compassion fatigue. I’m sure you’ll agree there are a lot of people in need at the moment, so it’s little wonder the need for empathy is spreading well beyond the typical ‘helping’ professions.
My main suggestion would be to see whether you can engage the people above you to request structural support or an intervention for your staff. If people are coming forward needing support, this may be flowing on to affect their ability to perform, suggesting there’s a likely business case for investing in some support, thereby taking some load off you. You can read more re: this business case in this excellent report by Attridge (2008) and article by Pescund et al. (2015) .
For you personally — well done on recognizing that your capacities are being stretched! For a range of suggestions to look after yourself, take a look at our dedicated article for ideas.
I hope this helps, and best of luck!
– Nicole | Community Manager
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

How to Prevent and Treat Compassion Fatigue + Tests
The wide range of circumstances experienced by counselors and therapists leaves them open and vulnerable to experiencing compassion fatigue (Negash & Sahin, 2011). Such a [...]

Empathy 101: 3+ Examples and Psychology Definitions
Have you ever experienced someone else’s emotions as your own? Has a book, film, or photograph ever driven you to tears? Or have you ever [...]

Living With the Inner Critic: 8 Helpful Worksheets (+ PDF)
We all know this voice in our head that constantly criticizes, belittles, and judges us. This voice has many names: inner critic, judge, saboteur, the [...]
Read other articles by their category
- Body & Brain (49)
- Coaching & Application (57)
- Compassion (26)
- Counseling (51)
- Emotional Intelligence (24)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (20)
- Mindfulness (45)
- Motivation & Goals (45)
- Optimism & Mindset (34)
- Positive CBT (28)
- Positive Communication (20)
- Positive Education (47)
- Positive Emotions (32)
- Positive Leadership (18)
- Positive Parenting (4)
- Positive Psychology (33)
- Positive Workplace (37)
- Productivity (16)
- Relationships (46)
- Resilience & Coping (36)
- Self Awareness (21)
- Self Esteem (38)
- Strengths & Virtues (32)
- Stress & Burnout Prevention (34)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)
Download 3 Free Self-Compassion Tools Pack (PDF)
3 Self-Compassion Tools (PDF)
Compassion fatigue in healthcare providers: A systematic review and meta-analysis
Affiliations.
- 1 University of Calgary, Canada.
- 2 Alberta Health Services, Canada.
- 3 Carleton University, Canada.
- PMID: 31829113
- DOI: 10.1177/0969733019889400
Background: Compassion fatigue is recognized as impacting the health and effectiveness of healthcare providers, and consequently, patient care. Compassion fatigue is distinct from "burnout." Reliable measurement tools, such as the Professional Quality of Life scale, have been developed to measure the prevalence, and predict risk of compassion fatigue. This study reviews the prevalence of compassion fatigue among healthcare practitioners, and relationships to demographic variables.
Methods: A systematic review was conducted using key words in MEDLINE, PubMed, and Ovid databases. Data were extracted from a total of 71 articles meeting inclusion criteria, from studies measuring compassion fatigue in healthcare providers using a validated instrument. Quantitative and qualitative data were extracted and compiled by three independent reviewers into an evidence table that included basic study characteristics, study strength and quality determination, measurements of compassion fatigue, and general findings. Meta-analysis, where data allowed, was stratified by Professional Quality of Life version, heterogeneity was quantified, and pooled means were reported with 95% confidence interval. A table of major study characteristics and results was created.
Ethical consideration: This paper contains no primary data obtained directly from research participants. Data obtained from previously published resources have been acknowledged within references. Psychological distress, particularly compassion fatigue, can be insidious, no health profession is immune, and may significantly impact the ability to provide care.
Results: A total of 71 studies were included. Compassion fatigue was reported across all practitioner groups studied. Relationships to most demographic variables such as years of experience and specialty were either not statistically significant or unclear. Variability in reporting of Professional Quality of Life results was found.
Interpretation: Compassion fatigue exists across diverse practitioner groups. Prevalence is highly variable, and its relationship with demographic, personal, and/or professional variables is inconsistent. Questions are raised about how to mitigate compassion fatigue.
Keywords: Burnout; Professional Quality of Life; compassion fatigue; healthcare practitioner; nursing; secondary trauma.
Publication types
- Meta-Analysis
- Systematic Review
- Burnout, Professional / etiology
- Burnout, Professional / psychology
- Compassion Fatigue / complications
- Compassion Fatigue / etiology*
- Compassion Fatigue / psychology
- Health Personnel / psychology*
- Job Satisfaction
- Middle Aged
- Quality of Life / psychology
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Compassion Fatigue among Healthcare, Emergency and Community Service Workers: A Systematic Review
Fiona cocker.
1 School of Public Health and Preventive Medicine, Monash Centre for Occupational and Environmental Health (MonCOEH), Monash University, Prahran 3004, Australia
Nerida Joss
2 Melbourne School of Population and Global Health, University of Melbourne, Melbourne 3010, Australia; [email protected]
Compassion fatigue (CF) is stress resulting from exposure to a traumatized individual. CF has been described as the convergence of secondary traumatic stress (STS) and cumulative burnout (BO), a state of physical and mental exhaustion caused by a depleted ability to cope with one’s everyday environment. Professionals regularly exposed to the traumatic experiences of the people they service, such as healthcare, emergency and community service workers, are particularly susceptible to developing CF. This can impact standards of patient care, relationships with colleagues, or lead to more serious mental health conditions such as posttraumatic stress disorder (PTSD), anxiety or depression. A systematic review of the effectiveness of interventions to reduce CF in healthcare, emergency and community service workers was conducted. Thirteen relevant studies were identified, the majority of which were conducted on nurses ( n = 10). Three included studies focused on community service workers (social workers, disability sector workers), while no studies targeting emergency service workers were identified. Seven studies reported a significant difference post-intervention in BO ( n = 4) or STS ( n = 3). This review revealed that evidence of the effectiveness of CF interventions in at-risk health and social care professions is relatively recent. Therefore, we recommend more research to determine how best to protect vulnerable workers at work to prevent not only CF, but also the health and economic consequences related to the ensuing, and more disabling, physical and mental health outcomes.
1. Introduction
The compassion and empathy shown by healthcare, emergency and community service professionals can prove psychically, mentally and economically costly. In short, exposure to patients or clients experiencing trauma or distress can negatively impact professional’s mental and physical health, safety and wellbeing, as well as that of their families, the people they care for, and their employing organizations. The term compassion fatigue (CF) was coined to described the phenomenon of stress resulting from exposure to a traumatized individual rather than from exposure to the trauma itself [ 1 ]. An often extreme state of tension and preoccupation with the emotional pain and/or physical distress of those being helped can create a secondary traumatic stress (STS) for the caregiver [ 2 , 3 ], and, when converged with cumulative burnout (BO), a state of physical and mental exhaustion caused by a depleted ability to cope with one’s everyday environment [ 4 , 5 , 6 ], CF results.
CF is characterized by exhaustion, anger and irritability, negative coping behaviours including alcohol and drug abuse, reduced ability to feel sympathy and empathy, a diminished sense of enjoyment or satisfaction with work, increased absenteeism, and an impaired ability to make decisions and care for patients and/or clients [ 7 ]. The negative effects of providing care are aggravated by the severity of the traumatic material to which the caregiver is exposed, such as direct contact with victims, particularly when the exposure is of a graphic nature. This places certain occupations, such as healthcare, emergency and community service workers, at an increased risk of developing CF and potentially more debilitating conditions such as depression and anxiety [ 8 ], and even posttraumatic stress disorder (PTSD) [ 9 ]. These conditions are known to increase sickness absence, psychological injury claims, and job turnover, and negatively impact productivity.
Compassion fatigue (CF) has been variously defined, and the related concepts of BO, STS and vicarious traumatisation (VT) are often used interchangeably and incorrectly to describe the phenomenon. BO and STS are related to CF, but as defined by Stamm, they are two distinct outcomes of exposure [ 10 ]. As demonstrated by Figure 1 , BO and STS arise from separate failed survival strategies [ 11 ]. BO arises from a assertiveness-goal achievement response and occurs when an individual cannot achieve his or her goals and results in “frustration, a sense of loss of control, increased willful efforts, and diminishing morale” [ 11 ]. Alternatively, STS arises from a rescue-caretaking response and occurs when an individual cannot rescue or save someone from harm and results in guilt and distress [ 11 ]. Subsequently, STS and BO lead to CF if the aforementioned symptoms are not mediated by a third, equally important concept of compassion satisfaction (CS). CF and CS can be seen as the positive and negative consequences of working with individuals who have experienced or are currently experiencing trauma or suffering [ 10 ]. As a result, a substantial amount of evidence suggests CS is an important part of the whole [ 12 ], thus increasing the significance of building resiliency and the transformation from negative to positive aspects [ 10 , 13 , 14 ].

