Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
- Methodology
- What Is a Cohort Study? | Definition & Examples

What Is a Cohort Study? | Definition & Examples
Published on February 24, 2023 by Tegan George .
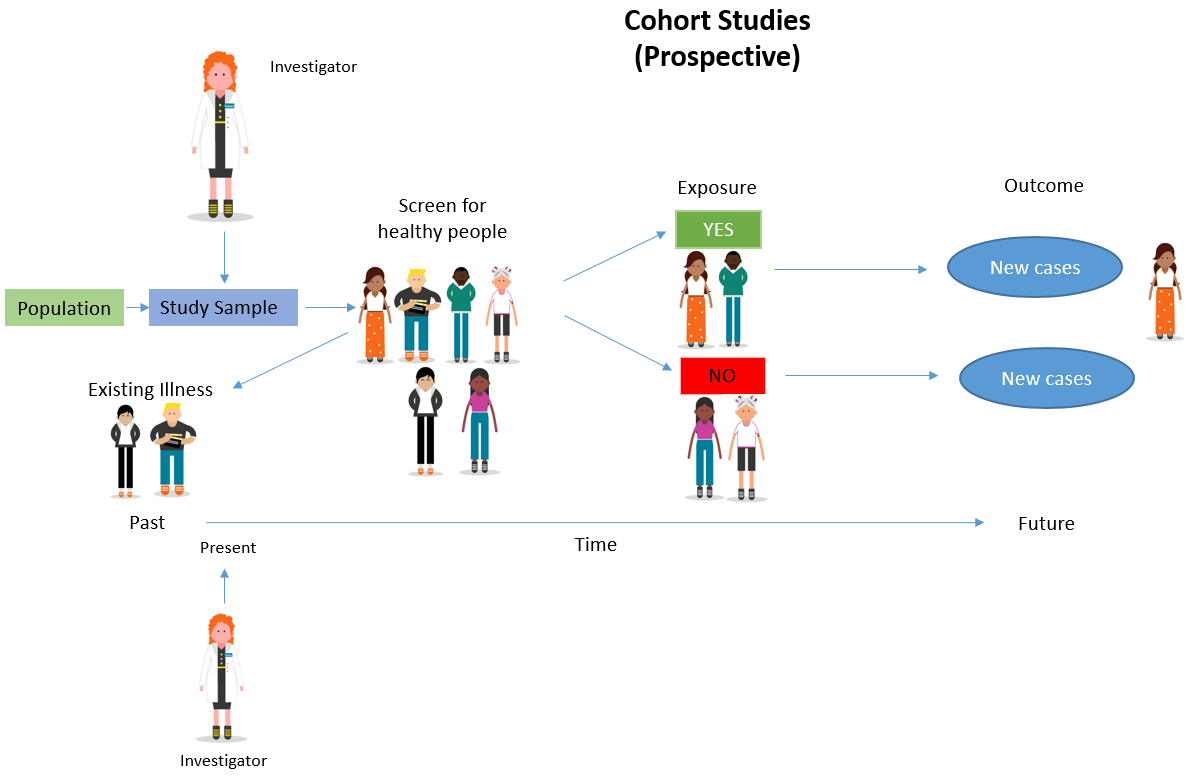
A cohort study is a type of observational study that follows a group of participants over a period of time, examining how certain factors (like exposure to a given risk factor) affect their health outcomes. The individuals in the cohort have a characteristic or lived experience in common, such as birth year or geographic area.
While there are several types of cohort study—including open, closed, and dynamic—there are two that are particularly common: prospective cohort studies and retrospective cohort studies .
The initial cohort consisted of about 18,000 newborns. They were enrolled in the study shortly after birth, with regular follow-ups, medical examinations, and cognitive assessments to track their physical, social, and cognitive development.
Cohort studies are particularly useful for identifying risk factors for diseases. They can help researchers identify potential interventions to help prevent or treat the disease, and are often used in fields like medicine or healthcare research.
Table of contents
When to use a cohort study, examples of cohort studies, advantages and disadvantages of cohort studies, frequently asked questions.
Cohort studies are a type of observational study that can be qualitative or quantitative in nature. They can be used to conduct both exploratory research and explanatory research depending on the research topic.
In prospective cohort studies , data is collected over time to compare the occurrence of the outcome of interest in those who were exposed to the risk factor and those who were not. This can help ascertain whether the risk factor could be associated with the outcome.
In retrospective cohort studies , your participants must already possess the disease or health outcome being studied prior to joining. The study is then focused on analyzing the health outcomes of those who share the exposure to the risk factor over a period of time.
A cohort study could be a good fit for your research if:
- You have access to a large pool of research subjects and are comfortable and able to fund research stretching over a longer timeline.
- The relationship between the exposure and health outcome you’re studying is not well understood, and/or its long-term effects have not been thoroughly investigated.
- The exposure you’re studying is rare, or there are possible ethical considerations preventing you from a traditional experimental design .
- Cohort studies in general are more longitudinal in nature. They usually follow the group studied over a long period of time, investigating how certain factors affect their health outcomes.
- Case–control studies rely on primary research , comparing a group of participants already possessing a condition of interest to a control group lacking that condition in real time.
Receive feedback on language, structure, and formatting
Professional editors proofread and edit your paper by focusing on:
- Academic style
- Vague sentences
- Style consistency
See an example

Cohort studies are common in fields like medicine, epidemiology, and healthcare.
Cohort studies are a strong research method , particularly in epidemiology, health, and medicine, but they are not without their disadvantages.
Advantages of cohort studies
Advantages of cohort studies include:
- Cohort studies are better able to approach an estimation of causality than other types of observational studies. Due to their ability to establish temporality, multiple outcomes, and disease incidence over time, researchers are able to determine with more certainty that the exposure indeed preceded the outcome. This strengthens a claim for a cause-and-effect relationship between the variables of interest.
- Due to their long nature, cohort studies are a particularly good choice for studying rare exposures , such as exposure to a new drug or an environmental toxin. Other research designs aren’t able to incorporate the breadth and depth of the impact as broadly as cohort studies do.
- Because cohort studies usually rely on large groups of participants, they are better able to control for potentially confounding variables , such as age, gender identity, or socioeconomic status. Relatedly, the ability to use a sampling method that ensures a more representative sample of the population leads to findings that are typically much more generalizable , with higher internal validity and external validity .
Disadvantages of cohort studies
Disadvantages of cohort studies include:
- Cohort studies can be extremely time-consuming and expensive to conduct due to their long and intense nature.
- Cohort studies are at risk for biases inherent to long-term studies like attrition bias and survivorship bias , as participants are likely to drop out over time. Measurement errors like omitted variable bias and information bias can also confound your analysis, leading you to draw conclusions that may not be true.
- Like many other experimental designs , cohort studies can raise questions regarding ethical considerations . This is particularly the case if the exposure of interest is harmful, or if there is no known treatment for it. Prior to beginning your research, it is critical to ensure that participation in your study is fully voluntary, informed, and as safe as it can be for your research subjects.
The easiest way to remember the difference between prospective and retrospective cohort studies is timing.
- A prospective cohort study moves forward in time, following a group of participants to track the development of an outcome of interest.
- A retrospective cohort study moves backward in time, first identifying a group of people who already possess the outcome of interest, and then looking backwards to assess their exposure to a risk factor.
A closed cohort study is a type of cohort study where all participants are selected at the beginning of the study, with no new participants added during any of the follow-up periods.
This approach is useful when the exposure being studied is rare, or when it isn’t practically or financially feasible to recruit new participants.
In a cohort study , the incidence refers to the number of new cases of a disease or health outcome that develop during the study period, while prevalence refers to the proportion of the population who have the disease or health outcome at a given point in time. Cohort studies are particularly useful for measuring incidence rates.
A dynamic cohort study is a type of cohort study where the participants are not fixed at the start of the study. Instead, new participants can be added over time if they become eligible to participate. This approach is useful when the study population is expected to change over time.
Sources in this article
We strongly encourage students to use sources in their work. You can cite our article (APA Style) or take a deep dive into the articles below.
George, T. (2023, February 24). What Is a Cohort Study? | Definition & Examples. Scribbr. Retrieved March 25, 2024, from https://www.scribbr.com/methodology/cohort-study/
Euser, A. M., Zoccali, C., Jager, K. J., & Dekker, F. W. (2009). Cohort Studies: Prospective versus Retrospective. Nephron Clinical Practice , 113 (3), c214–c217. https://doi.org/10.1159/000235241
Is this article helpful?
Tegan George
Other students also liked, what is a prospective cohort study | definition & examples, what is a retrospective cohort study | definition & examples, what is an observational study | guide & examples, what is your plagiarism score.
Quantitative study designs: Cohort Studies
Quantitative study designs.
- Introduction
- Cohort Studies
- Randomised Controlled Trial
- Case Control
- Cross-Sectional Studies
- Study Designs Home
Cohort Study
Did you know that the majority of people will develop a diagnosable mental illness whilst only a minority will experience enduring mental health? Or that groups of people at risk of having high blood pressure and other related health issues by the age of 38 can be identified in childhood? Or that a poor credit rating can be indicative of a person’s health status?
These findings (and more) have come out of a large cohort study started in 1972 by researchers at the University of Otago in New Zealand. This study is known as The Dunedin Study and it has followed the lives of 1037 babies born between 1 April 1972 and 31 March 1973 since their birth. The study is now in its fifth decade and has produced over 1200 publications and reports, many of which have helped inform policy makers in New Zealand and overseas.
In Introduction to Study Designs, we learnt that there are many different study design types and that these are divided into two categories: Experimental and Observational. Cohort Studies are a type of observational study.
What is a Cohort Study design?
- Cohort studies are longitudinal, observational studies, which investigate predictive risk factors and health outcomes.
- They differ from clinical trials, in that no intervention, treatment, or exposure is administered to the participants. The factors of interest to researchers already exist in the study group under investigation.
- Study participants are observed over a period of time. The incidence of disease in the exposed group is compared with the incidence of disease in the unexposed group.
- Because of the observational nature of cohort studies they can only find correlation between a risk factor and disease rather than the cause.
Cohort studies are useful if:
- There is a persuasive hypothesis linking an exposure to an outcome.
- The time between exposure and outcome is not too long (adding to the study costs and increasing the risk of participant attrition).
- The outcome is not too rare.
The stages of a Cohort Study
- A cohort study starts with the selection of a group of participants (known as a ‘cohort’) sourced from the same population, who must be free of the outcome under investigation but have the potential to develop that outcome.
- The participants must be identical, having common characteristics except for their exposure status.
- The participants are divided into two groups – the first group is the ‘exposure’ group, the second group is free of the exposure.
Types of Cohort Studies
There are two types of cohort studies: Prospective and Retrospective .
How Cohort Studies are carried out
Adapted from: Cohort Studies: A brief overview by Terry Shaneyfelt [video] https://www.youtube.com/watch?v=FRasHsoORj0)
Which clinical questions does this study design best answer?
What are the advantages and disadvantages to consider when using a cohort study, what does a strong cohort study look like.
- The aim of the study is clearly stated.
- It is clear how the sample population was sourced, including inclusion and exclusion criteria, with justification provided for the sample size. The sample group accurately reflects the population from which it is drawn.
- Loss of participants to follow up are stated and explanations provided.
- The control group is clearly described, including the selection methodology, whether they were from the same sample population, whether randomised or matched to minimise bias and confounding.
- It is clearly stated whether the study was blinded or not, i.e. whether the investigators were aware of how the subject and control groups were allocated.
- The methodology was rigorously adhered to.
- Involves the use of valid measurements (recognised by peers) as well as appropriate statistical tests.
- The conclusions are logically drawn from the results – the study demonstrates what it says it has demonstrated.
- Includes a clear description of the data, including accessibility and availability.
What are the pitfalls to look for?
- Confounding factors within the sample groups may be difficult to identify and control for, thus influencing the results.
- Participants may move between exposure/non-exposure categories or not properly comply with methodology requirements.
- Being in the study may influence participants’ behaviour.
- Too many participants may drop out, thus rendering the results invalid.
Critical appraisal tools
To assist with the critical appraisal of a cohort study here are some useful tools that can be applied.
Critical appraisal checklist for cohort studies (JBI)
CASP appraisal checklist for cohort studies
Real World Examples
Bell, A.F., Rubin, L.H., Davis, J.M., Golding, J., Adejumo, O.A. & Carter, C.S. (2018). The birth experience and subsequent maternal caregiving attitudes and behavior: A birth cohort study . Archives of Women’s Mental Health .
Dykxhoorn, J., Hatcher, S., Roy-Gagnon, M.H., & Colman, I. (2017). Early life predictors of adolescent suicidal thoughts and adverse outcomes in two population-based cohort studies . PLoS ONE , 12(8).
Feeley, N., Hayton, B., Gold, I. & Zelkowitz, P. (2017). A comparative prospective cohort study of women following childbirth: Mothers of low birthweight infants at risk for elevated PTSD symptoms . Journal of Psychosomatic Research , 101, 24–30.
Forman, J.P., Stampfer, M.J. & Curhan, G.C. (2009). Diet and lifestyle risk factors associated with incident hypertension in women . JAMA: Journal of the American Medical Association , 302(4), 401–411.
Suarez, E. (2002). Prognosis and outcome of first-episode psychoses in Hawai’i: Results of the 15-year follow-up of the Honolulu cohort of the WHO international study of schizophrenia . ProQuest Information & Learning, Dissertation Abstracts International: Section B: The Sciences and Engineering , 63(3-B), 1577.
Young, J.T., Heffernan, E., Borschmann, R., Ogloff, J.R.P., Spittal, M.J., Kouyoumdjian, F.G., Preen, D.B., Butler, A., Brophy, L., Crilly, J. & Kinner, S.A. (2018). Dual diagnosis of mental illness and substance use disorder and injury in adults recently released from prison: a prospective cohort study . The Lancet. Public Health , 3(5), e237–e248.
References and Further Reading
Greenhalgh, T. (2014). How to Read a Paper : The Basics of Evidence-Based Medicine , John Wiley & Sons, Incorporated, Somerset, United Kingdom.