Compassion fatigue: conceptual model adapted from Middleton [ 28 ].
The most commonly used definition of CF was developed by Figley [ 1 ] and describes the concept as “a state of exhaustion and dysfunction biologically, psychologically, and socially as a result of prolonged exposure to compassion stress and all it invokes” (p. 253). This definition more effectively encompasses the multiple dimensions of CF. Lynch and Lobo [ 15 ] defined the attributes of CF as an established relationship between the caregiver and the patient/client all associated with the caregiving role and the psychological and physical responses it arouses [ 15 ]. Yoder et al . [ 16 ] identified triggering events based on nurses taking care of patients who were experiencing serious life-threatening situations and cases involving futile or palliative care. Lynch and Lobo [ 15 ] also identified system issues or organisational factors, such as physical and emotionally demanding assignments and extra work days as risk factors for CF, while Najjar et al . identified that empathy is vital to the development of CF, as the caregiver must have the ability to perceive and understand what their patient/client is experiencing and be able to communicate this understanding [ 17 ]. Finally, the psychological response to the conflicting elements of empathy and suffering provides the foundation for ongoing stress and subsequent CF [ 15 ]. In summary, CF results from “the change in empathetic ability of the caregiver in reaction to the prolonged and overwhelming stress of caregiving” [ 15 ].
CF is most commonly measured using the validated Professional Quality of Life (ProQoL) scale. The overall concept of ProQoL is a complex milieu of characteristics of the work environment (organization, tasks), the individual’s personal characteristics, and their exposure to primary and secondary trauma in the work setting. In short, ProQoL refers to the quality one feels in relation to their work as a caregiver, and both the positive and negative aspects of doing one’s job. As such, the ProQoL scale measures both pre-cursors of CF (BO and STS), and CS.
Since the mid-1990s [ 1 , 18 , 19 , 20 ] the emotional, cognitive, and physical consequences of providing professional services to trauma victims and survivors have been addressed in the literature and several conceptual models have been developed in attempt to explain them. However, the majority of research to date has focused on identifying the prevalence and predictors of CF in a unique occupational group such as nurses [ 21 , 22 ], therapists [ 23 , 24 ], community service workers, and healthcare professionals in hospital emergency departments or intensive care units [ 25 ]. While these studies have gone some way to illuminate how CF can be addressed, their findings cannot be generalised to working populations beyond the healthcare sector. Furthermore, despite the identification of modifiable individual and organisational risk factors used to inform the development of interventions and programs to prevent and treat CF, few studies have attempted to examine and interrogate the quality of these preventive measures. These include workload intensity, inadequate rest time periods between shifts, task repetitiveness [ 3 ], low control and low job satisfaction [ 26 ], poor resilience, lack of meaningful recognition, and poor managerial support [ 27 ]. As a result, employers and managers in the healthcare, emergency and community services sectors have very little conclusive evidence as to the best way to prevent CF, and physical and mental health outcomes, when its known risk factors—exposure to traumatised patients and clients—are inherent in the type of work that the employees supervise and undertake.
The ultimate goal of CF research is to create healthy caregivers that are able to master the art of resiliency and return quickly to high-functioning behaviours, both at work and outside the workplace, after exposure to the traumatic experience of a patient or client. As experiencing secondary trauma could be considered an inherent risk for the occupations of interest in this paper, the actual job exposures may be difficult to modify. Therefore, interventions that promote individual resilience and educate at-risk workers about effective coping strategies in response to these adverse job exposures are equally important and likely to have significant health and economic benefits, as they reduce not only STS, BO and CF, but also the risk of more serious mental health disorders such as anxiety and depression, the quality of life and productivity consequences of which are well documented. Therefore, this systematic review aimed to: (i) identify existing evidence on interventions to reduce CF in healthcare, and emergency and community service professionals; and (ii) determine the most effective workplace-based strategies for reducing CF, directly or via modifying its recognised individual and organisational risk factors and/or promoting Compassion Satisfaction.
2.1. Search Strategy
The following search strategy was carried out using the major relevant database search engines ( i.e ., EMBASE, CINHAL, PsychInfo, Web of Science, PubMed, and Scopus). Search terms were divided into four groups. Group 1 related to CF, related concepts, and variants or derivatives such as VT or STS. Group 2 included at-risk occupation types commonly exposed to known risk factors for CF such as frontline health, emergency and community service workers. Group 3 included terms related to the study design, for which we used the Cochrane search terms for identifying interventions and trials (e.g., intervention or training or program or efficacy or randomized control group). Group 4 related to employment type or derivatives of related words such as employees, workers and professionals.
The search was limited to peer-reviewed articles published in English between January 1990 and December 2015. Both authors (Fiona Cocker and Nerida Joss) screened article titles and abstracts to determine eligibility. In addition, a hand search of key journals and reference lists of all studies selected for inclusion in the analysis was conducted. Appendix Table A1 contains a summary of the search strategy.
2.2. Inclusion and Exclusion Criteria
The inclusion criteria dictated that the studies contained a quantitative evaluation of an intervention that reported outcomes on a standardized and validated measure for compassion fatigue. This measure could be any of the validated versions of the most commonly used Professional Quality of Life (Pro-QoL) or a less common, but equally valid measure of CF. Alternatively, the outcomes could be one of the sub-scales of the Pro-QoL; CS, a protective factor, or STS or BO, both of which are known risk factors for CF. Finally, the outcome could be a subscale of a general health measure that has evidence of validity as a CF, BO, STS, or CS screening tool (e.g., Maslach Burnout Scale [ 29 ], or The Resilience Scale [ 30 ]). The intervention had to target CF directly or indirectly through a known risk factor for CF, such as those reviewed in the introduction (lack of meaningful recognition, years of experience, higher job satisfaction, and poor psychosocial work climate). The intervention settings could be in work or non-work settings. Studies were excluded if they did not report on CF, focused on prevalence of CF only, or used a qualitative methodology.
2.3. Data Extraction
The variables extracted covered intervention descriptors, sample characteristics, implementation characteristics, quality of the research design (use of control group, random allocation), and outcome indicators. We did not use a quality rating score in the analysis, as it introduces subjectivity and is prone to incomplete data. Coding instructions and guidelines were developed by the first and second authors in order to reduce the subjectivity of decisions made. On completion of the coding, the first author (Fiona Cocker) independently checked the coding of each of the papers. Instances in which disagreement with the initial coding decisions occurred were resolved by consensus between both authors (Fiona Cocker and Nerida Joss).
2.4. Statistical Analysis
Our primary outcomes were the components of the ProQoL: BO, STS and CS. Due to the small number of studies identified ( n = 13), no statistical analysis was undertaken, and meta-analysis was not possible.
Figure 2 presents the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram summarizing the inclusion and exclusion decisions made by both authors (Fiona Cocker and Nerida Joss). Due to the small number of hits generated (229), all articles were carefully inspected to determine whether they met criteria for inclusion, as opposed to making exclusion decisions solely on the basis of the initial title screening. Following this review, two duplicate articles were removed, and 216 articles were excluded. The majority of the studies ( n = 198, 91.6%) were excluded, as they focused solely on prevalence of CF, or a CF risk factor, within a particular occupational group. The remainder of articles were excluded, as they did not evaluate the effectiveness of a CF prevention or intervention program, their primary focus was not CF, or they did not have a specific, validated measure of CF or factors which contribute to CF. For example, studies were excluded if they had a PTSD or stress-related outcome measure, measures of general psychosocial functioning, or well-being scales that have not been established in the literature as valid indicators of CF. The application of these inclusion criteria resulted in a total of 13 studies being deemed suitable for the detailed, systematic review and data extraction.