Hoffmann, T. a., Bennett, S. P., & Mar, C. D. (2017). Evidence-Based Practice Across the Health Professions (Third edition. ed.): Elsevier.
Song, J.W. & Chung, K.C. (2010). Observational studies: cohort and case-control studies . Plastic and Reconstructive Surgery , 126(6), 2234-42.
Mann, C.J. (2003). Observational research methods. Research design II: cohort, cross sectional, and case-control studies . Emergency Medicine Journal , 20(1), 54-60.
- << Previous: Introduction
- Next: Randomised Controlled Trial >>
- Last Updated: Feb 29, 2024 4:49 PM
- URL: https://deakin.libguides.com/quantitative-study-designs
Prospective Cohort Study Design: Definition & Examples
Julia Simkus
Editor at Simply Psychology
BA (Hons) Psychology, Princeton University
Julia Simkus is a graduate of Princeton University with a Bachelor of Arts in Psychology. She is currently studying for a Master's Degree in Counseling for Mental Health and Wellness in September 2023. Julia's research has been published in peer reviewed journals.
Learn about our Editorial Process
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
On This Page:
A prospective study, sometimes called a prospective cohort study, is a type of longitudinal study where researchers will follow and observe a group of subjects over a period of time to gather information and record the development of outcomes.

The participants in a prospective study are selected based on specific criteria and are often free from the outcome of interest at the beginning of the study. Data on exposures and potential confounding factors are collected at regular intervals throughout the study period.
By following the participants prospectively, researchers can establish a temporal relationship between exposures and outcomes, providing valuable insights into the causality of the observed associations.
This study design allows for the examination of multiple outcomes and the investigation of various exposure levels, contributing to a comprehensive understanding of the factors influencing health and disease.
How it Works
Participants are enrolled in the study before they develop the outcome or disease in question and then are observed as it evolves to see who develops the outcome and who does not.
Cohort studies are observational, so researchers will follow the subjects without manipulating any variables or interfering with their environment.
Similar to retrospective studies , prospective studies are beneficial for medical researchers, specifically in the field of epidemiology, as scientists can watch the development of a disease and compare the risk factors among subjects.
Before any appearance of the disease is investigated, medical professionals will identify a cohort, observe the target participants over time, and collect data at regular intervals.
Weeks, months, or years later, depending on the duration of the study design, the researchers will examine any factors that differed between the individuals who developed the condition and those who did not.
They can then determine if an association exists between an exposure and an outcome and even identify disease progression and relative risk.
Determine cause-and-effect relationships
Because researchers study groups of people before they develop an illness, they can discover potential cause-and-effect relationships between certain behaviors and the development of a disease.
Multiple diseases and conditions can be studied at the same time
Prospective cohort studies enable researchers to study causes of disease and identify multiple risk factors associated with a single exposure. These studies can also reveal links between diseases and risk factors.
Can measure a continuously changing relationship between exposure and outcome
Because prospective cohort studies are longitudinal, researchers can study changes in levels of exposure over time and any changes in outcome, providing a deeper understanding of the dynamic relationship between exposure and outcome.
Limitations
Time consuming and expensive.
Prospective studies usually require multiple months or years before researchers can identify a disease’s causes or discover significant results.
Because of this, they are often more expensive than other types of studies. Recruiting and enrolling participants is another added cost and time commitment.
Requires large subject pool
Prospective cohort studies require large sample sizes in order for any relationships or patterns to be meaningful. Researchers are unable to generate results if there is not enough data.
- Framingham Heart Study: Studied the effects of diet, exercise, and medications on the development of hypertensive or arteriosclerotic cardiovascular disease in residents of the city of Framingham, Massachusetts.
- Caerphilly Heart Disease Study: Examined relationships between a wide range of social, lifestyle, dietary, and other factors with incident vascular disease.
- The Million Women Study: Analyzed data from more than one million women aged 50 and over to understand the effects of hormone replacement therapy use on women’s health.
- Nurses’ Health Study: Studied the effects of diet, exercise, and medications on the development of hypertensive or arteriosclerotic cardiovascular disease.
- Sleep-Disordered Breathing and Mortality: Determined whether sleep-disordered breathing and its sequelae of intermittent hypoxemia and recurrent arousals are associated with mortality in a community sample of adults aged 40 years or older (Punjabi et al., 2009)
Frequently Asked Questions
1. what does it mean when an observational study is prospective.
A prospective observational study is a type of research where investigators select a group of subjects and observe them over a certain period.
The researchers collect data on the subjects’ exposure to certain risk factors or interventions and then track the outcomes. This type of study is often used to study the effects of suspected risk factors that cannot be controlled experimentally.
2. What is the primary difference between a randomized clinical trial and a prospective cohort study?
In a retrospective study, the subjects have already experienced the outcome of interest or developed the disease before the start of the study.
The researchers then look back in time to identify a cohort of subjects before they had developed the disease and use existing data, such as medical records, to discover any patterns.
In a prospective study, on the other hand, the investigators will design the study, recruit subjects, and collect baseline data on all subjects before any of them have developed the outcomes of interest.
The subjects are followed and observed over a period of time to gather information and record the development of outcomes.
3. What is the primary difference between a randomized clinical trial and a prospective cohort study?
In randomized clinical trials , the researchers control the experiment, whereas prospective cohort studies are purely observational, so researchers will observe subjects without manipulating any variables or interfering with their environment.
Researchers in randomized clinical trials will randomly divide participants into groups, either an experimental group or a control group.
However, in prospective cohort studies, researchers will identify a cohort and observe the target participants as a whole to examine any factors that differ between the individuals who develop the condition and those who do not.
Euser, A. M., Zoccali, C., Jager, K. J., & Dekker, F. W. (2009). Cohort studies: prospective versus retrospective. Nephron. Clinical practice, 113(3), c214–c217. https://doi.org/10.1159/000235241
Hariton, E., & Locascio, J. J. (2018). Randomised controlled trials – the gold standard for effectiveness research: Study design: randomised controlled trials. BJOG : an international journal of obstetrics and gynaecology, 125(13), 1716. https://doi.org/10.1111/1471-0528.15199
Netherlands Cooperative Study on the Adequacy of Dialysis-2 Study Group de Mutsert Renée r. de_mutsert@ lumc. nl Grootendorst Diana C Boeschoten Elisabeth W Brandts Hans van Manen Jeannette G Krediet Raymond T Dekker Friedo W. (2009). Subjective global assessment of nutritional status is strongly associated with mortality in chronic dialysis patients. The American journal of clinical nutrition, 89(3), 787-793.
Punjabi, N. M., Caffo, B. S., Goodwin, J. L., Gottlieb, D. J., Newman, A. B., O”Connor, G. T., Rapoport, D. M., Redline, S., Resnick, H. E., Robbins, J. A., Shahar, E., Unruh, M. L., & Samet, J. M. (2009). Sleep-disordered breathing and mortality: a prospective cohort study. PLoS medicine, 6(8), e1000132. https://doi.org/10.1371/journal.pmed.1000132
Ranganathan, P., & Aggarwal, R. (2018). Study designs: Part 1 – An overview and classification. Perspectives in clinical research, 9(4), 184–186.
Song, J. W., & Chung, K. C. (2010). Observational studies: cohort and case-control studies. Plastic and reconstructive surgery, 126(6), 2234–2242. https://doi.org/10.1097/PRS.0b013e3181f44abc.
Further Information
- Euser, A. M., Zoccali, C., Jager, K. J., & Dekker, F. W. (2009). Cohort studies: prospective versus retrospective. Nephron Clinical Practice, 113(3), c214-c217.
- Design of Prospective Studies
- Hammoudeh, S., Gadelhaq, W., & Janahi, I. (2018). Prospective cohort studies in medical research (pp. 11-28). IntechOpen.
- Nabi, H., Kivimaki, M., De Vogli, R., Marmot, M. G., & Singh-Manoux, A. (2008). Positive and negative affect and risk of coronary heart disease: Whitehall II prospective cohort study. Bmj, 337.
- Bramsen, I., Dirkzwager, A. J., & Van der Ploeg, H. M. (2000). Predeployment personality traits and exposure to trauma as predictors of posttraumatic stress symptoms: A prospective study of former peacekeepers. American Journal of Psychiatry, 157(7), 1115-1119.
How to choose your study design
Affiliation.
- 1 Department of Medicine, Sydney Medical School, Faculty of Medicine and Health, University of Sydney, Sydney, New South Wales, Australia.
- PMID: 32479703
- DOI: 10.1111/jpc.14929
Research designs are broadly divided into observational studies (i.e. cross-sectional; case-control and cohort studies) and experimental studies (randomised control trials, RCTs). Each design has a specific role, and each has both advantages and disadvantages. Moreover, while the typical RCT is a parallel group design, there are now many variants to consider. It is important that both researchers and paediatricians are aware of the role of each study design, their respective pros and cons, and the inherent risk of bias with each design. While there are numerous quantitative study designs available to researchers, the final choice is dictated by two key factors. First, by the specific research question. That is, if the question is one of 'prevalence' (disease burden) then the ideal is a cross-sectional study; if it is a question of 'harm' - a case-control study; prognosis - a cohort and therapy - a RCT. Second, by what resources are available to you. This includes budget, time, feasibility re-patient numbers and research expertise. All these factors will severely limit the choice. While paediatricians would like to see more RCTs, these require a huge amount of resources, and in many situations will be unethical (e.g. potentially harmful intervention) or impractical (e.g. rare diseases). This paper gives a brief overview of the common study types, and for those embarking on such studies you will need far more comprehensive, detailed sources of information.
Keywords: experimental studies; observational studies; research method.
© 2020 Paediatrics and Child Health Division (The Royal Australasian College of Physicians).
- Case-Control Studies
- Cross-Sectional Studies
- Research Design*
- Search Menu
- Advance Articles
- Editor's Choice
- Braunwald's Corner
- ESC Guidelines
- EHJ Dialogues
- Issue @ a Glance Podcasts
- CardioPulse
- Weekly Journal Scan
- European Heart Journal Supplements
- Year in Cardiovascular Medicine
- Asia in EHJ
- Most Cited Articles
- ESC Content Collections
- Author Guidelines
- Submission Site
- Why publish with EHJ?
- Open Access Options
- Submit from medRxiv or bioRxiv
- Author Resources
- Self-Archiving Policy
- Read & Publish
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Journals Career Network
- About European Heart Journal
- Editorial Board
- About the European Society of Cardiology
- ESC Publications
- War in Ukraine
- ESC Membership
- ESC Journals App
- Developing Countries Initiative
- Dispatch Dates
- Terms and Conditions
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, conclusions, acknowledgements, supplementary data, declarations, data availability, ethical approval, pre-registered clinical trial number.
- < Previous
Human papillomavirus infection and cardiovascular mortality: a cohort study
Yoosoo Chang and Seungho Ryu contributed equally as co-corresponding authors.
- Article contents
- Figures & tables
- Supplementary Data
Hae Suk Cheong, Yoosoo Chang, Yejin Kim, Min-Jung Kwon, Yoosun Cho, Bomi Kim, Eun-Jeong Joo, Young Ho Bae, Chanmin Kim, Seungho Ryu, Human papillomavirus infection and cardiovascular mortality: a cohort study, European Heart Journal , Volume 45, Issue 12, 21 March 2024, Pages 1072–1082, https://doi.org/10.1093/eurheartj/ehae020
- Permissions Icon Permissions
High-risk human papillomavirus (HR-HPV) infection—a well-established risk factor for cervical cancer—has associations with cardiovascular disease (CVD). However, its relationship with CVD mortality remains uncertain. This study examined the associations between HR-HPV infection and CVD mortality.
As part of a health examination, 163 250 CVD-free Korean women (mean age: 40.2 years) underwent HR-HPV screening and were tracked for up to 17 years (median: 8.6 years). National death records identified the CVD mortality cases. Hazard ratios (HRs) and 95% confidence intervals (CIs) for CVD mortality were estimated using Cox proportional hazard regression analyses.
During 1 380 953 person-years of follow-up, 134 CVD deaths occurred, with a mortality rate of 9.1 per 10 5 person-years for HR-HPV(−) women and 14.9 per 10 5 person-years for HR-HPV(+) women. After adjustment for traditional CVD risk factors and confounders, the HRs (95% CI) for atherosclerotic CVD (ASCVD), ischaemic heart disease (IHD), and stroke mortality in women with HR-HPV infection compared with those without infection were 3.91 (1.85–8.26), 3.74 (1.53–9.14), and 5.86 (0.86–40.11), respectively. The association between HR-HPV infection and ASCVD mortality was stronger in women with obesity than in those without ( P for interaction = .006), with corresponding HRs (95% CI) of 4.81 (1.55–14.93) for obese women and 2.86 (1.04–7.88) for non-obese women.
In this cohort study of young and middle-aged Korean women, at low risks for CVD mortality, those with HR-HPV infection had higher death rates from CVD, specifically ASCVD and IHD, with a more pronounced trend in obese individuals.

High-risk human papillomavirus infection and cardiovascular mortality. HR, hazard ratio; HR-HPV, high-risk human papillomavirus infection; CI, confidence interval; BMI, body mass index; CVD, cardiovascular disease.
See the editorial comment for this article ‘Human papilloma virus and atherosclerotic cardiovascular disease’, by N.C. Chan, https://doi.org10.1093/eurheartj/ehad829 .
Cardiovascular diseases (CVDs) are the world’s leading cause of death, accounting for an estimated 17.9 million deaths (32% of all global deaths) in 2019, with this number projected to increase to 23.6 million by 2030. 1–3 Despite considerable advancements in the management strategies targeting conventional CVD risk factors, such as cigarette smoking, dyslipidaemia, high blood pressure, and diabetes, CVD remains a leading cause of death and disability. 3–6 Furthermore, these conventional risk factors alone do not completely explain the high incidence and prevalence of CVD, 3 with ∼20% of CVD cases lacking these conventional risk factors. 7 Identifying modifiable non-conventional risk factors of CVD is, therefore, crucial in developing optimal preventive and treatment strategies for reducing CVD.