Flow diagram of study selection. CF=Compassion Fatigue.
3.1. Characteristics of Included Studies
Characteristics of included studies ( n = 13) are presented in Table 1 . Of the included studies n = 11 (84.6%) were conducted in the USA [ 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 ], one in Australia [ 42 ], and one in Israel [ 43 ]. Ten of the thirteen studies included nurses (76.9%), with three studies specifically focusing on oncology nurses [ 32 , 34 , 35 ], one on pediatric nurses [ 43 ], and one on emergency nurses [ 39 ]. Other occupational groups represented were social workers ( n = 2, 15.4%) [ 31 , 33 ], chaplains ( n = 1, 7.7%) [ 33 ], hospice workers ( n = 1, 7.7%) [ 40 ], disability sector workers ( n = 1, 7.7%) [ 42 ], and miscellaneous medical staff ( n = 3, 23.1%) [ 37 , 38 , 41 ]. No studies targeting emergency service workers were identified. The 13 studies included represented a total sample size of 671 ( M = 52, SD = 43), with sample sizes for the individual studies ranging from seven [ 36 ] to 154 [ 34 ]. Of those that reported mean age ( n = 7, 53.8%) [ 31 , 34 , 35 , 38 , 40 , 42 , 43 ], averages ranged from 40.5 years [ 35 ] to 49.3 years [ 43 ], and of those which reported sex distribution ( n = 11, 84.6%) [ 31 , 32 , 33 , 34 , 35 , 36 , 38 , 39 , 40 , 42 , 43 ], the majority of subjects were female (58.8% [ 42 ]–100% [ 43 ]). All included studies had a follow-up period ranging from three weeks [ 31 ] to six months [ 35 ] post-intervention.
Summary of included studies reporting on CF interventions ( n = 13).
a BO = burnout, CS = compassion satisfaction, STS = secondary traumatic stress/secondary traumatization, CF = compassion fatigue; b ES = Effect Size; c TBS = Team Building Questionnaire; MBI = Maslach Burnout Inventory; EAI = Empathy Assessment Inventory; PSS = Perceived Stress Scale; DHSES = Disaster-Helper Self-Efficacy Scale; RSE = Rosenberg Self-Esteem Scale; HS = Hope Scale; MAAS = Mindful Attention Awareness Scale; HCAHPS = Hospital Consumer Assessment of Healthcare Providers and Systems; DASS = Depression Anxiety Stress Scale; FFMQ = Five Facet Mindfulness Questionnaire; PHQ-9 = Patient Health Questionnaire (9); PANAS = Positive and Negative Affect Schedule; SWLS = Satisfaction With Life Scale; CBI = Copenhagen Burnout Inventory; HCGI = Hospice Clinician Grief Inventory; WES = Work Environment Scale; WCQ = Ways of Coping Questionnaire; CD-RISC = Connor-Davidson Resilience Scale; d Licensed Practical Nurses.
3.2. Outcome Measurements
Ten (76.9%) of the included studies used a version of the Professional Quality of Life Scale (ProQoL) [ 10 ] to measure CF, as well as its subscales CS, BO and STS. Other measures of CF used were The Compassion Fatigue Scale (CFS), both original [ 1 ] and revised [ 44 ] versions, designed to assess both secondary trauma and job burnout, and the Compassion Satisfaction and Fatigue Test (CSFT) [ 12 ]. Three (23.1%) of the included studies [ 31 , 32 , 39 ] measured only one type of outcome (e.g., ProQoL, Version 5, Manufacturer, City, Country). The remaining ten included articles [ 33 , 34 , 35 , 36 , 37 , 38 , 40 , 41 , 42 , 43 ] measured the following outcomes in addition to CF ( Table 1 ): (i) burnout [ 34 , 35 , 38 , 42 , 45 ]; (ii) team building [ 33 ]; (iii) impact of traumatic events [ 34 ]; (iv) satisfaction with work or life [ 34 , 42 ]; (v) empathy [ 36 ]; (vi) resilience [ 36 , 41 ]; (vii) depression, anxiety, stress, or perceived stress [ 36 , 37 , 38 , 42 ]; (viii) self-efficacy [ 43 ], self-esteem [ 43 ]; mastery and hope [ 43 ]; mindfulness [ 37 , 38 ], healthcare consumer assessment [ 37 ], general health [ 42 ]; grief [ 40 ]; work environment [ 40 ]; and coping [ 41 ].
3.3. Intervention Design
All of the interventions evaluated in the included studies were individually focused, and the majority ( n = 7, 53.8%) focused on stress reduction using yoga and/or mindfulness [ 31 , 37 , 42 ], structured meditation [ 32 , 39 ], music therapy [ 33 ], or a combination thereof [ 38 ]. Of the remaining four included studies, two evaluated interventions focused on building individual resilience [ 34 , 35 ], one aimed to build professional self-efficacy [ 43 ], and Stanton et al . [ 36 ] used Transcranial Magnetic Stimulation to increase resilience and empathy, and reduce stress. Eleven studies described single-faceted interventions focusing on yoga, mindfulness, meditation, or music therapy [ 31 , 32 , 33 , 37 , 38 , 40 , 42 ], resilience and coping [ 34 , 35 , 41 ], or transcranial magnetic stimulation [ 36 ]. In contrast, Berger et al . [ 43 ] and Flarity et al . [ 39 ] described more complex interventions involving on multiple, interactive sessions focused on promoting professional self-efficacy, improving theoretical knowledge, and assigning homework tasks, and individual and group exercises, guided imagery, take home materials including print-outs, DVDs and music CDs, and access to educational resources and publications, respectively. The included studies differed in their methodology; ten studies (76.9%) [ 31 , 32 , 33 , 34 , 35 , 36 , 37 , 39 , 41 , 42 ] used a pre/post design, two studies (15.4%) used randomised controlled designs (RCTs), one with a waitlist control group [ 38 ], the other with a no treatment, concurrent control group [ 40 ]. Finally, Berger et al . [ 43 ] used a quasi-random control trial with a wait list control group. Intervention periods of the included studies ranged from three to twelve weeks ( M = 6.1, SD = 2.7), session length ranged from 16 to 240 min ( M = 78.9, SD = 58.6), and the frequency of sessions ranged from once a week to five times a week ( M = 1.5, SD = 1.2). None of the included studies assessed intervention quality using a validated measure, and the majority of studies ( n = 10, 76.9%) used unrepresentative, convenience samples.
3.4. Effect of Interventions to Prevent or Manage Compassion Fatigue
The follow-up intervals ranged from three weeks [ 31 ], immediately post-intervention, to 6 months [ 35 ] after the baseline measurements. Eight (61.5%) of included studies reported a significant difference post-intervention in either CF, or one of the ProQoL subscales BO, CS, or STS. More specifically, five studies (38.5%) [ 32 , 34 , 35 , 39 , 41 ] reported significantly reduced BO and STS, risk factors for CF, and three studies (23.1%) [ 38 , 39 , 43 ] reported significantly increased CS, a protective factor in the development of CF. Flarity et al ., the one study to achieve reduction in BO and STS and an increase is CS, conducted an intensive, two-level intervention amongst emergency nurses involving, firstly, a four hour, interactive group seminar focused the “…origin of CF, the physiological effects, signs and symptoms of CF and BO, as well as the factors associated with emergency nursing that may lead to CF and BO”, as well as providing information about how to prevent and treat CF using the five elements identified by Gentry et al . [ 44 ]; self-regulation, intentionality, perceptual maturation/self-validated caregiving, connection and self-care. Secondly, participants were given multimedia resources such as printed seminar handouts, a guided imagery CD, access to a website with CF, CS and resiliency educational resources and publications, and DVD which informed them of Gentry’s [ 44 ] aforementioned five elements. This is, by far, the most comprehensive intervention evaluated by the included studies and, not surprisingly, has the most significant, positive outcomes. Unlike the other twelve interventions evaluated, this intervention focuses on teaching participants: (i) about CF; (ii) how to recognise, and actively prevent and treat CF in themselves and their colleagues; and (iii) provides them with tools and resources to consolidate these learnings which is likely to increase the probability of these positive outcomes remaining long term. However, this is yet to be determined.