Human papillomavirus (HPV) is a sexually transmitted infection, 8 with a prevalence rate of 2%–44% in the general female population. 9 High-risk strains of HPV (HR-HPV) infection are well-established causative agents of anogenital cancers in women. 10 Several cross-sectional studies have suggested a possible association between HR-HPV and atherosclerotic CVD (ASCVD). 9 , 11 Our recent prospective cohort study supports this association in new-onset CVD. 12 However, no cohort studies have evaluated the long-term CVD outcomes associated with HR-HPV infection.
Understanding the contribution of HR-HPV infection to long-term cardiovascular consequences in women with HPV may have important clinical significance, particularly considering the availability of HPV vaccines. 13 Thus, we conducted a large-scale cohort study of Korean women who underwent a HR-HPV test as part of a health screening programme to verify our hypothesis that HR-HPV infection in women is associated with increased CVD mortality, with potential effect modification by obesity.
Study design and participants
The Kangbuk Samsung Health Study is a cohort study of Korean adults aged 18 years or older who underwent annual or biennial health examinations at the Kangbuk Samsung Hospital Total Healthcare Centers in Seoul and Suwon, South Korea. 12 , 14 Data were collected as part of health screening examinations, which included questionnaires, blood tests, and imaging examinations. 14
The study population comprised women aged ≥30 years who underwent a comprehensive health screening examination between 2004 and 2018 ( n = 178 854). The final sample size was 163 250 after we excluded 15 604 participants who met the following criteria ( Figure 1 ): unknown vital status due to invalid identifiers, missing data on body mass index (BMI), blood pressure, lipid profiles, glucose, insulin, or high-sensitivity C-reactive protein (hsCRP) levels, as well as history of CVD, hysterectomy, or cancer.

Selection process of the study population
The requirement for written informed consent was waived due to the use of de-identified data obtained as part of routine health screening examinations. This study was approved by the institutional review board of Kangbuk Samsung Hospital (KBSMC 2022-05-029).
Measurements
Demographic characteristics, health behaviours, medical history, and medication use were assessed as a basic part of the health examinations using standardized, self-administered questionnaires, as previously described. 14 Smoking status was classified as never, former, or current. Alcohol consumption was categorized as ≤20 or >20 g/day. Regular exercise was defined as engaging in vigorous physical activity at least three times per week. 14 , 15 The assessment of weekly vigorous physical activity frequency varied over time: (i) from 2004 to 2008, it was based on activities inducing perspiration; (ii) in 2009–10, it focused on vigorous activities like running, aerobics, fast bicycling, or hiking that made participants breathe much harder than normal; and (iii) starting in 2011, the validated Korean version of the International Physical Activity Questionnaire Short Form was used for this assessment. 16 , 17 A high level of education is characterized by having a college graduate degree or higher.
Trained nurses measured the participants’ height, weight, and blood pressure. Obesity was defined as a BMI ≥ 25 kg/m 2 according to Asian-specific criteria. 18 Hypertension was defined based on systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or the current use of blood pressure–lowering medications.
Blood samples were drawn from the antecubital vein after a minimum 10 h fast. Blood tests included total cholesterol, HDL cholesterol (HDL-C), LDL cholesterol (LDL-C), triglycerides, alanine transaminase (ALT), fasting glucose, insulin, and hsCRP. The homeostasis model assessment of insulin resistance (HOMA-IR) was calculated as fasting insulin (mg/dL) × fasting glucose (mg/dL)/405. Diabetes mellitus was assessed according to fasting serum glucose levels ≥126 mg/dL, glycated haemoglobin levels ≥6.5%, self-reports of a previous diagnosis, or the use of blood glucose–lowering agents.
High-risk human papillomavirus tests were performed as part of cervical cancer screening, using cervical specimens, and all samples were analysed in a core laboratory located at Kangbuk Samsung hospital. 12 From 2004 until April 2016, the HR Hybrid Capture 2 assay (Qiagen, Gaithersburg, MD, USA) was used for HR-HPV testing, following the manufacturer’s protocol. The HR Hybrid Capture 2 is a sandwich-capture molecular hybridization assay that utilizes chemiluminescence detection to provide a semi-quantitative result. Specifically, the assay denatures HPV DNA and then hybridizes single-stranded HPV DNA with a mixture of single-stranded, full-genomic-length RNA probes that are specific for 13 HR-HPV genotypes (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, and 68). The results were considered negative if the measurements were below the relative light-unit cut-off of 1.0. After April 2016, the Roche Cobas HPV assay was used for HR-HPV testing. This is a fully automated real-time polymerase chain reaction (PCR) assay that involves DNA extraction and purification using a Cobas ×480 Instrument (Roche Molecular Systems, Rotkreuz, Switzerland), followed by real-time PCR amplification and type-specific hybridization that is performed by the Cobas z480 Analyzer (Roche Molecular Systems). The assay utilizes a mixture of primer pairs and probes to amplify and detect the 14 HR-HPV DNAs. The results were considered as positive when the cycle threshold was <40.0. The result is reported as either negative or positive for HPV16 and HPV18 and as a pooled result for the other 12 HR-HPVs (31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68). To maintain quality control (QC), two QC materials with positive and negative controls provided by the manufacturer were included in each run. Moreover, prior to replacing an obsolete analyser with a new one in the laboratory, a performance evaluation was conducted to ensure that the samples could be successfully validated for precision and comparisons of quantitative measurements based on the Clinical and Laboratory Standards Institute guidelines EP5 and EP12-A2. During the majority of study periods, the measurement of HR-HPV did not differentiate between Types 16 and 18 and the other HR-HPV types. Therefore, for the analysis, HR-HPV positivity was categorized as binary (HR-HPV negative vs. HR-HPV positive). Both HR-HPV testing procedures in this study were approved by the US Food and Drug Administration for HR-HPV screening and were subjected to rigorous QC measures to ensure accuracy and reliability of the results. 19
The Framingham Risk Score (FRS) was calculated based on age, smoking status (current, past, or never), diabetes mellitus (absence or presence), systolic blood pressure (mmHg), HDL-C concentration (mg/dL), and total cholesterol concentration (mg/dL). The 10-year risk of developing CVD was considered low if the result was <10%. 20
Mortality follow-up
We followed up on mortality until the end of 2020 using nationwide death certificate data from the Korea National Statistical Office. Because all deaths of Koreans must be reported to the Korea National Statistical Office, death certificate data for Korean adults are virtually complete. To determine the cause of death, we used the single most relevant underlying cause of death as identified by the Korean National Statistical Office and classified according to the International Classification of Diseases (10th revision) (ICD-10). The concordance rate between the causes of death listed on death certificates and the patient diagnoses in the medical utilization data was in the range of 72.2%–91.9%. 21 , 22 Circulatory system disease ICD-10 I00–I99 was used to define CVD mortality, while ASCVD mortality was defined by ICD-10 I20–I25, I63–I64, G45, and I70–I74. The mortality data were further divided into the following causes of death: ischaemic heart disease (IHD, I20–25); ischaemic stroke [I63–64, no death caused due to transient cerebral ischaemic attacks (G45)]; peripheral artery disease (I70–I74); and other CVDs except for ASCVD (I codes except for the ASCVD codes stated above). 23 , 24
Statistical analysis
The primary endpoint was CVD mortality, including its subtypes. We followed each participant from their baseline examination until the occurrence of CVD death or until the end of 2020, whichever occurred first. Participants who died of other causes were censored on the date of death. Cox proportional hazard regression analyses were used to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) for CVD mortality. Using age as the timescale, the age of subjects was recorded at their first health check-up exam (left truncation) and the age at which subjects exited the analysis, either at the time of death or on 31 December 2020. The proportional hazards assumption was assessed by examining the graphs of the estimated log–log survival; no violation of the assumption was found.
Initially, the models were adjusted for age (timescale), and then, these were further adjusted for confounding variables between HR-HPV and CVD mortality, including the centre attended (Seoul or Suwon); year of screening exam; BMI; smoking (never, past, current, or unknown); alcohol intake (0, <20, ≥20 g/day, or unknown); regular exercise (no, yes, or unknown); education level (<community college graduate, ≥community college graduate, or unknown); history of diabetes; history of hypertension; and lipid-lowering medication use (Model 1). Model 2 was further adjusted for triglycerides, LDL-C, HDL-C, HOMA-IR, and hsCRP. As obesity is associated with an increased risk of HPV infection or its persistence, 25 , 26 to examine whether the associations between HR-HPV and CVD mortality differ according to the presence of obesity, we performed a stratified analysis according to the presence of obesity (defined as a BMI ≥ 25 kg/m 2 according to Asian-specific criteria). Furthermore, an additional analysis stratified according to FRS categories (FRS < 10% vs. FRS ≥ 10% 20 ) was performed to assess whether the associations are modified by traditional cardiovascular risk factors.
To account for competing risks, a counterfactual framework to define the marginal cumulative incidence (net risk) was employed, which represents the risk under elimination of competing events. 27 This estimation was carried out using the parametric g -formula method. In this assessment, we examined each distinct cause of death separately, while considering deaths unrelated to the specific cause as alternative competing risks. For instance, when assessing cardiovascular deaths through the g -formula approach, non-cardiovascular deaths were treated as competing risks.
To address the potential imbalance in characteristics between participants with and without HPV infection and enhance comparability between the two groups, we calculated the propensity score for HPV infection. These individual scores were then utilized to more effectively address the existing imbalance between the two groups. 28 , 29 We employed two analytical approaches: inverse probability weights (IPWs) and covariate adjustment using propensity scores. 28 We estimated the probability of HPV infection as a function of the baseline characteristics and used these probabilities to assign weights to each individual in the analysis. Each individual was weighted by the inverse of the predicted probability of HPV infection.
We conducted a sensitivity analysis including data from women with a history of cervical cancer who had undergone HPV testing, despite being initially excluded from the main analysis due to the potential removal of the cervix (which is the primary site of HPV infection) via hysterectomy.
Statistical analyses were performed using STATA version 17.0 software (StataCorp LP, College Station, TX, USA) and R version 4.3.0. All reported P -values were two-tailed, with P < .05 considered statistically significant.
The mean age ± standard deviation (SD) and mean BMI ± SD of the 163 250 participants were 40.2 ± 9.7 years and 22.0 ± 3.1 kg/m 2 , respectively. The prevalence rate of HR-HPV infections was 9.2%. High-risk human papillomavirus infection was positively associated with age, current smoking status, alcohol intake, regular exercise, history of hypertension, history of diabetes, blood pressure, HDL-C, ALT, and HOMA-IR, whereas it was inversely associated with education level, use of lipid-lowering medications, LDL-C, and hsCRP ( Table 1 ).
Estimated a mean values (95% confidence interval) and adjusted a proportions (95% confidence interval) of the baseline characteristics of the study participants according to high-risk human papillomavirus status
CI, confidence interval; HPV, human papillomavirus; BMI, body mass index; CVD, cerebrovascular disease; BP, blood pressure; LDL-C, LDL cholesterol; HDL-C, HDL cholesterol; ALT, alanine aminotransferase; hsCRP, high-sensitivity C-reactive protein; HOMA-IR, homeostasis model assessment of insulin resistance.
a Adjusted for age.
b BMI ≥ 25 kg/m 2 .
c ≥20 g of ethanol per day.
d ≥3 times per week.
e ≥College graduate.
Table 2 shows the association between HR-HPV positivity and CVD mortality rates. During 1 380 953 person-years of follow-up, 134 CVD deaths occurred, resulting in a mortality rate of 9.7 per 10 5 person-years (refer to Supplementary data online , Table S1 for specific disease code information related to CVD deaths). The median follow-up was 8.6 years (inter-quartile range: 5.4–11.5). High-risk human papillomavirus infection was significantly associated with an increased risk of ASCVD and IHD mortality; however, no significant association was observed between HR-HPV infection and mortality due to ischaemic stroke or other forms of CVD, aside from ASCVD ( Figure 2 ). The multivariable-adjusted HRs (95% CI) for ASCVD and IHD mortality were 3.56 (1.67–7.56) and 3.36 (1.37–8.25), respectively, for participants who were HR-HPV–positive compared with those who were HR-HPV–negative. Upon additional adjustment for triglycerides, LDL-C, HDL-C, HOMA-IR, and hsCRP, the associations remained consistent. Treating HR-HPV and potential confounders as time-varying variables resulted in stronger associations between HR-HPV infections and overall circulatory system disease, ASCVD, and IHD mortality compared with those of time-fixed models ( Table 2 ). In our study, where we conducted five separate tests, we applied Bonferroni adjustment, considering a score as significant only if the corresponding P -value was ≤α/5. The association between HR-HPV and ASCVD/IHD mortality remained significant, even after Bonferroni correction (see Supplementary data online , Table S2 ).

A Kaplan–Meier curve of cumulative mortality of cardiovascular disease mortality by human papillomavirus positivity: ( A ) circulatory system disease, ( B ) atherosclerotic cardiovascular disease, ( C ) ischaemic heart disease, ( D ) ischaemic stroke, and ( E ) other circulatory system diseases except for atherosclerotic cardiovascular disease. CVD, cardiovascular disease; HPV, human papillomavirus; ASCVD, atherosclerotic cardiovascular disease; IHD, ischaemic heart disease
Hazard ratios (95% confidence interval) for cardiovascular disease mortality according to high-risk human papillomavirus status
HPV, human papillomavirus; ASCVD, atherosclerotic cardiovascular disease; IHD, ischaemic heart disease; BMI, body mass index; LDL-C, LDL cholesterol; HDL-C, HDL cholesterol; HOMA-IR, homeostasis model assessment of insulin resistance; hsCRP, high-sensitivity C-reactive protein.
a Estimated from the Cox proportional hazards model with age as a timescale to estimate HRs and 95% CIs. The multivariable model was adjusted for age (timescale), centre, year of screening examination, smoking status, alcohol consumption, regular exercise, BMI, education level, history of diabetes, history of hypertension, and use of medication for hyperlipidaemia; Model 2: the same factors used in Model 1 plus an adjustment for triglycerides, LDL-C, HDL-C, HOMA-IR, and hsCRP.
b Estimated from the proportional hazard model with HPV status, smoking, alcohol consumption, regular exercise, BMI, history of diabetes, history of hypertension, and use of medication for hyperlipidaemia as time-dependent categorical variables and baseline sex, centre, year of screening, and education level as time-fixed variables.
In the counterfactual framework for the marginal cumulative incidence (net risk), the risk under HR-HPV infection for ASCVD mortality was significantly higher than the risk without HR-HPV infection (see Supplementary data online , Table S3 and Figure S1 ). Specifically, risk differences (%) at year 10 were as follows: 0.080 (95% CI: 0.018–0.250) for ASCVD mortality, 0.036 (95% CI: 0.000–0.115) for IHD mortality, and 0.014 (95% CI: −0.006–0.104) for ischaemic stroke mortality.
In sensitivity analyses using propensity score, the results obtained using either IPWs or covariate adjustment were found to be very similar to those obtained without using propensity score analyses (see Supplementary data online , Table S4 ). In sensitivity analyses including women with a history of cervical cancer, the prevalence of HPV infection was 11.2%, which was higher compared with that of the group without a history of cervical cancer (9.2%). In this analysis, no cardiovascular deaths occurred among the women with cervical cancer. The results, including those with a history of cervical cancer, yielded similar findings. Notably, the association between HR-HPV infection and ASCVD mortality remained statistically significant (see Supplementary data online , Table S5 ).
When stratified by obesity status, a trend was observed towards stronger associations between HR-HPV and CVD mortality (especially ASCVD mortality) in the obese group (defined as BMI ≥ 25 kg/m 2 ) compared with the non-obese group. The multivariable-adjusted HR (95% CI) for ASCVD mortality when comparing HR-HPV–positive participants with HR-HPV–negative participants was 4.81 (1.55–14.93) in the obese group, whereas the corresponding HR (95% CI) was 2.86 (1.04–7.88) in the non-obese group ( P for interaction = .006; Table 3 and Figure 3 ). No such patterns were observed for mortality from other forms of CVD, aside from ASCVD.

A Kaplan–Meier curve of cumulative mortality of atherosclerotic cardiovascular disease mortality by human papillomavirus positivity among ( A ) non-obese and ( B ) obese women. CVD, cardiovascular disease; HPV, human-papillomavirus; ASCVD, atherosclerotic cardiovascular disease; IHD, ischaemic heart disease
Hazard ratios (95% confidence interval) for cardiovascular disease mortality according to high-risk human papillomavirus status by obesity
CI, confidence interval; HPV, human papillomavirus; HR, hazard ratio; ASCVD, atherosclerotic cardiovascular disease; IHD, ischaemic heart disease.
a Estimated using the Cox proportional hazards model with age as a timescale to estimate HRs and 95% CIs. The multivariate model was adjusted for age (timescale), centre, year of screening examination, smoking status, alcohol consumption, regular exercise, education level, history of diabetes, history of hypertension, and use of medication for hyperlipidaemia.
When stratified by FRS (FRS < 10% and FRS ≥ 10%, see Supplementary data online , Table S6 ), significantly elevated risks of ASCVD and IHD mortality were found in individuals positive for HR-HPV, regardless of their FRS group.
In this large-scale cohort study of 163 250 apparently healthy young and middle-aged women without pre-existing CVD, the absolute risks of CVD mortality were low. However, those with HR-HPV infection had a higher rate of deaths attributed to CVD mortality, specifically ASCVD and IHD mortality. These associations remained significant even after adjusting for CVD risk factors and other possible confounders. The strength of this association was greater in women with obesity, indicating that the relationship between HR-HPV infection and CVD mortality may be modified by obesity ( Structured Graphical Abstract ).
Recent research has expanded its focus beyond HPV’s association with cancer development, and accumulating epidemiological evidence suggests that HPV is associated with CVD risk. A cross-sectional study conducted in the USA found that women with genital HPV infection, especially HR-HPV, had a nearly three-fold higher history of myocardial infarction or stroke compared with that in women without HPV. 11 However, this study was limited by their cross-sectional design, use of self-collected samples of HPV, and/or reliance on self-reported outcome data. Another study found that patients with head and neck cancer who tested positive for HPV had a four-fold increased risk of stroke. 30 In a previous cohort study, we demonstrated that young Korean women infected with HR-HPV, as ascertained by clinician-collected samples, were at elevated risk of CVD events, especially those who were obese and metabolically unhealthy. 12 Nonetheless, no studies have examined the association between HR-HPV and long-term CVD outcomes to our knowledge. The present study extends our earlier work on HR-HPV and CVD by demonstrating that HR-HPV infection is associated with an increased risk of CVD mortality, particularly due to ASCVD or IHD. We did not directly examine the association among HPV infection, non-fatal CVD, and CVD mortality within a single dataset. However, the collective evidence from these two studies suggests that HPV infection may indeed act as a risk factor for the development of non-fatal CVD and contribute to poor prognosis, ultimately leading to CVD mortality. Several factors contribute to an elevated risk of cardiovascular mortality. Firstly, HPV is not recognized as a cardiovascular risk factor, and effective strategies for managing HPV infections in relation to cardiovascular complications are lacking. Additionally, there is a notable absence of antiviral drugs designed specifically for HPV treatment as well as a lack of pharmaceutical interventions targeting inflammation, which is a potential mechanism through which HPV increases cardiovascular events.
Chronic infection has emerged as a non-conventional risk factor of unexplained cardiovascular events, and recent studies suggest that it may play a role in the development of atherosclerosis. 13 , 31 Recently, severe acute respiratory syndrome coronavirus-2 has been shown to cause direct myocardial injury, and worsen pre-existing CVD, potentially leading to an increased risk of cardiovascular complications and mortality. 32 , 33 Although there is relatively limited evidence on the relationship between HR-HPV and atherosclerotic processes compared with other viral pathogens, our findings support the notion that the connection between HPV and increased CVD risks is likely mediated by the involvement of HPV in ASCVD. 34 HPV may promote atherogenesis by infecting vascular cells or non-vascular cells and inducing systemic inflammation. 35–37 Contrary to the traditional belief that HPV replicates only locally and has limited systemic effects, several reports have demonstrated that HPV DNA can be isolated from white blood cells in circulating blood, both in healthy blood donors and patients with HPV-associated cancers; thus, this suggests that HPV may reach arterial structures via the bloodstream. 35 , 38 , 39 HPV infection may also accelerate atherogenesis by eliciting a persistent inflammatory response and systemic inflammation. 35–37
In our study, the association between HR-HPV and ASCVD mortality remained even after adjustment for hsCRP levels (a well-established low-grade inflammatory biomarker) and lipid profiles (including triglycerides, LDL-C, and HDL-C levels). Although it is uncertain whether the observed associations are due to effects beyond inflammation, hsCRP (despite being a predictor of atherosclerotic risk) is unlikely to be causally involved in atherogenic pathways. 40 While the inflammatory role in CVD is crucial, 41 investigating the mechanistic pathogenesis of CVD based on the inflammatory hypothesis of atherosclerosis suggests that gaining insights by moving upstream in the inflammatory cascade from hsCRP to interleukin (IL)-6 to IL-1 could be valuable. 42 Indeed, clinical trials and mechanistic studies suggest that colchicine and other anti-inflammatory agents targeting upstream inflammatory markers, such as IL-1 and IL-6, have potential atheroprotective effects. 42–44 Thus, future research should explore upstream markers (such as IL-1 and IL-6) to gain a better understanding of the connection among HR-HPV, inflammation, atherosclerotic progression, and CVD mortality.
The present study found a stronger association between HR-HPV and CVD mortality in obese individuals compared with that in non-obese individuals, which is consistent with our previous study results where obesity modified the association between HR-HPV and incident CVD. 12 The mechanisms explaining this association have been previously discussed, 12 with suggestions including compromised immune responses to HPV infection due to obesity-associated metabolic abnormalities and obesity-induced systemic inflammation, which exacerbate the atherosclerotic process and contribute to the risk of CVD and CVD mortality in conjunction with HPV. 45 , 46
In the stratified analyses based on the FRS, the excess relative risks of ASCVD and IHD mortality in HPV-positive individuals with respect to HPV-negative individuals were similar in both the FRS < 10% and FRS ≥ 10% groups, with a four-fold increase in risk. Thus, based on traditional risk factors, HR-HPV infection poses an additional risk of CVD mortality, even in low-risk individuals. Particularly, the limitations of the FRS include the underestimation of coronary heart disease risk in women, in whom up to 20% of coronary artery diseases that occur are unrelated to these traditional risk factors. 7 , 47 The observed associations between HR-HPV and ASCVD mortality, strongly modified by obesity than by the conventional risk factors assessed by the FRS, suggest that chronic systemic inflammation may constitute a key pathogenic mechanism in HPV–CVD dynamics, 34 as inflammation is also a primary mediator linking obesity and CVD. 48 Further mechanistic studies are required to confirm these findings.
In sensitivity analyses including women with a history of cervical cancer, the association between HR-HPV infection and ASCVD mortality remained statistically significant. No cardiovascular deaths were observed among the subjects with cervical cancer, limiting further assessment of cervical cancer, HPV infection, and CVD risk. However, it is important to note that the number of subjects with cervical cancer in our study was only 734 patients, potentially limiting its ability to assess the relationship among HPV infection, cervical cancer, and their association with CVD risk. To further investigate the persistence of HPV infection in patients with treated cervical cancer and its potential association with cardiovascular events, future studies with a larger sample size specifically focused on this population and incorporating measures of HPV persistence are warranted.
Human papillomavirus vaccines have been widely introduced since 2007 and have been effective in preventing HPV-related cancers and benign conditions. 49 , 50 In countries with high vaccine uptake, HPV vaccination programmes have also been effective in reducing the risk of HPV 16 and 18 infection (up to an 83% reduction), as well as the risk of anogenital warts (up to a 67% reduction) and cervical intra-epithelial neoplasia 2 (up to a 51% reduction). 50 In a recent analysis from the National Health and Nutrition Examination, it was reported that significant associations between vaginal HPV infection and CVD were not observed among HPV-vaccinated women. 51 Although it remained unclear in the study whether the loss of the pathogenic activities of HPV in women post-vaccination reduced the risk of CVD or whether the vaccine itself had direct cardioprotective effects via some unknown mechanism, the findings, together with ours, potentially suggest that HPV risk reduction through vaccination may have benefits in preventing adverse long-term CVD outcomes. Human papillomavirus vaccination is recommended before sexual debut for both sexes and has been approved for selective therapy in older adults. 49 Successful national HPV vaccination campaigns may reduce not only HPV-related cancers but also CVD and CVD-related mortality. Future longitudinal studies should further evaluate the potential benefits of HPV vaccination or treatment in reducing CVD mortality.
Our study had several limitations. First, we lacked information on the duration of exposure to HR-HPV infection before the baseline visit, which precluded lifetime HPV infection status assessment, including initial infection, regression, and persistence. Second, we did not identify specific HR-HPV genotypes, low-risk HPV infection cases, or cervical pathology data. We also lacked data on the vaccination status and type-specific HPV genotypes of the vaccinated women in this study. In Korea, the quadrivalent and bivalent HPV vaccines have been approved for use in women aged 9–26 since 2007 and 2008, respectively. Human papillomavirus vaccination was initially introduced in South Korea as part of the National Immunization Program in 2016 targeting 12-year-old girls. 52 Considering that our study included female participants with a mean age of 40.2 ± 9.7 years who attended a health check-up programme between 2004 and 2018, it is reasonable to assume that the HPV vaccination rate among individuals in our study might be relatively low. Furthermore, the prevalence of HPV 16 and HPV 18, the most aggressive oncogenic strains covered by the HPV vaccine, may have decreased over time as vaccine uptake increased, whereas the prevalence of other non-vaccine HPV subtypes may not differ or may be slightly lower between vaccinated and non-vaccinated women. 53 , 54 This could result in an underestimation of the association between the most oncogenic HR-HPV types (16 and 18) and CVD mortality. Third, our study population consisted of young and middle-aged Korean women with relatively high socioeconomic statuses and education levels, in whom the HR-HPV prevalence rate was 9.2%, similar to the 8.4% reported based on health check-ups in Korean women 55 but lower than the overall prevalence rate of 14%–19% in US women aged 30 years or older. 56 Thus, it is important to acknowledge that the findings of this study are limited to Korean women, and caution should be exercised when extrapolating these results to other populations. The study focused on HR-HPV testing as part of a health examination exclusively for women, while HPV testing is not routinely performed in men. However, a previous study involving patients with head and neck cancer, predominantly males (74.9%), discovered that HPV-positive status was linked to an increased risk of stroke or transient ischaemic attack. 30 This implies that HPV infection may also be considered a risk factor for CVD in men as well. In recent years, the significance of HPV testing and vaccination in men for the prevention and early detection of HPV-related diseases has been increasingly recognized. 57 Given the high prevalence of HPV infection in both men and women, it is crucial to further investigate whether HPV infection serves as an unconventional risk factor in CVD development and prognosis, considering larger and more diverse populations. Fourth, the relatively small number of CVD deaths in the study sample may have constrained the statistical power to detect significant associations. Furthermore, despite the relative risk for ASCVD mortality being 3.5 times higher in HPV-positive women compared with HPV-negative women, it is crucial to note that the absolute risk for these outcomes is small among these relatively healthy and young individuals, equalling to 7.1 deaths per 100.000 person-years of follow-up. It is also important to clarify that this study did not establish a causal relationship between HR-HPV infection and CVD mortality. Further research is needed to confirm these findings through studies involving different populations with varied demographics, including age, sex, race/ethnicity, and comorbidities.
In this large cohort study of young and middle-aged Korean women, who have low absolute risks of CVD mortality, we identified a positive association between HR-HPV infection and elevated risk of CVD mortality, particularly among individuals with obesity. Our findings suggest that HR-HPV infection, especially when combined with obesity, may be associated with an increased risk of CVD mortality. Considering the absence of specific antiviral drugs targeting HPV and the limited pharmaceutical interventions for inflammation associated with HPV, further research is warranted to explore potential vaccine strategies aimed at reducing HR-HPV infection and the potential use of anti-inflammatory drugs in the context of HPV-associated CVD, with the goal of mitigating CVD mortality and improving patient outcomes.
We express our gratitude to the staff of the Kangbuk Samsung Health Study for their diligent efforts, unwavering commitment, and ongoing support.