4. Discussion
This systematic review identified the evidence on interventions designed to reduce CF in health, emergency and community service workers to determine the most effective workplace based strategies for reducing CF directly or via modifying its recognised individual and organisational risk factors. Despite the significant attention given to measuring the prevalence of CF in this cohort of workers, there is a lack of information and evidence about effective interventions designed to reduce CF in these occupational groups. We have found that, despite recognition of the threat exposure to secondary trauma poses to the mental health and wellbeing of certain at-risk occupational groups, and the established existence of wellness programs to combat CF and related concepts, rigorous, academic evaluation of evidence on this topic has only recently emerged in the last few years, with the earliest study published in 2011 with a group of 80 pediatric nurses in Israel, thus indicating the relative novelty of interventional research in this area. By consolidating the small amount of evidence available we have been able to identify promising interventions in this area as well as the evidence gaps and areas in need of research attention in the future. In doing so, the subsequent evidence based workplace-based interventions have the potential to reduce CF and more serious, chronic and economically costly mental disorders, to the benefit of individual workers, employers and the broader society and economy through the retention of healthy, productive workers who service those in need of healthcare and social assistance.
4.1. Study Population Characteristics
The majority of studies identified in our search have been generated from the US ( n = 11), with nurses as the occupational group of interest ( n = 10). As such, nurses were disproportionally represented, limiting the generalizability of findings to other equally at-risk occupations such as police, fire fighters, paramedics and other health and community service workers. Further, the majority of subjects represented in the included studies were female (58.8% [ 42 ] to 100% [ 43 ]), which, while reflective of the healthcare and social assistance industry to which many of the at-risk populations belong [ 46 ], once again, reduces the level of generalizability as other occupational groups at-risk of CF, such as the male-dominated emergency services [ 46 ] are not included. Older workers were also disproportionally represented, with averages ranging from 40.5 years [ 35 ] to 49.3 years [ 43 ], thus limiting applicability of the findings to younger workers who may be at risk of developing CF. More specifically, evidence has identified that both age and years of professional experience were protective factors for STS, CF, or BO [ 47 , 48 , 49 ]. In addition to the over-representation of several demographic characteristics, some individual characteristics (e.g., educational attainment) and organisational factors (e.g., long work hours and caseloads with high percentages of trauma patients) which have been associated with an increased incidence of STS and CF [ 50 , 51 ], were not considered.
4.2. Study Design and Methodological Quality
Comparison between studies was difficult given the heterogeneity of the interventions themselves and the lower level of methodological quality for the majority of studies. The majority of studies were of low to moderate quality ( n = 11), with only two RCT studies included in our review [ 38 , 40 ]. The majority of studies ( n = 10) employed a pre-post design, most of which did not include a long-term follow up (≥8 weeks). Additionally, the length of the intervention period varied considerably from a single four hour session [ 39 ] to six, one hour sessions once a week for 12 weeks [ 43 ]. This is a concern, as significant behavioural and personal routine modification is required in some cases, without any complementary changes being made to the work-related risk factors such as reduced exposure to traumatised patients or clients or increased rest between shifts. Change is also unlikely within this short time period [ 52 , 53 ], thus making significant improvement in CS or a significant decrease in BO and/or STS similarly improbable. Finally, in addition to highly variable methodological design and quality, most studies included ( n = 12) have small sample sizes with less than 100 subjects, which reduce statistical power, increase the possibility of type II error, and reduce the ability for statistical tests to detect significant differences between values.
4.3. Effectiveness of CF Interventions
The thirteen included studies in our search demonstrated mixed or no effects. While ten studies reported significant improvement in at least one element of CF, no study reported positive change on all three indicators (STS, BO, CS) and only one study had a follow up period of longer than eight weeks. This makes it difficult to determine with any certainty whether these effects were likely to be sustained over time.
When we considered the findings of the included studies by the content of the interventions evaluated, didactic and ecologic music therapy interventions were shown to be ineffective, as was grief resolution, which involves expression of grief feelings, connecting socially with colleagues experiencing similar feelings, and participation in a grief ritual to farewell patients who had died, Transcranial Direct Current Stimulation, and mindfulness education. In contrast, structured meditation using an audio CD [ 32 ], and interactive group seminars followed by individual and group exercises such as guided imagery, and multimedia resources (printed handouts, DVD, guided imaging/music CD, a website with CF and CS, and resiliency educational resources and publications) resulted in a significant decrease in BO. However, the most promising trend was for the effectiveness of interventions involving an element focused on teaching and/or bolstering resilience [ 35 , 39 , 41 ], all of which showed improvement in BO, and two of which demonstrated a reduction in STS and BO, and an improvement in CS. These findings are encouraging, as they suggest that workers in at-risk occupational groups can be taught to cope with the known risk factors for the development of CF, which are also, unfortunately, unavoidable parts of their job. It also suggests a need to invest in programs such as the Accelerated Program for Compassion Fatigue (ARP), developed by Gentry et al . [ 44 ], a five-session model for the treatment of the deleterious effects caregivers experience as a result of their care giving work [ 54 ] through the promotion of resilience and self-efficacy. Participants in the ARP not only report a reduction in CF symptoms, they also feel more empowered, more energetic, and have a stronger sense of self-worth. Designed to reduce the intensity, frequency and duration of symptoms associated with Compassion Fatigue, ARP aims to help at-risk workers identify symptoms of CF, recognise CF triggers, identify and utilize existing available resources, review personal and professional history to the present day to identified those at increased risk, master arousal reduction methods, resolve any impediments to efficacy, initiate conflict resolution, and initiate a supportive aftercare plan-in collaboration with their employer or supervisor.