Supplementary data are available at European Heart Journal online.
Disclosure of Interest
All authors declare no disclosure of interest for this contribution.
The data will not be made publicly available owing to our institutional review board’s regulations. However, the analytical methods are available from the corresponding author upon reasonable request.
This study was supported by the SKKU Excellence in Research Award Research Fund (Sungkyunkwan University, 2022).
This study was approved by the institutional review board of Kangbuk Samsung Hospital (KBSMC 2022-05-029).
Not applicable.
Roth GA , Forouzanfar MH , Moran AE , Barber R , Nguyen G , Feigin VL , et al . Demographic and epidemiologic drivers of global cardiovascular mortality . N Engl J Med 2015 ; 372 : 1333 – 41 . https://doi.org/10.1056/NEJMoa1406656
Google Scholar
Timmis A, Vardas P, Townsend N, Torbica A, Katus H, De Smedt D, et al . European Society of Cardiology: cardiovascular disease statistics 2021. Eur Heart J 2022; 43 :716–99. https://doi.org/10.1093/eurheartj/ehab892
Benjamin EJ , Blaha MJ , Chiuve SE , Cushman M , Das SR , Deo R , et al. Heart disease and stroke statistics—2017 update: a report from the American Heart Association . Circulation 2017 ; 135 : e146 – 603 . https://doi.org/10.1161/CIR.0000000000000485
Piepoli MF , Hoes AW , Agewall S , Albus C , Brotons C , Catapano AL , et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) . Eur Heart J 2016 ; 37 : 2315 – 81 . https://doi.org/10.1093/eurheartj/ehw106
Arnett DK , Blumenthal RS , Albert MA , Buroker AB , Goldberger ZD , Hahn EJ , et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines . Circulation 2019 ; 140 : e596 – 646 . https://doi.org/10.1161/CIR.0000000000000678
Visseren FLJ , Mach F , Smulders YM , Carballo D , Koskinas KC , Back M , et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice . Eur Heart J 2021 ; 42 : 3227 – 337 . https://doi.org/10.1093/eurheartj/ehab484
Khot UN , Khot MB , Bajzer CT , Sapp SK , Ohman EM , Brener SJ , et al. Prevalence of conventional risk factors in patients with coronary heart disease . JAMA 2003 ; 290 : 898 – 904 . https://doi.org/10.1001/jama.290.7.898
Satterwhite CL , Torrone E , Meites E , Dunne EF , Mahajan R , Ocfemia MC , et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008 . Sex Transm Dis 2013 ; 40 : 187 – 93 . https://doi.org/10.1097/OLQ.0b013e318286bb53
Brito LMO , Brito HO , Correa R , de Oliveira Neto CP , Costa JPL , Monteiro SCM , et al. Human papillomavirus and coronary artery disease in climacteric women: is there an association? ScientificWorldJournal 2019 ; 2019 : 1872536 . https://doi.org/10.1155/2019/1872536
Koshiol J , Lindsay L , Pimenta JM , Poole C , Jenkins D , Smith JS . Persistent human papillomavirus infection and cervical neoplasia: a systematic review and meta-analysis . Am J Epidemiol 2008 ; 168 : 123 – 37 . https://doi.org/10.1093/aje/kwn036
Kuo HK , Fujise K . Human papillomavirus and cardiovascular disease among U.S. women in the National Health and Nutrition Examination Survey, 2003 to 2006 . J Am Coll Cardiol 2011 ; 58 : 2001 – 6 . https://doi.org/10.1016/j.jacc.2011.07.038
Joo EJ , Chang Y , Kwon MJ , Cho A , Cheong HS , Ryu S . High-risk human papillomavirus infection and the risk of cardiovascular disease in Korean women . Circ Res 2019 ; 124 : 747 – 56 . https://doi.org/10.1161/CIRCRESAHA.118.313779
Muhlestein JB . Chronic infection and coronary atherosclerosis. Will the hypothesis ever really pan out? J Am Coll Cardiol 2011 ; 58 : 2007 – 9 . https://doi.org/10.1016/j.jacc.2011.08.015
Chang Y , Ryu S , Choi Y , Zhang Y , Cho J , Kwon MJ , et al. Metabolically healthy obesity and development of chronic kidney disease: a cohort study . Ann Intern Med 2016 ; 164 : 305 – 12 . https://doi.org/10.7326/M15-1323
Haskell WL , Lee IM , Pate RR , Powell KE , Blair SN , Franklin BA , et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association . Med Sci Sports Exerc 2007 ; 39 : 1423 – 34 . https://doi.org/10.1249/mss.0b013e3180616b27
Craig CL , Marshall AL , Sjostrom M , Bauman AE , Booth ML , Ainsworth BE , et al. International physical activity questionnaire: 12-country reliability and validity . Med Sci Sports Exerc 2003 ; 35 : 1381 – 95 . https://doi.org/10.1249/01.MSS.0000078924.61453.FB
Chun MY . Validity and reliability of Korean version of international physical activity questionnaire short form in the elderly . Korean J Fam Med 2012 ; 33 : 144 – 51 . https://doi.org/10.4082/kjfm.2012.33.3.144
World Health Organization Western Pacific Region . The Asia-Pacific Perspective: Redefining Obesity and Its Treatment . Sydney : Health Communications Australia , 2000 .
Google Preview
cobas HPV test . https://www.accessdata.fda.gov/cdrh_docs/pdf10/p100020s017c.pdf (28 February 2023, date last accessed).
D’Agostino RB Sr , Vasan RS , Pencina MJ , Wolf PA , Cobain M , Massaro JM , et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study . Circulation 2008 ; 117 : 743 – 53 . https://doi.org/10.1161/CIRCULATIONAHA.107.699579
Song YM , Sung J . Body mass index and mortality: a twelve-year prospective study in Korea . Epidemiology 2001 ; 12 : 173 – 9 . https://doi.org/10.1097/00001648-200103000-00008
Won TY , Kang BS , Im TH , Choi HJ . The study of accuracy of death statistics . J Korean Soc Emerg Med 2007 ; 18 : 256 – 62 . http://www.jksem.org/journal/view.php?number=924
Kim KS , Hong S , Han K , Park CY . Assessing the validity of the criteria for the extreme risk category of atherosclerotic cardiovascular disease: a nationwide population-based study . J Lipid Atheroscler 2022 ; 11 : 73 – 83 . https://doi.org/10.12997/jla.2022.11.1.73
Lee HH , Cho SMJ , Lee H , Baek J , Bae JH , Chung WJ , et al. Korea heart disease fact sheet 2020: analysis of nationwide data . Korean Circ J 2021 ; 51 : 495 – 503 . https://doi.org/10.4070/kcj.2021.0097
Molokwu JC , Penaranda E , Lopez DS , Dwivedi A , Dodoo C , Shokar N . Association of metabolic syndrome and human papillomavirus infection in men and women residing in the United States . Cancer Epidemiol Biomarkers Prev 2017 ; 26 : 1321 – 7 . https://doi.org/10.1158/1055-9965.EPI-17-0129
Huang X , Zhao Q , Yang P , Li Y , Yuan H , Wu L , et al. Metabolic syndrome and risk of cervical human papillomavirus incident and persistent infection . Medicine (Baltimore) 2016 ; 95 : e2905 . https://doi.org/10.1097/MD.0000000000002905
Young JG , Stensrud MJ , Tchetgen Tchetgen EJ , Hernan MA . A causal framework for classical statistical estimands in failure-time settings with competing events . Stat Med 2020 ; 39 : 1199 – 236 . https://doi.org/10.1002/sim.8471
Austin PC . An introduction to propensity score methods for reducing the effects of confounding in observational studies . Multivariate Behav Res 2011 ; 46 : 399 – 424 . https://doi.org/10.1080/00273171.2011.568786
Rosenbaum PR , Rubin DB . The central role of the propensity score in observational studies for causal effects . Biometrika 1983 ; 70 : 41 – 55 . https://doi.org/10.1093/biomet/70.1.41
Addison D , Seidelmann SB , Janjua SA , Emami H , Staziaki PV , Hallett TR , et al. Human papillomavirus status and the risk of cerebrovascular events following radiation therapy for head and neck cancer . J Am Heart Assoc 2017 ; 6 : e006453 . https://doi.org/10.1161/JAHA.117.006453
Pothineni NVK , Subramany S , Kuriakose K , Shirazi LF , Romeo F , Shah PK , et al. Infections, atherosclerosis, and coronary heart disease . Eur Heart J 2017 ; 38 : 3195 – 201 . https://doi.org/10.1093/eurheartj/ehx362
Tobler DL , Pruzansky AJ , Naderi S , Ambrosy AP , Slade JJ . Long-term cardiovascular effects of COVID-19: emerging data relevant to the cardiovascular clinician . Curr Atheroscler Rep 2022 ; 24 : 563 – 70 . https://doi.org/10.1007/s11883-022-01032-8
Aleksova A , Fluca AL , Gagno G , Pierri A , Padoan L , Derin A , et al. Long-term effect of SARS-CoV-2 infection on cardiovascular outcomes and all-cause mortality . Life Sci 2022 ; 310 : 121018 . https://doi.org/10.1016/j.lfs.2022.121018
Tonhajzerova I , Olexova LB , Jurko A Jr , Spronck B , Jurko T , Sekaninova N , et al. Novel biomarkers of early atherosclerotic changes for personalised prevention of cardiovascular disease in cervical cancer and human papillomavirus infection . Int J Mol Sci 2019 ; 20 : 3720 . https://doi.org/10.3390/ijms20153720
Hemmat N , Ebadi A , Badalzadeh R , Memar MY , Baghi HB . Viral infection and atherosclerosis . Eur J Clin Microbiol Infect Dis 2018 ; 37 : 2225 – 33 . https://doi.org/10.1007/s10096-018-3370-z
Lawson JS , Glenn WK , Tran DD , Ngan CC , Duflou JA , Whitaker NJ . Identification of human papilloma viruses in atheromatous coronary artery disease . Front Cardiovasc Med 2015 ; 2 : 17 . https://doi.org/10.3389/fcvm.2015.00017
Manzo-Merino J , Massimi P , Lizano M , Banks L . The human papillomavirus (HPV) E6 oncoproteins promotes nuclear localization of active caspase 8 . Virology 2014 ; 450–451 : 146 – 52 . https://doi.org/10.1016/j.virol.2013.12.013
Bodaghi S , Wood LV , Roby G , Ryder C , Steinberg SM , Zheng ZM . Could human papillomaviruses be spread through blood? J Clin Microbiol 2005 ; 43 : 5428 – 34 . https://doi.org/10.1128/JCM.43.11.5428-5434.2005
Foresta C , Bertoldo A , Garolla A , Pizzol D , Mason S , Lenzi A , et al. Human papillomavirus proteins are found in peripheral blood and semen Cd20+ and Cd56+ cells during HPV-16 semen infection . BMC Infect Dis 2013 ; 13 : 593 . https://doi.org/10.1186/1471-2334-13-593
Elliott P , Chambers JC , Zhang W , Clarke R , Hopewell JC , Peden JF , et al. Genetic loci associated with C-reactive protein levels and risk of coronary heart disease . JAMA 2009 ; 302 : 37 – 48 . https://doi.org/10.1001/jama.2009.954
Ridker PM , Bhatt DL , Pradhan AD , Glynn RJ , MacFadyen JG , Nissen SE , et al. Inflammation and cholesterol as predictors of cardiovascular events among patients receiving statin therapy: a collaborative analysis of three randomised trials . Lancet 2023 ; 401 : 1293 – 301 . https://doi.org/10.1016/S0140-6736(23)00215-5
Ridker PM . From C-reactive protein to interleukin-6 to interleukin-1: moving upstream to identify novel targets for atheroprotection . Circ Res 2016 ; 118 : 145 – 56 . https://doi.org/10.1161/CIRCRESAHA.115.306656
Ridker PM , Everett BM , Thuren T , MacFadyen JG , Chang WH , Ballantyne C , et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease . N Engl J Med 2017 ; 377 : 1119 – 31 . https://doi.org/10.1056/NEJMoa1707914
Nidorf SM , Fiolet ATL , Mosterd A , Eikelboom JW , Schut A , Opstal TSJ , et al. Colchicine in patients with chronic coronary disease . N Engl J Med 2020 ; 383 : 1838 – 47 . https://doi.org/10.1056/NEJMoa2021372
Henning RJ . Obesity and obesity-induced inflammatory disease contribute to atherosclerosis: a review of the pathophysiology and treatment of obesity . Am J Cardiovasc Dis 2021 ; 11 : 504 – 29 . https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8449192/
Scott M , Nakagawa M , Moscicki AB . Cell-mediated immune response to human papillomavirus infection . Clin Diagn Lab Immunol 2001 ; 8 : 209 – 20 . https://doi.org/10.1128/CDLI.8.2.209-220.2001
Ridker PM , Buring JE , Rifai N , Cook NR . Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score . JAMA 2007 ; 297 : 611 – 9 . https://doi.org/10.1001/jama.297.6.611
Khafagy R , Dash S . Obesity and cardiovascular disease: the emerging role of inflammation . Front Cardiovasc Med 2021 ; 8 : 768119 . https://doi.org/10.3389/fcvm.2021.768119
Dilley S , Miller KM , Huh WK . Human papillomavirus vaccination: ongoing challenges and future directions . Gynecol Oncol 2020 ; 156 : 498 – 502 . https://doi.org/10.1016/j.ygyno.2019.10.018
Drolet M , Benard E , Perez N , Brisson M ; HPV Vaccination Impact Study Group . Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: updated systematic review and meta-analysis . Lancet 2019 ; 394 : 497 – 509 . https://doi.org/10.1016/S0140-6736(19)30298-3
Liang X , Chou OHI , Cheung BMY . The effects of human papillomavirus infection and vaccination on cardiovascular diseases, NHANES 2003–2016 . Am J Med 2023 ; 136 : 294 – 301.e2 . https://doi.org/10.1016/j.amjmed.2022.09.021
Seong J , Ryou S . Overview of the efficacy of human papillomavirus virus vaccines . J Bacteriol Virol 2020 ; 50 : 158 – 67 . https://doi.org/10.4167/jbv.2020.50.3.158
Malagon T , Drolet M , Boily MC , Franco EL , Jit M , Brisson J , et al. Cross-protective efficacy of two human papillomavirus vaccines: a systematic review and meta-analysis . Lancet Infect Dis 2012 ; 12 : 781 – 9 . https://doi.org/10.1016/S1473-3099(12)70187-1
Carozzi F , Puliti D , Ocello C , Anastasio PS , Moliterni EA , Perinetti E , et al. Monitoring vaccine and non-vaccine HPV type prevalence in the post-vaccination era in women living in the Basilicata region, Italy . BMC Infect Dis 2018 ; 18 : 38 . https://doi.org/10.1186/s12879-018-2945-8
Kim MJ , Kim JJ , Kim S . Type-specific prevalence of high-risk human papillomavirus by cervical cytology and age: data from the health check-ups of 7,014 Korean women . Obstet Gynecol Sci 2013 ; 56 : 110 – 20 . https://doi.org/10.5468/OGS.2013.56.2.110
Lewis RM , Markowitz LE , Gargano JW , Steinau M , Unger ER . Prevalence of genital human papillomavirus among sexually experienced males and females aged 14–59 years, United States, 2013–2014 . J Infect Dis 2018 ; 217 : 869 – 77 . https://doi.org/10.1093/infdis/jix655
Plummer M , de Martel C , Vignat J , Ferlay J , Bray F , Franceschi S . Global burden of cancers attributable to infections in 2012: a synthetic analysis . Lancet Glob Health 2016 ; 4 : e609 – 16 . https://doi.org/10.1016/S2214-109X(16)30143-7
Author notes
- atherosclerosis
- cardiovascular diseases
- heart disease risk factors
- human papillomavirus
Email alerts
Companion article.