The ARP program borrows from PTSD literature and focuses on the restorative quality of personal self-awareness and promotes the sharing of stories and debriefing to assist those experiencing CF in rebuilding their professional and personal life quality. The ARP also advocates the promotion of self-compassion in order to encourage individuals to challenge a negative internal dialogue and focus on shifting their automatic thoughts and beliefs to reflect more positive outlook. Finally, the program promotes the development of a combination of “Resiliency Skills” of “Antibodies” which, have been shown to be correlated with lessened CF, greater job satisfaction, better quality of life and lessened anxiety [ 54 , 55 ]. They are as follows: (i) self-care and revitalisation; (ii) connection and support; (iii) intentionality, or eradicating stress and shifting from reactive to intentional behavior [ 56 ]; (iv) self-regulation, which involves developing the ability to intentionally control the activity and lessen the energy of the Autonomic Nervous System while engaged in the activities of daily living. For some, this may prove as simple as relaxing the muscles while encountering the myriad of perceived threats that emerge throughout each workday; and (v) perceptual maturation, which is a cognitive skill and involves maturing the perceptions of self towards resiliency and the perceptions of the workplace, to render them less toxic.
4.4. Limitations
While a thorough search strategy was designed to undertake this systematic review, limitations should be considered in the interpretation of results. As with any search, despite searching six major databases, some studies may have been missed. Our search was limited to only search English language journals, and, therefore, studies published in a language other than English might have missed.
4.5. Implications for Future Research
This review indicates that there is some promising evidence emerging about interventions to reduce CF, in particular in nurses. However, given the small number of published studies to date, it is difficult to determine the impact on this or other occupations. The review has shown that in particular, there is a gap in research conducted in many emergency occupations such as police and fire fighters, and other health community services such child protection and disability support workers, and disability and human service workers, and further research is needed using more rigorous study designs and representative samples. These groups are particularly susceptible to developing CF due to the nature of their work. In addition, future research could focus on the impact of CF interventions in a more diverse range of at-risk occupation groups, over-sample younger aged workers and men in order to the determine the effectiveness of interventions designed to reduce CF, or prevent and manage known risk factors, in these established at-risk populations.
This can be best understood if we consider CF, or its risk and protective factors BO, STS, and CS, as upstream determinants of common mental disorders such as a depression and anxiety, the health and economic cost of which can be considerable within the employed population [ 57 , 58 , 59 ]. More specifically, by reducing the incidence of CF, future cases of depression and anxiety could be prevented, thus reducing the related health and economic consequences of these conditions. The effectiveness of this approach was demonstrated in the work of LaMontagne et al . [ 60 ], who estimated that the potential cost saving of eliminating job strain as an avoidable predictor of depression was $730 million AUD for one year and $11.8 billion AUD over a lifetime. However, it must be noted that, although workplace psychosocial stressors, such as job strain, have been linked to poor mental and physical health in a growing body of scientific evidence, the exploration of CF in such a relationship is a relatively newer concept. Therefore, future work is required to: (i) establish the degree to which, if any, CF increases a worker’s future risk of depression or anxiety, after accounting for other known risk factors; and (ii) establish whether CF can be effectively reduced or eliminated by a combination of work- and worker-directed interventions across occupational groups. Once established, the epidemiological and economic modelling approach used by LaMontagne et al . [ 60 ] could be used to highlight the financial value of investing in the mental health workers at-risk of CF in addition to the existing legal or moral motivators, to the ultimate benefit of employers, workers, and the patients and clients they serve.
Furthermore, there has been minimal effort made to apply the aforementioned findings about health, allied health, and community service workers to reduce CF and its negative health, wellbeing and safety consequences. Therefore, we recommend a systematic review be conducted to determine the prevalence of CF across occupation types to assist in identifying those most at risk, and, therefore, in most need of intervention. Finally, although it is difficult to make definitive conclusions due to the quality of the evidence in this review, the interventions that contain at least one element of resilience training appeared to have the most effect on CF. Therefore, we suggest researchers, employers and managers consider this when designing interventions to reduce CF in the future.
5. Conclusions
To our knowledge, this is the first review to attempt to evaluate the evidence of the effectiveness of CF interventions in at-risk health, emergency and social care professions. Results revealed that, despite an awareness of the prevalence of CF in these at-risk workers, there is a lack of information and evidence about effective workplace based strategies to reduce CF in these occupational groups via modifying its recognised individual and organisational risk factors. Therefore, we recommend more research to determine how best to protect vulnerable workers in order to prevent CF, as well as the potentially more significant health and economic consequences related to the subsequent physical and mental health outcomes.
Acknowledgments
The authors thank Tegan Daley-Driscoll for her assistance with conducting the searches and identifying potentially relevant papers.
Appendix A. Search Strategy
Search parameters were created to identify studies that met the following criteria:
- Published in the past 25 years (January 1990–December 2015)
- Targeting a known risk factor or a protective factor for CF
- See key words below for “CF and related concepts” OR
- Targeting CF directly
- Included a valid outcome measure of CF
- See key words below for “At-risk occupations”
- See key words below for “Design”
- See key words below for “Employment type”
- EMBASE, CINHAL, PsychInfo, Web of Science, PubMed, Scopus, Google Scholar
- Exclude the following papers:
- Journal of Traumatic Stress