- Human papilloma virus and atherosclerotic cardiovascular disease
Related articles in PubMed
Citing articles via, looking for your next opportunity, affiliations.
- Online ISSN 1522-9645
- Print ISSN 0195-668X
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Study Design 101: Cohort Study
- Case Report
- Case Control Study
- Cohort Study
- Randomized Controlled Trial
- Practice Guideline
- Systematic Review
- Meta-Analysis
- Helpful Formulas
- Finding Specific Study Types
A study design where one or more samples (called cohorts) are followed prospectively and subsequent status evaluations with respect to a disease or outcome are conducted to determine which initial participants exposure characteristics (risk factors) are associated with it. As the study is conducted, outcome from participants in each cohort is measured and relationships with specific characteristics determined
- Subjects in cohorts can be matched, which limits the influence of confounding variables
- Standardization of criteria/outcome is possible
- Easier and cheaper than a randomized controlled trial (RCT)
Disadvantages
- Cohorts can be difficult to identify due to confounding variables
- No randomization, which means that imbalances in patient characteristics could exist
- Blinding/masking is difficult
- Outcome of interest could take time to occur
Design pitfalls to look out for
The cohorts need to be chosen from separate, but similar, populations.
How many differences are there between the control cohort and the experiment cohort? Will those differences cloud the study outcomes?
Fictitious Example
A cohort study was designed to assess the impact of sun exposure on skin damage in beach volleyball players. During a weekend tournament, players from one team wore waterproof, SPF 35 sunscreen, while players from the other team did not wear any sunscreen. At the end of the volleyball tournament players' skin from both teams was analyzed for texture, sun damage, and burns. Comparisons of skin damage were then made based on the use of sunscreen. The analysis showed a significant difference between the cohorts in terms of the skin damage.
Real-life Examples
Hoepner, L., Whyatt, R., Widen, E., Hassoun, A., Oberfield, S., Mueller, N., ... Rundle, A. (2016). Bisphenol A and Adiposity in an Inner-City Birth Cohort. Environmental Health Perspectives, 124 (10), 1644-1650. https://doi.org/10.1289/EHP205
This longitudinal cohort study looked at whether exposure to bisphenol A (BPA) early in life affects obesity levels in children later in life. Positive associations were found between prenatal BPA concentrations in urine and increased fat mass index, percent body fat, and waist circumference at age seven.
Lao, X., Liu, X., Deng, H., Chan, T., Ho, K., Wang, F., ... Yeoh, E. (2018). Sleep Quality, Sleep Duration, and the Risk of Coronary Heart Disease: A Prospective Cohort Study With 60,586 Adults. Journal Of Clinical Sleep Medicine, 14 (1), 109-117. https://doi.org/10.5664/jcsm.6894
This prospective cohort study explored "the joint effects of sleep quality and sleep duration on the development of coronary heart disease." The study included 60,586 participants and an association was shown between increased risk of coronary heart disease and individuals who experienced short sleep duration and poor sleep quality. Long sleep duration did not demonstrate a significant association.
Related Formulas
- Relative Risk
Related Terms
A group that shares the same characteristics among its members (population).
Confounding Variables
Variables that cause/prevent an outcome from occurring outside of or along with the variable being studied. These variables render it difficult or impossible to distinguish the relationship between the variable and outcome being studied).
Population Bias/Volunteer Bias
A sample may be skewed by those who are selected or self-selected into a study. If only certain portions of a population are considered in the selection process, the results of a study may have poor validity.
Prospective Study
A study that moves forward in time, or that the outcomes are being observed as they occur, as opposed to a retrospective study, which looks back on outcomes that have already taken place.
Now test yourself!
1. In a cohort study, an exposure is assessed and then participants are followed prospectively to observe whether they develop the outcome.
a) True b) False
2. Cohort Studies generally look at which of the following?
a) Determining the sensitivity and specificity of diagnostic methods b) Identifying patient characteristics or risk factors associated with a disease or outcome c) Variations among the clinical manifestations of patients with a disease d) The impact of blinding or masking a study population
Evidence Pyramid - Navigation
- Meta- Analysis
- Case Reports
- << Previous: Case Control Study
- Next: Randomized Controlled Trial >>

- Last Updated: Sep 25, 2023 10:59 AM
- URL: https://guides.himmelfarb.gwu.edu/studydesign101

- Himmelfarb Intranet
- Privacy Notice
- Terms of Use
- GW is committed to digital accessibility. If you experience a barrier that affects your ability to access content on this page, let us know via the Accessibility Feedback Form .
- Himmelfarb Health Sciences Library
- 2300 Eye St., NW, Washington, DC 20037
- Phone: (202) 994-2850
- [email protected]
- https://himmelfarb.gwu.edu


Metabolic Disease and The Risk of Post-COVID Conditions: A Retrospective Cohort Study
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Wubin Xie
- ORCID record for Heather E. Hsu
- ORCID record for Paul R. Shafer
- ORCID record for Meghan I. Podolsky
- ORCID record for Andrew C. Stokes
- For correspondence: [email protected]
- Info/History
- Preview PDF
Objective To examine the influence of having a baseline metabolic disorder (diabetes, hypertension, and/or obesity) on the risk of developing new clinical sequelae potentially related to SARS-CoV-2 in a large sample of commercially insured adults in the US.
Design, setting, and participants Deidentified data were collected from the IBM/Watson MarketScan Commercial Claims and Encounters (CCAE) Databases and Medicare Supplemental and Coordination of Benefits (MDCR) Databases from 2019 to 2021. A total of 839,344 adults aged 18 and above with continuous enrollment in the health plan were included in the analyses. Participants were grouped into four categories based on their COVID-19 diagnosis and whether they had at least one of the three common metabolic disorders at baseline (diabetes, obesity, or hypertension).
Measures and methods ICD-10-CM codes were used to determine new symptoms and conditions after the acute phase of SARS-CoV-2 infection, defined as ending 21 days after initial diagnosis date, or index period for those who did not have a COVID-19 diagnosis. Propensity score matching (PSM) was used to create comparable reference groups. Cox proportional hazard models were conducted to estimate hazard ratios and 95% confidence intervals.
Results Among the 772,377 individuals included in the analyses, 36,742 (4.8%) without and 20,912 (2.7%) with a baseline metabolic disorder were diagnosed with COVID-19. On average, COVID-19 patients with baseline metabolic disorders had more 2.4 more baseline comorbidities compared to those without baseline metabolic disorders. Compared to adults with no baseline metabolic condition, the risks of developing new clinical sequelae were highest among COVID-19 patients with a baseline metabolic condition (HRs ranging from 1.51 to 3.33), followed by those who had a baseline metabolic condition but with no COVID-19 infection (HRs ranging from 1.33 to 2.35), and those who had COVID-19 but no baseline metabolic condition (HRs ranging from 1.34 to 2.85).
Conclusions In a large national cohort of commercially insured adults, COVID-19 patients with a baseline metabolic condition had the highest risk of developing new clinical sequelae post-acute infection phase, followed by those who had baseline metabolic condition but no COVID-19 infection and those who had COVID-19 but no baseline metabolic disorder.
Competing Interest Statement
Dr. Stokes reported receiving grants from Johnson & Johnson, Inc. outside of the submitted work. No other disclosures were reported.
Funding Statement
We gratefully acknowledge receiving financial support through grants from the Robert Wood Johnson Foundation (77521); the National Institute on Aging (R01-AG060115-04S1); the W.K. Kellogg Foundation (P-6007864-2022); the National Science Foundation (CCF-2200052); and Swiss Re, Inc. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
The details of the IRB/oversight body that provided approval or exemption for the research described are given below:
Ethical approval was granted by the Boston University/Boston Medical Center Institutional Review Board.
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
All data produced in the present study are available upon reasonable request to the authors.
View the discussion thread.
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
Subject Area
- Epidemiology
- Addiction Medicine (313)
- Allergy and Immunology (616)
- Anesthesia (158)
- Cardiovascular Medicine (2257)
- Dentistry and Oral Medicine (278)
- Dermatology (201)
- Emergency Medicine (368)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (794)
- Epidemiology (11550)
- Forensic Medicine (10)
- Gastroenterology (676)
- Genetic and Genomic Medicine (3542)
- Geriatric Medicine (336)
- Health Economics (612)
- Health Informatics (2287)
- Health Policy (910)
- Health Systems and Quality Improvement (858)
- Hematology (333)
- HIV/AIDS (742)
- Infectious Diseases (except HIV/AIDS) (13128)
- Intensive Care and Critical Care Medicine (751)
- Medical Education (357)
- Medical Ethics (100)
- Nephrology (386)
- Neurology (3327)
- Nursing (190)
- Nutrition (504)
- Obstetrics and Gynecology (648)
- Occupational and Environmental Health (643)
- Oncology (1748)
- Ophthalmology (523)
- Orthopedics (208)
- Otolaryngology (283)
- Pain Medicine (222)
- Palliative Medicine (66)
- Pathology (436)
- Pediatrics (998)
- Pharmacology and Therapeutics (418)
- Primary Care Research (399)
- Psychiatry and Clinical Psychology (3043)
- Public and Global Health (5975)
- Radiology and Imaging (1216)
- Rehabilitation Medicine and Physical Therapy (711)
- Respiratory Medicine (807)
- Rheumatology (367)
- Sexual and Reproductive Health (345)
- Sports Medicine (311)
- Surgery (383)
- Toxicology (50)
- Transplantation (170)
- Urology (142)
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Delirium and incident...
Delirium and incident dementia in hospital patients in New South Wales, Australia: retrospective cohort study
- Related content
- Peer review
- Emily H Gordon , senior lecturer 1 2 ,
- David D Ward , research fellow 1 2 ,
- Hao Xiong , research fellow 3 ,
- Shlomo Berkovsky , professor of medical artificial intelligence 3 ,
- Ruth E Hubbard , professor of geriatric medicine 1 2
- 1 Centre for Health Services Research, The University of Queensland, Princess Alexandra Hospital, Woolloongabba, QLD, Australia
- 2 Australian Frailty Network, The University of Queensland, Princess Alexandra Hospital, Woolloongabba, QLD, Australia
- 3 Centre for Health Informatics, Macquarie University, North Ryde, NSW, Australia
- Correspondence to: EH Gordon e.gordon{at}uq.edu.au ( @DrEHGordon on X)
- Accepted 22 February 2024
Objectives To determine the strength and nature of the association between delirium and incident dementia in a population of older adult patients without dementia at baseline.
Design Retrospective cohort study using large scale hospital administrative data.
Setting Public and private hospitals in New South Wales, Australia between July 2001 and March 2020.
Participants Data were extracted for 650 590 hospital patients aged ≥65 years. Diagnoses of dementia and delirium were identified from ICD-10 (international classification of diseases, 10th revision) codes. Patients with dementia at baseline were excluded. Delirium-no delirium pairs were identified by matching personal and clinical characteristics, and were followed for more than five years.
Main outcome measures Cox proportional hazards models and Fine-Gray hazard models were used to estimate the associations of delirium with death and incident dementia, respectively. Delirium-outcome dose-response associations were quantified, all analyses were performed in men and women separately, and sensitivity analyses were conducted.
Results The study included 55 211 matched pairs (48% men, mean age 83.4 years, standard deviation 6.5 years). Collectively, 58% (n=63 929) of patients died and 17% (n=19 117) had a newly reported dementia diagnosis during 5.25 years of follow-up. Patients with delirium had 39% higher risk of death (hazard ratio 1.39, 95% confidence interval 1.37 to 1.41) and three times higher risk of incident dementia (subdistribution hazard ratio 3.00, 95% confidence interval 2.91 to 3.10) than patients without delirium. The association with dementia was stronger in men (P=0.004). Each additional episode of delirium was associated with a 20% increased risk of dementia (subdistribution hazard ratio 1.20, 95% confidence interval 1.18 to 1.23).
Conclusions The study findings suggest delirium was a strong risk factor for death and incident dementia among older adult patients. The data support a causal interpretation of the association between delirium and dementia. The clinical implications of delirium as a potentially modifiable risk factor for dementia are substantial.
Introduction
Delirium is characterised by inattention and disturbance of awareness that represents a change from baseline cognitive function, and is precipitated by acute events such as illness and surgery. Delirium is a prevalent condition in hospital, with an estimated occurrence of 23% in patients with acute medical conditions 1 and up to 45% in patients aged 90 years and older. 2 Delirium is associated with adverse outcomes, including death in hospital or in the short to medium term post discharge, prolonged hospital stay, and new admission to a residential institution. 3 In 2020, Goldberg and colleagues 4 found that delirium was also associated with long term cognitive decline (ie, decrease in objective cognitive scores or new clinical diagnosis of dementia) in their meta-analysis of 24 studies including 10 459 patients. This association persisted in their subgroup analysis of 19 studies examining patients without cognitive impairment at baseline. An association between delirium and incident dementia in patients without dementia at baseline has been reported in a subsequent systematic review and meta-analysis. 5 However, included studies were relatively modest in size (between 78 and 329 patients) and variably adjusted for important confounders. Furthermore, studies did not account for the competing risk of death, which is particularly high in this vulnerable population and might contribute to biased risk estimates of incident dementia in relation to delirium. 6
Mechanisms linking delirium with incident dementia are under debate. Delirium might be an epiphenomenon, it might uncover unrecognised (preexisting or preclinical) dementia, or it might cause dementia by accelerating underlying neuropathological processes or de novo mechanisms. 7 Observational studies are limited in their capacity to validate causality; however, the association between delirium and dementia is not amenable to randomisation. Dose-response analysis might contribute valuable information to the debate about causality. In 2021, the Delirium and Cognitive Impact in Dementia study showed that more than one episode of delirium was associated with a greater risk of incident dementia compared with a single episode in a sample of 173 older hospital patients. 8
As the global burden of dementia increases, 9 it is important to confirm the extent to which delirium is a potentially modifiable risk factor. We aimed to use large scale hospital administrative data to clarify the strength and nature of the association between delirium and incident dementia in a population of older adult patients without dementia at baseline.
We undertook a retrospective cohort study using a longitudinal statewide dataset linked by the New South Wales (NSW) Centre for Health Record Linkage. 10
Data sources
The NSW Admitted Patient Data Collection records all inpatient episodes of care (defined by separations—discharges, transfers, and deaths) from all NSW public and private hospitals. Data include personal (eg, date of birth, gender, residential address, country of birth), administrative (eg, admission and separation dates), and clinical (eg, diagnoses and procedures) information. For each episode, one primary diagnosis and up to 50 secondary diagnoses are coded using the international classification of diseases, 10th revision (ICD-10). 11 Admitted Patient Data Collection records linked to the NSW Registry of Births, Deaths and Marriages data were available from July 2001 onwards. Linked data up to and including 31 March 2020 were available to the research team (>12 million episodes).
Study design and sample
We defined a six year index period (1 January 2009 to 31 December 2014) so that sufficient data were available to determine that patients did not have a previous dementia diagnosis, to calculate a hospital frailty risk score (HFRS) for every patient, and to provide adequate follow-up for all patients ( fig 1 ). A HFRS was calculated for each patient using ICD-10 codes recorded for episodes in the preceding two year period (see supplementary material for further information about HFRS). 12 The follow-up period for all patients was 63 months (5.25 years), which was the time between the end of the index period and the end of the dataset. We identified 650 590 patients aged 65 years and older who had one or more episodes of care (total episodes 4 779 584) from NSW hospitals during the index period.

Study design. Patients in the delirium group (index episode=orange circle) and no delirium group (index episode=green circle) were matched 1:1 according to age, gender, hospital frailty risk score, primary diagnosis, hospital length of stay and intensive care unit length of stay of index episode. Arrows to left of circles represent exclusion of previous dementia diagnosis and two year lookback for hospital frailty risk score calculation. Arrows to right of circles represent 63 month follow-up period
- Download figure
- Open in new tab
- Download powerpoint
Dementia and delirium diagnoses were extracted from primary and secondary diagnoses data using ICD-10 codes (see supplementary material). In Australian hospitals, a patient presenting to hospital with cognitive impairment, or with an acute change in behaviour or cognitive status in hospital, is assessed for delirium by an appropriately trained clinician, ideally using a validated tool (commonly the 4AT, a diagnostic tool designed specifically for routine clinical use). 13 Patients with a dementia diagnosis or episode of delirium recorded before the index period were excluded, as were patients aged >110 years and those with data inconsistencies (eg, implausible dates).
Patients were then categorised into delirium and no delirium groups. For patients in the delirium group, the first episode recording a delirium diagnosis was identified as the index episode. Patients with a dementia diagnosis recorded at or before the index episode were then excluded.
Patients in the delirium group were matched 1:1 to patients in the no delirium group according to patient and episode characteristics with potential to confound the association between delirium and subsequent risk of dementia. The confounders were patient age (in years; continuous variable), gender (man or woman), HFRS (≥0; continuous variable), and the primary diagnosis (ICD-10 code up to seven characters), episode length of stay (in days; discrete variable), and intensive care unit length of stay (in days; continuous variable) of the index episode. In the event that delirium was the primary diagnosis of an index episode, the primary diagnosis variable was not used for matching. Patients in the no delirium group with a dementia diagnosis recorded at or before the index episode were excluded and an alternative match was identified. Matching was without replacement; that is, each patient without delirium was matched to (at most) one patient with delirium.
The primary outcomes were incident dementia and death. The start date of the episode with a newly recorded dementia diagnosis was identified as the event time for incident dementia (see supplementary material for incident dementia ICD-10 codes). Mortality data, including date of death (the other event time), were available in the linked data.
Statistical analysis
Descriptive summary statistics were calculated at baseline separately for patients in the delirium and no delirium groups, and for patients who made up the total eligible sample for comparison. In all statistical models, linear associations were assumed between continuous covariates (age, HFRS, episode length of stay, and intensive care unit length of stay) and study outcomes (death and incident dementia).
When death was the outcome, patient follow-up was from the index episode until death. When dementia was the outcome, patient follow-up was from the index episode until the onset of dementia or death (whichever came first). In both instances, patients who remained event free were censored at 63 months.
We first assessed differences between the delirium group and the no delirium group in the incidence of an outcome (death or dementia). Next, we applied a landmarking approach to determine the presence of a dose-response association between the number of episodes of delirium and the outcome. 14 The number of delirium episodes occurring within the first 12 months of follow-up was associated with event incidence rates subsequent to that 12 month period. Delirium episodes were first used as categorical variables in the full sample (categorised as 0 episodes, 1 episode, 2 episodes, and ≥3 episodes) and then as continuous variables in the delirium cohort only. Dose-response models included covariates of age and gender, and the number of hospital episodes recorded within the landmark period (categorised as 1-5, 6-10, 11-20, and >20 episodes), and only patients who remained event free within the landmark period were included.
A different statistical modelling technique was used for each outcome. For death, we used Cox proportional hazards models and expressed the strength of associations as hazard ratios. For dementia, we used Fine-Gray subdistribution hazard models that accounted for the competing risk of death and expressed associations as subdistribution hazard ratios. 15 Given the strong association between delirium and risk of death, the competing risks analysis approach improves the accuracy of association estimates.
We conducted several sensitivity analyses to assess the robustness of associations. For both outcomes, we excluded patient pairs with distance values within the top 10% (least matched patients) and simultaneously included as covariates all characteristics used in the matching process (ie, age, gender, HFRS, primary diagnosis ICD-10 category, episode length of stay, and intensive care unit length of stay) to account for any residual differences in characteristics between groups. Additionally, when dementia was the outcome, we repeated analyses after excluding patients who died or had a diagnosis of dementia within 24 months of their index episode to reduce the impact of undetected dementia on the results. To assess the robustness of the dose-response associations, we repeated the analyses while extending the landmark period from 12 to 24 months. Finally, all analyses were conducted in the total matched sample and for men and women separately.
All estimates of associations were accompanied by 95% confidence intervals to represent the uncertainty. Statistical analyses were conducted using R version 4.2.3.
Supplementary analyses
We opted for a matched cohort design to reduce the confounding effects of key clinical variables and to permit sensitivity analyses that adjusted for residual confounding. Matching reduced the computational burden in this large study and allowed more reliable comparison without sacrificing statistical precision. The supplementary material presents an alternative approach using the total eligible sample.
Patient and public involvement
This study was inspired by EHG and REH’s clinical experience as geriatricians. There was no direct patient and public involvement in the study because the analysis of this restricted access administrative dataset was retrospective. However, a consumer representative with lived experienced of delirium who is actively involved in delirium prevention and education programmes in Australia reviewed the manuscript, confirmed the importance and potential impact of the study and its results, and contributed to the dissemination strategy.
Sample characteristics
Of the 650 590 patients, 626 467 were eligible for inclusion in the analytical sample. The supplementary material presents the 80 most frequent ICD-10 codes recorded as primary diagnoses for these patients. The matched study sample included 110 422 patients across the two groups ( fig 1 ). Table 1 presents personal and clinical characteristics for the total eligible sample (n=626 467) and the matched sample (delirium group n=55 211; no delirium group n=55 211). At baseline, matched patients ranged in age from 65 to 109 years and most were older (mean age 83.4 years, standard deviation 6.5 years). Women and men were almost equally represented (52% women, 48% men). Despite matching, the length of stay (for the index episode and in the intensive care unit) was slightly longer for the delirium group than the no delirium group. In the delirium group, 6351 patients had a primary diagnosis of delirium. The supplementary material includes additional results about matching .
Baseline characteristics of study sample
- View inline
Delirium and risk of death
The rate of death was 1.4 times higher in the delirium group than in the no delirium group ( table 2 ), which equates to a 39% increased risk of death ( fig 2 , upper panel). The risk was similar for men and women (interaction P=0.62). After excluding the least matched patients and adjusting for all covariates used in the matching process, the association strengthened marginally (hazard ratio 1.41, 95% confidence interval 1.39 to 1.44). When all eligible patients from the total sample were analysed and characteristics used in the matching were included in statistical models as covariates, findings were similar although associations strengthened (see supplementary material).
Delirium and occurrence of death and dementia

Association of delirium with death by baseline group (upper panel) and episodes of delirium recorded within first 12 months of follow-up (landmark period; lower panel). Associations presented in forest plot in lower panel were adjusted for age and gender at baseline, and number of hospital episodes recorded within landmark period. Total sample data are hazard ratio 1.36 (95% confidence interval 1.33 to 1.39) for one delirium episode, 1.67 (1.61 to 1.72) for two episodes, and 1.82 (1.74 to 1.90) for three or more episodes. Corresponding data for men only are 1.36 (1.32 to 1.40), 1.71 (1.63 to 1.79), and 1.83 (1.72 to 1.95), respectively. Corresponding data for women only are 1.36 (1.32 to 1.40), 1.63 (1.56 to 1.70), and 1.81 (1.70 to 1.91), respectively
When episodes of delirium were counted within the 12 month landmark period and categorised (0 episodes, 1 episode, 2 episodes, ≥3 episodes), more episodes were monotonically associated with a higher risk of death ( fig 2 , lower panel). These associations strengthened marginally when episodes of delirium were counted within a 24 month landmark period (see supplementary material). Among patients who experienced at least one episode of delirium within the landmark period, each additional episode of delirium was associated with a 10% increased risk of death (hazard ratio 1.10, 95% confidence interval 1.09 to 1.12).
Delirium and risk of dementia
The rate of incident dementia in the delirium group was 3.4 times higher than the no delirium group ( table 2 ). After accounting for the competing risk of death, the risk of incident dementia remained three times higher among the delirium group ( fig 3 , upper panel). This association was stronger for men than women (subdistribution hazard ratio 3.17 and 2.88, respectively, P=0.004). The association also strengthened marginally after excluding the least matched patients and adjusting for all covariates used in the matching process (3.09, 2.98 to 3.19) and was similar after excluding patients who died or developed dementia within 24 months of the index episode (2.98, 2.86 to 3.11). When all eligible patients from the total sample were analysed and characteristics used in the matching were included as covariates, results were comparable although most associations were weaker (see supplementary material).

Association of delirium with incident dementia by baseline group (upper panel) and episodes of delirium recorded within first 12 months of follow-up (landmark period; lower panel). Associations presented in forest plot in lower panel were adjusted for age and gender at baseline, and number of hospital episodes recorded within landmark period. Total sample data are subdistribution hazard ratio 2.81 (95% confidence interval 2.70 to 2.92) for one delirium episode, 3.70 (3.50 to 3.91) for two episodes, and 4.91 (4.57 to 5.28) for three or more episodes. Corresponding data for men only are 3.06 (2.88 to 3.25), 4.15 (3.81 to 4.52), and 5.72 (5.12 to 6.38), respectively. Corresponding data for women only are 2.64 (2.51 to 2.78), 3.42 (3.18 to 3.67), and 4.39 (3.99 to 4.83), respectively
In the 12 month landmark analysis, more delirium episodes were monotonically associated with a higher risk of incident dementia ( fig 3 , lower panel). These associations weakened marginally when episodes of delirium were counted within a 24 month landmark period (see supplementary material). Among patients who experienced at least one episode of delirium within the landmark period, each additional episode of delirium was associated with a 20% increased risk of dementia (subdistribution hazard ratio 1.20, 95% confidence interval 1.18 to 1.23).
Principal findings
We found delirium to be a strong risk factor for death and incident dementia in this cohort of older Australian hospital patients. We observed that among patients without dementia at baseline with at least one episode of delirium, the risk of a new dementia diagnosis was about three times higher than for patients without delirium over five years of follow-up. Among patients with at least one episode of delirium, each additional episode of delirium increased that risk by 20%. These associations were observed in a large scale dataset and were robust to several tests of bias and confounding, supporting the hypothesis that delirium has a strong independent effect on dementia risk in this clinical population.
Comparison with other studies
In our study, the rate of death was higher than the rate of incident dementia. Death was an important competing risk—it was an outcome of equal or higher clinical importance than the primary outcome that changed the probability of the primary outcome. 6 Leighton and colleagues 16 recently estimated the cumulative incidence of new dementia (accounting for competing risk of death without a dementia diagnosis) to be 31% by five years in their sample of 12 949 patients with delirium aged 65 years and older. This proportion is higher than our result (25%), possibly owing to their inclusion of dementia diagnosis at death (18% of patients) in their cumulative incidence calculations.