- Work and Stress
- Occupational and Environmental Medicine
- Oncology Nursing Forum
- Nursing Administration Quarterly
- Health and Social Work
Keywords used in Search Strategy.
Author Contributions
Both Fiona Cocker and Nerida Joss defined the aims of this systematic review, designed the search strategy, defined the inclusion and exclusion criteria, reviewed the identified articles, extracted and reviewed the data, and prepared and edited the manuscript.
Conflicts of Interest
The authors have no conflict of interest.
Compassion Fatigue Essays
Care; remedial program for teachers with compassion fatigue., the impact of secondary traumatic stress on nurses: compassion fatigue, coping strategies, and self-care, popular essay topics.
- American Dream
- Artificial Intelligence
- Black Lives Matter
- Bullying Essay
- Career Goals Essay
- Causes of the Civil War
- Child Abusing
- Civil Rights Movement
- Community Service
- Cultural Identity
- Cyber Bullying
- Death Penalty
- Depression Essay
- Domestic Violence
- Freedom of Speech
- Global Warming
- Gun Control
- Human Trafficking
- I Believe Essay
- Immigration
- Importance of Education
- Israel and Palestine Conflict
- Leadership Essay
- Legalizing Marijuanas
- Mental Health
- National Honor Society
- Police Brutality
- Pollution Essay
- Racism Essay
- Romeo and Juliet
- Same Sex Marriages
- Social Media
- The Great Gatsby
- The Yellow Wallpaper
- Time Management
- To Kill a Mockingbird
- Violent Video Games
- What Makes You Unique
- Why I Want to Be a Nurse
- Send us an e-mail
We use cookies to enhance our website for you. Proceed if you agree to this policy or learn more about it.
- Essay Database >
- Essay Examples >
- Essays Topics >
- Essay on Health
Plan To Combat Compassion Fatigue And Burnout Essay Samples
Type of paper: Essay
Topic: Health , Nursing , Emotions , Stress , Adult , Adulthood , Spiritual , Breastfeeding
Words: 1000
Published: 11/06/2021
ORDER PAPER LIKE THIS
Work burnout and stress are common phenomenon in a health care setting due to long work working hours, hostile clients, complexity of illnesses and divergent view from the colleagues. As such, lack of good sleep, losing temper and getting irritated are common occurrence which can hardly be avoided in this profession. Factors which contribute to these adverse occurrences and frustrations are strict work schedules, emergency cases, poor work procedures and schedules, errors and near misses, lack of data, poor relations, ethical dilemma and lack of resources/equipment. Thus, absenteeism, sick leave, depression, mental sickness and temper are frequent results of work burnout and stress. Notably, the health care setting is a complex environment with variety of persons that may or may not blend well with each other due to differences in character perspective on life, purpose, goals, culture and spiritual believes. Thus, regularly health practitioners differ with each other on how certain assignment should be carried out and who should be involved. Hence, in order to overcome this difficulty when it comes to building healthy relationship in the workplace, it is better to appreciate the contribution played by each staff and respect their work since they have a great role to play in ensuring that the health facility achieves its goals. Additionally, God has managed to place individuals in different work settings to ensure every person plays a greater role in making the world a better place. Every staff in a health facility has been assigned a duty by God so as to fulfill their purpose here on earth. Therefore, health practitioners and subordinates ought to work together irrespective of their differences to achieve a common goal and fulfill the assignment they have been given by God.
1.4 2.4 3.3 4.4 5.3 6.4 7.3
Total 25/28 (Emotional adult)
Part B: Principle 1 1.3 2.3 3.4 4.3 5.3 6.3
Total 21/24 (Emotional adult)
Principle 2 7.2 8.2 9.4 10.3 11.4 12.4
Total 19/24 (Emotional adolescent)
Principle 3 13.3 14.3 15.3 16.3 17.4 18.3 19.3
Total 22/28 (Emotional adult)
Principle 4 20.3 21.4 22.3 23.4 24.3 25.3
Total 20/24 (Emotional adult)
Principle 5 26.4 27.3 28.4 29.2 30.3
Total 16/20 (Emotional adult)
Principle 6 31.2 32.3 33.4 34.4 35.3 36.3 37.4 38.3 39.3 40.3
Total 32/40 (Emotional adult)
Burnout inventory 1. b 2. b 3. b 4. a 5. b 6. a 7. b 8. a 9. a 10. b 11. b 12. c
Total 39/48 {Feverish (elevated burnout risk)}
Being a nurse, I appreciate the fact that it is my mandate to give care to individuals that are sickly in the society. This is in line with the God’s requirement of serving others. However, there are challenges that are likely to present themselves in our efforts to serve others (Morrison & Korol, 2014). Incidences of burnout are likely to catch up with us when providing care to patients. From my own assessment, my burnout levels are at the Feverish stage. This implies that I am in a better position to manage my stress well but I’m likely to occasionally get trapped in stress levels that are likely to lead to depression and other sorts of illnesses (Morrison & Korol, 2014). Such burnout incidences may result from the fact that I may not receive adequate sleep due to cases of emergency that may come in while I’m at home relaxing. Therefore, such incidences are likely to make my temperament towards my work to change thus making me easily irritable (Morrison & Korol, 2014). This ease in irritability is likely to affect my concentration levels when performing daily activities like cleaning and cooking. Consequently, such overwhelming incidences will result in increased burnout incidences. Although, mostly aim at a position to manage my stress level and intermingle with clients and colleagues comfortably, at times it come really hard to manage my stress level and fatigue especially during emergency and sudden change of work schedule. Additionally, differences in opinion and perspective with colleagues arise which affect my relation with them and which can be stressing. Conclusively, it is vital to promote my spiritual well-being by addressing the factors that are likely to lead to burnout and stress. As such, sharing tribulations so as to come up with solutions concerning different problems in the healthcare setting is vital in promoting quality holistic care to patients. Changing operational procedures and schedules is also vital in reducing burnout incidences. Getting guidance from counselors and praying also form the basis under which I can be able to address my emotional burnout. Reading inspirational materials and meditation also, assist a lot in getting inner peace which goes a long way in curbing incidences of burnout and promote spiritual growth. Therefore, the aforementioned activities are targeted at promoting my spiritual growth and eliminating burnout incidences.
Dossey, B. M., & Keegan, L. (2012). Holistic nursing. Jones & Bartlett Publishers. Haugan, G., Rannestad, T., Hammervold, R., Garåsen, H., & Espnes, G. A. (2014). The relationships between self‐transcendence and spiritual well‐being in cognitively intact nursing home patients. International journal of older people nursing, 9(1), 65-78. Morrison, K. B., & Korol, S. A. (2014). Nurses' perceived and actual caregiving roles: identifying factors that can contribute to job satisfaction.Journal of clinical nursing, 23(23-24), 3468-3477. Solomon, J. (2014). Nurses ‘coping strategies with compassion fatigue: A Literature Review.

Cite this page
Share with friends using:
Removal Request

Finished papers: 2613
This paper is created by writer with
ID 267646385
If you want your paper to be:
Well-researched, fact-checked, and accurate
Original, fresh, based on current data
Eloquently written and immaculately formatted
275 words = 1 page double-spaced

Get your papers done by pros!
Other Pages
Violence essays, front entrance essays, funiculus essays, extractor essays, example of article review on scholarly writing analysis, critical thinking on w6 learning journal qualitative research, good creative writing about some of the most important factors that i would consider when evaluating computer hardware include, good example of essay on forestry manager, free kerry steinmann essay sample, macro environment essay example, educational research essay to use for practical writing help, natural justice essay, cultural risk factors example essay by an expert writer to follow, are we too dependent on computers argumentative essay, sample essay on the treatment of juveniles, employee performance appraisal case study, free essay on police conduct and integrity, good research proposal about role of family in psychological development of the individual, transmission tower structural assessment engineering assignments examples, good example of essay on project evaluation, public administration case study sample, good example of finance essay 6, perfect model essay on watergate scandal, jetblue airways westjet airlines and others a sample case study for inspiration mimicking, dignity in euthanasia example essay by an expert writer to follow, essay on dandelion wine, learn to craft essays on understanding white collar crime with this example, diversity and cultural competence a sample research paper for inspiration mimicking, good essay on ethical decision making counselor joe, sample essay on dynamic leadership, proper essay example about products and cost allocation, essay on qualitative research phenomenology, contributor case studies, nutrient case studies, pillar case studies, brush case studies, juice case studies, basin case studies, brushing case studies, ice cream case studies, obstacle case studies, refund case studies.
Password recovery email has been sent to [email protected]
Use your new password to log in
You are not register!
By clicking Register, you agree to our Terms of Service and that you have read our Privacy Policy .
Now you can download documents directly to your device!
Check your email! An email with your password has already been sent to you! Now you can download documents directly to your device.
or Use the QR code to Save this Paper to Your Phone
The sample is NOT original!
Short on a deadline?
Don't waste time. Get help with 11% off using code - GETWOWED
No, thanks! I'm fine with missing my deadline
Peter DeWitt's
Finding common ground.
A former K-5 public school principal turned author, presenter, and leadership coach, DeWitt provides insights and advice for education leaders. He can be found at www.petermdewitt.com . Read more from this blog .
To Boost Student Mental Health, Support Teachers

- Share article
Professional development since 2020 has featured some version of this check-in.

While we chuckled in person or virtually shared into a Zoom chat, we were met with shallow acknowledgement of stressors and then back to work we went. Education has had key shifts, and 2020 was different from those previous shifts. Between school shutdowns, an unprecedented mistrust of community toward educators, and political divide in society, it is no wonder sessions opened with tiptoeing around the needs of educators. These challenges have persisted while changing the landscape of our schools.
A more accurate check-in might look like this:

When considering these squares from real voices, it may be hard to identify with one. We must brace ourselves for deeper challenges, including a looming fiscal cliff. As budgets tighten, critical resources dwindle. Support that offset behavior and mental health are among the first to go. Our teachers, academic counselors, and administrators will be left with the task of serving as ill-prepared and ill-equipped behavioral interventionist, mental health professional, and social-skills instructor. That goes in tandem with expectations of taking students with learning gaps to higher academic levels.
While well-meaning districts and leaders have facilitated after-school yoga sessions, like many other ideas, it falls short. A group of teachers, paraprofessionals, and principals from Southern California have provided insight into actionable steps to go beyond check-ins to address the impact that a post-pandemic world has had.

Align the Currently Existing MTSS System
Schools have some version of a multitiered system of support (MTSS). Implementation falls short from three factors: 1) lack of common language and common understanding of the components of and alignment to MTSS; 2) ineffective communication across all levels of the school system; and 3) identified Tier 1 strategies need not be implemented universally.
Strengthen Classroom-Level Processes
Teachers have observed high levels of aggression, anxiety, developmental delays, relationship problems, and trauma among students. As teachers better identify challenges, they have found the most effective tool in addressing and reducing the symptoms of behaviors was consistent and clear classroom structures and routines. Schools that had strong schoolwide Positive Behavioral Intervention and Support (PBIS) systems realized more success through implementation across the school.
Implement Tiered Levels of Support
It seems the understanding of tiered levels of support is limited to identifying that there are up to four tiers of support. There is a need to establish a common language and a common understanding. Students cannot access services that adults cannot speak to clearly. Teams should look at already existing proven frameworks such as PBIS, trauma-informed practices, Zones of Regulation, and Universal Design for Learning (UDL) to align tiers of intervention to their MTSS framework.
Empower Teacher Assessment to Connect to Services
An ineffective process is the student study team. Teachers identify academic, behavioral, mental, or social challenges. They then follow steps outlined that, at a minimum, can take up to 12 weeks from referral, identification and implementation of interventions, and meeting to discuss outcomes. Many times a full year was wasted because teachers could have been provided the tools to act immediately. The elephant in the room: Teachers expressed signaled mistrust in their ability to serve a student just in time. Schools need to overhaul their student study-team system to allow teachers to have immediate access to implement interventions. One suggestion is to follow the Everyone Graduates Center ABC Model developed in partnership with John Hopkins University.
Utilize the Multidisciplinary Team
While tools and agency should be given to execute support, teachers cannot work in isolation. After establishing common language and common understanding around the various strategies, tiers of interventions, and support available, schools should utilize a framework for communication and ongoing access to resources. The Everyone Graduated Center ABC Model offers guidelines for creating cohorts, forming effective teams, and scheduling meetings in a proactive rather than reactive manner.
Identify and Address Barriers to Implementation
Building and district leaders must address eight different barriers:

This is the starting point for immediate action. Building and site leaders must establish common language and common understanding around frameworks and practices that need to be implemented or better aligned. We must also care for our staff’s mental health differently. This begins with ensuring that our teachers’ professional development needs, as well as this alignment, is done during the workday. While it is great to provide teachers with additional pay after school, when teachers express burnout and compassion fatigue, putting in hours after a long workday does not cut it. We show we are serious about supporting our teachers by incorporating this into the professional workday and fully equipping and training our teams.
The opinions expressed in Peter DeWitt’s Finding Common Ground are strictly those of the author(s) and do not reflect the opinions or endorsement of Editorial Projects in Education, or any of its publications.
Sign Up for The Savvy Principal
Edweek top school jobs.

Sign Up & Sign In


IMAGES
VIDEO
COMMENTS
Compassion fatigue can affect the most dedicated workers—people who continue to help by working extra shifts or foregoing days off, neglecting their own self-care. This can result from exposure ...
Compassion fatigue (CF), or the extreme stress and burnout from helping others, is widely considered to be harmful to professional well-being. Due to a lack of awareness and education around CF in healthcare professionals, mental health clinicians may feel particularly unsure about how to treat these common symptoms. There is considerable ...
This 66-item questionnaire is a more extensive and revised version of the CFST that contains a series of positively oriented questions intended to measure compassion satisfaction and fatigue (Bride et al., 2007). Statements scored include: I have happy thoughts about those I help and how I could help them.
4.1 The connection between empathy and compassion fatigue. Compassion is an essential component of patient care provided by health professionals [ 46 ]. The care-giving relationship is founded on empathy and a critical characteristic of compassion fatigue is a loss or lack of empathy [ 47, 48 ].
Compassion fatigue can show itself in a range of symptoms and behaviors, such as: Diminished ability or interest to care for others. Preoccupation with people you help. Mental and/or physical exhaustion. Anger and irritability. Anxiety and/or depression. Intrusive thoughts. Sleep problems. Being easily startled.
Essay on Compassion Fatigue. Compassion represents an "acknowledgement of another's suffering and is accompanied by the expression of a desire to ease or end that suffering." (Van der Cingal, 2009, p. 124) This is a fundamental characteristic usually found in health care workers and nurses especially. In one twelve hour shift, a nurse's ...
He begins by defining "compassion fatigue" from Figley (1995. p.7) as the behaviors and emotions resulting from knowing about a traumatic event experienced by someone else and the resulting stress from wanting to or helping this person. Compassion fatigue is further distinguished from "burnout" by stating that it involves higher levels ...
Background: Compassion fatigue is recognized as impacting the health and effectiveness of healthcare providers, and consequently, patient care. Compassion fatigue is distinct from "burnout." Reliable measurement tools, such as the Professional Quality of Life scale, have been developed to measure the prevalence, and predict risk of compassion ...
Compassion Fatigue Essays. New workers in the health care role are often excited, energetic, and ready to take on whatever comes at them. Little do they know compassion fatigue is nipping at their heels. Compassion fatigue is common among health care providers and consists of five major concepts. These five concepts are ambiguity, no-win ...
What is Nursing Compassion Fatigue and Burnout? In response to the work-place stressors that nurses face in the hospital setting, many have developed ineffective comping mechanisms demonstrated by detachment and relationship distancing while others have fallen victim to compassion fatigue and burnout (Lee, Daugherty, Eskierka, & Hamelin, 2019).
Compassion fatigue (CF) is stress resulting from exposure to a traumatized individual. CF has been described as the convergence of secondary traumatic stress (STS) and cumulative burnout (BO), a state of physical and mental exhaustion caused by a depleted ability to cope with one's everyday environment. Professionals regularly exposed to the ...
Compassion Fatigue Essays. Care; Remedial Program for Teachers With Compassion Fatigue. For some teachers, their beloved professional career morphs and takes an unexpected emotional turn. From excitement to exhaustion, thriving to survive, a sense of hollowness slowly replaces the spark of hope. These feelings are part of a phenomenon called ...
The main characteristic of compassion fatigue is its ability to affect the physical, social, and emotional well-being of a person. The symptoms caused by compassion fatigue can be divided into work-related, emotional, and physical issues (Lombardo & Eyre, 2011). Examples of work-related issues include avoiding patients, reduced empathy, or poor ...
Essay on Compassion Fatigue. Compassion represents an "acknowledgement of another's suffering and is accompanied by the expression of a desire to ease or end that suffering." (Van der Cingal, 2009, p. 124) This is a fundamental characteristic usually found in health care workers and nurses especially. In one twelve hour shift, a nurse's ...
PAGES 2 WORDS 541. Compassion Burnout. The author of this report has been asked to take and assess two surveys. Once getting the results of the surveys, the author is to answer several questions. The first question asks the author how the author would deal with compassion fatigue if and when it rears its head.
Paper Type: 2500 Word Essay Examples. Compassion fatigue, which is also known, as secondary traumatic stress is a natural effect that occurs as a result of taking care of patients who are in pain, stressed, suffering, or traumatized. Compassion fatigue commonly affects nurses who show extreme empathy for patients and their relatives.
Aim: The purpose of this study is to determine the relationship and effect level among com-. passion fatigue, empathy, and emotional contagion in fourth- year nursing students. Methods: The study ...
Essay On Compassion Fatigue. 2285 Words10 Pages. Scope of the Problem One research study on compassion fatigue and burnout found that "burnout has been more closely associated with systemic stressors in the work environment (Malachi, 2003), and compassion fatigue has been associated with the demands of interacting with traumatized clients ...
Behavioral symptoms of compassion fatigue usually manifest in behaviors that are out of the ordinary for the person. Some examples might include irritability, being withdrawn from family, friends and co-workers, moody, appetite changes, unable to get adequate sleep, and isolating one's self (Portnoy, D., 2011).
Plan To Combat Compassion Fatigue And Burnout Essay Samples. Type of paper: Essay. Topic: Health, Nursing, Emotions, Stress, Adult, Adulthood, Spiritual, Breastfeeding. Pages: 4. Words: 1000. Published: 11/06/2021. Work burnout and stress are common phenomenon in a health care setting due to long work working hours, hostile clients, complexity ...
To study the level of compassion fatigue and compassion satisfaction experienced by mental health nurses. A descriptive, cross-sectional, electronic survey design was utilized. The Professional Quality of Life Scale-5 was used. The study was conducted at a large, urban hospital that exclusively treats patients with mental health and addiction ...
Prevent Compassion Fatigue Compassion fatigue has been referred to as "the cost of caring" for others in several fields of work -- notably healthcare, social work and other professions in which empathy and hands-on human assistance can lead to something close to burnout. Compassion fatigue is described as a "…stress response that emerges suddenly and without warning and includes a sense of ...
Compassion fatigue occurs when nurses unknowingly internalize the anxiety, trauma, and distress of their patients, further leading to nursing burnout. Burnout can be described as a prolonged response to physical and emotional stressors that result in feelings of exhaustion, a sense of being overwhelmed, insecurity, anxiety, cynicism, and ...
Submit an Essay Submit a Letter to the Editor ... While it is great to provide teachers with additional pay after school, when teachers express burnout and compassion fatigue, putting in hours ...