Recently, two studies conducted competing risk analyses in smaller cohorts of older patients and reported different risk estimates for incident dementia in relation to delirium in patients without dementia at baseline (subdistribution hazard ratio 1.94 and 8.70, respectively). 17 18 The studies had many methodological differences, most notably in study design (retrospective v prospective), size (n=390 v 1100), duration of follow-up (median 24 months v mean 82 months), and covariates. While Garcez and colleagues 17 accounted primarily for the confounding effects of frailty in their older inpatient population, Rolandi and colleagues 18 examined the independent effects of non-modifiable and potentially modifiable risk factors in their population based study. Neither study adjusted for clinical variables relating to illness severity or examined the impact of more than one episode of delirium.
Richardson and colleagues 8 recently estimated that older patients with delirium had almost nine times the risk of incident dementia (odds ratio 8.8) compared with patients without delirium and that the risk increased with subsequent episodes of delirium (odds ratio 8.6 and 13.0 for one episode and more than one episode, respectively). These findings are consistent with our study, even though the estimates are higher. This difference might be attributable to the smaller study size (n=135), shorter duration of follow-up (12 months), and an unaccounted for competing risk of death (n=38, 18%). 8 Our study and that of Richardson and colleagues 8 share some strengths, including adjusting for baseline characteristics such as age, gender, frailty, and measures of illness severity (APACHE II (acute physiology and chronic health evaluation II) v primary diagnosis, episode length of stay, and intensive care unit length of stay). The studies differed in their approach to diagnosis of delirium and dementia. However, the meta-regression of 24 studies by Goldberg and colleagues 4 suggested that the approach to diagnosis might not have much impact on variance in results.
Mechanistic understanding and implications for future research
We found that there was a persistent association between delirium and incident dementia years after the episode of delirium (and resolution of the precipitating stressors), which suggests that delirium is not an epiphenomenon or merely a marker of unrecognised dementia or a vulnerable brain. Furthermore, the dose-response association between delirium and incident dementia suggests a causal link between the two conditions. Several hypotheses have been proposed explaining how delirium might cause dementia. 7 For example, the sequelae of delirium (drowsiness, agitation, circadian disturbance, and unsafe behaviours) might precipitate a cascade of geriatric syndromes (mobility impairment and falls, pressure ulcers, malnutrition and dehydration), medical complications (electrolyte disturbance, aspiration and respiratory failure, infection and venous thromboembolism) and chemical and physical restraint, all of which might exert a toxic effect on the brain. Alternatively, or additionally, delirium might contribute to neuronal injury and neurodegeneration through a range of disrupted biological mechanisms (see Fong and Inouye 7 for a comprehensive review). Associations between systemic inflammatory markers, delirium, and dementia are variable in preclinical and clinical models and appear to be influenced by the presence or absence of dementia pathology. Similarly, markers of neuroinflammation have been associated with both syndromes. Alzheimer’s disease biomarkers (eg, Aβ, tau) have been associated with risk of incident delirium and the association between the APOE genotype and delirium suggests a mediating role of genetic profiles related to systemic inflammation. Neuroimaging studies have identified structural and functional predictors of delirium, such as changes in network connectivity in the posterior cingulate cortex. A direct pathway between delirium and neuronal injury (not mediated by systemic inflammation, for example) has not been established but is theoretically possible. Ultimately, a better understanding of the delirium-dementia pathophysiological pathways might guide the development of new treatments with potential to prevent or reduce neurodegeneration.
In our study, we observed delirium to impart a larger increase in dementia risk in men than women. Despite this difference, in the delirium and no delirium groups, women experienced dementia at a slightly higher rate than men. The literature on sex differences in dementia is rapidly evolving; there is emerging evidence for differences in dementia risk 19 and mediating factors 20 for men and women. However, one meta-analysis (201 studies, n=998 187) did not find major differences in dementia incidence in men and women except in the oldest old (>90 years). 21 For delirium, it remains unclear whether gender is a predisposing risk factor, with both genders being associated with increased risk in various inpatient populations. 22
We might hypothesise that the increased risk of incident dementia with delirium in men indicates lower reserve (ie, higher burden of neuropathology). Although this might be unlikely given the higher global prevalence of dementia in older women than men, 21 it is increasingly understood that the association between neuropathological burden and clinical dementia is not linear 23 and that there are likely to be important sex differences in patterns of neuropathology in people with and without dementia. 24 Another hypothesis is that delirium in men might be more severe. However, a recent prospective study of older adults with delirium did not identify any gender differences in clinical phenotypes, course, or response to treatment. 25 There might also be fundamental sex differences in the biological mechanisms of delirium that lead to de novo neuronal injury and accelerated neurodegeneration. Future studies might explore these hypotheses to try and identify sex specific targets for intervention.
Pooled data from 14 studies including 2640 patients aged 18 years and older showed that multicomponent non-pharmacological interventions were associated with a reduced incidence of delirium (risk ratio 0.57), a reduced duration of a delirium episode, and reduced hospital length of stay compared with usual care. 26 In older adults specifically, a systematic review and meta-analysis of data from studies of a widely disseminated delirium prevention programme (the Hospital Elder Life Program) showed that the intervention was associated with a reduced incidence of delirium (odds ratio 0.47) and falls (odds ratio 0.58), a reduced hospital length of stay and preserved functional status, and reduced healthcare costs. 27 Currently, data are lacking about the impact of these interventions on the risk of incident dementia. 26 Because the burden of dementia is set to dramatically rise in coming decades and multicomponent non-pharmacological delirium prevention interventions are effective and readily implemented, quantifying the benefit of interventions on dementia incidence rates should be addressed in future clinical trials as a matter of priority. 28
Strengths and limitations of this study
In this large study of delirium and incident dementia, we minimised bias by adjusting for important personal and clinical baseline variables, having a long period of follow-up, and accounting for the competing risk of death in our analyses. This approach helped to overcome methodological issues prevalent in the existing literature. Therefore, it is likely that our estimate lies closer to the true effect of delirium on incident dementia in patients without dementia at baseline. The size and granularity of the data afforded precision when conducting adjusted dose-response analyses and the results of predetermined sensitivity analyses showed the robustness of the reported results. By stratifying results by gender, we generated insights with important pathophysiological and clinical implications.
The results should be considered within the context of this study’s limitations. Diagnosis of delirium and dementia depended on clinical coding of medical information from inpatient episodes of care recorded in the administrative dataset used. Differential diagnosis of delirium, dementia, and delirium superimposed on dementia is difficult and conditions might go undetected or be misattributed. 7 Under-coding of dementia during hospital admission is a well recognised issue and correlates with lack of documentation of dementia diagnosis in medical notes. 29 Similarly, published data suggest that coding for delirium underestimates true delirium rates. 30 While the use of routinely collected healthcare data in determining the presence of all cause dementia is supported by positive predictive values between 70% and 90%, 31 it is possible that erroneous diagnoses were made (false positives) and other diagnoses were missed (false negatives), which would affect the incident rates reported here. Future studies might combine different administrative data sources (eg, pharmaceutical, primary care, aged care) to improve case detection and reduce the potential for bias.
We matched delirium and no delirium groups 1:1 using important personal and clinical characteristics. However, we were limited to the data available in the administrative dataset and there could be residual confounding effects from unmeasured variables. Differences were found between delirium and no delirium groups for some characteristics ( table 1 ); however, sensitivity analyses that simultaneously included all characteristics used in the matching process as covariates resulted in marginal increases in the risk estimates, suggesting limited residual differences in characteristics between groups.
For our dose-response analysis, data about the duration and severity of delirium episodes were not available, which limited the analysis to the number of episodes of care with coded delirium. It is also possible that the association found between delirium and incident dementia was induced by a confounding variable. For example, incremental increases in frailty in a patient with several hospital admissions (episodes) might underpin the increased risk of incident dementia. Frailty has been shown to affect the association between neuropathological burden and dementia diagnosis in community dwelling adults, 23 and gender might have a further impact on this association. 20 However, we tried to account for time varying differences in general health status by including the number of episodes (admissions) during the landmark period as a covariate.
While our results are consistent with the hypothesis that delirium might play a causative part in dementia, they are not conclusive owing to the fundamental limitations of observational studies in determining causality. Nevertheless, the results of this study provide valuable insights because prospective randomised controlled trials are unlikely to be conducted.
Conclusions
Using large scale hospital administration data, this study found a strong association between delirium and incident dementia in older adults without dementia at baseline. A dose-response association between delirium and dementia supports a causal pathway between the two conditions, encouraging the search for accelerated and de novo pathways to neuronal injury and the development of new treatment strategies. Differences in the association between delirium and incident dementia in men and women reinforce the need to not only adjust for gender in future studies but also to look for gender specific associations that might have important mechanistic and clinical implications. Delirium is a factor that could triple a person’s risk of dementia. Therefore, delirium prevention and treatment are opportunities to reduce dementia burden globally.
What is already known on this topic
An association might exist between delirium and subsequent dementia; however, the strength and nature of this association are unclear because of limitations in existing observational studies
As the global burden of dementia increases, it is important to confirm the extent to which delirium is a potentially modifiable risk factor
What this study adds
Among patients without dementia at baseline with at least one episode of delirium, the risk of a new dementia diagnosis was about three times higher than for patients without delirium; each additional episode of delirium increased the risk by 20%
The association between delirium and incident dementia seems to be stronger in men than in women
Delirium prevention and treatment could reduce the burden of dementia globally
Ethics statements
Ethical approval.
The study was approved by the New South Wales Population and Health Service Research Ethics Committee (2019/ETH12806/2019.55). The Committee granted a waiver of the usual requirement of consent for the use of reidentifiable information held by NSW agencies, in line with the State Privacy Commissioner’s Guidelines for Research and the Health Records and Information Privacy Act 2002 (NSW).
Data availability statement
The data used in this study are available to the public through application to the Centre for Health Record Linkage (see www.cherel.org.au for more information). The analysis script (R markdown file) is available for download from https://espace.library.uq.edu.au/view/UQ:dfc4e74
Contributors: EHG contributed to the study design and interpretation of the results, and drafted the manuscript. HX contributed to the study design, data extraction and analysis, and reviewed the manuscript. DDW contributed to the study design, data analysis and interpretation of the results, drafted the statistical analysis and results sections of the manuscript, and reviewed the manuscript. SB conceptualised the study, contributed to the study design, data analysis and interpretation of the results, and reviewed the manuscript. REH conceptualised the study, contributed to the study design and interpretation of the results, and reviewed the manuscript. HX and SB had access to the entire dataset and study sample dataset. DDW had access to extracted study sample data for the purposes of data analysis. All authors had access to the final study results and accept responsibility to submit for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. EHG is the guarantor.
Funding: HX’s work was supported by the National Health and Medical Research Council: Partnership Centre for Health System Sustainability. The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at https://www.icmje.org/disclosure-of-interest/ and declare: support from National Health and Medical Research Council: Partnership Centre for Health System Sustainability for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
The lead author (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: Study outcomes will be published and made publicly available. A lay summary has also been formulated. Clinician investigators will disseminate results through clinical conferences and clinical networks within hospital and primary health services. The Australian Frailty Network (AFN) will disseminate results to national and international research collaborators, partner organisations (eg, Australasian Association of Gerontology), and consumer networks, including the AFN and EWE (Eat Walk Engage) consumer networks. The key findings will be disseminated by the Partnership Centre for Health Systems Sustainability coordinated by the Australian Institute for Health Innovation at Macquarie University. Investigators will also disseminate results through social media and press releases.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- von Känel R ,
- Eurelings LS ,
- de Jonghe JF ,
- Kalisvaart KJ ,
- Eikelenboom P ,
- van Gool WA
- Goldberg TE ,
- Pereira JV ,
- Aung Thein MZ ,
- Nitchingham A ,
- Samelson EJ ,
- Richardson SJ ,
- Davis DHJ ,
- Stephan BCM ,
- Livingston G ,
- Huntley J ,
- Sommerlad A ,
- ↵ Centre for Health Record Linkage. CHeReL Master Linkage Key: NSW Health; 2023. www.cherel.org.au/datasets .
- World Health Organization
- Gilbert T ,
- Neuburger J ,
- Kraindler J ,
- Australian Commission on Safety and Quality in Health Care
- Austin PC ,
- Latouche A ,
- Leighton SP ,
- Herron JW ,
- Jackson E ,
- Sheridan M ,
- Deligianni F ,
- Garcez FB ,
- Apolinario D ,
- Campora F ,
- Curiati JAE ,
- Jacob-Filho W ,
- Avelino-Silva TJ
- Rolandi E ,
- Zaccaria D ,
- Vaccaro R ,
- Anstey KJ ,
- Mortby ME ,
- Ranson JM ,
- Wallace LMK ,
- Llewellyn DJ ,
- Eramudugolla R ,
- Chidiac B ,
- Ormseth CH ,
- Oldham MA ,
- Josephson SA ,
- Whitaker E ,
- Andrew MK ,
- Bennett DA ,
- Barnes LL ,
- Schneider JA
- Hildenbrand FF ,
- Boettger S ,
- Spiller T ,
- ↵ Burton J, Craig L, Yong S, Siddiqi N, Teale E, Woodhouse R, et al. Non-pharmacological interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev. 2021(11).
- Hshieh TT ,
- Gartaganis SL ,
- Khachaturian AS ,
- Hayden KM ,
- Devlin JW ,
- Cappetta K ,
- Phillipson L
- Pendlebury ST ,
- Lovett NG ,
- Thomson RJ ,
- Wilkinson T ,
- Schnier C ,
- UK Biobank Neurodegenerative Outcomes Group and Dementias Platform UK
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.12(1); 2020 Jan

Observational Study Designs: Synopsis for Selecting an Appropriate Study Design
Assad a rezigalla.
1 Department of Basic Medical Sciences, College of Medicine, University of Bisha, Bisha, SAU
The selection of a study design is the most critical step in the research methodology. Crucial factors should be considered during the selection of the study design, which is the formulated research question, as well as the method of participant selection. Different study designs can be applied to the same research question(s). Research designs are classified as qualitative, quantitative, and mixed design. Observational design occupies the middle and lower parts of the hierarchy of evidence-based pyramid. The observational design is subdivided into descriptive, including cross-sectional, case report or case series, and correlational, and analytic which includes cross-section, case-control, and cohort studies. Each research design has its uses and points of strength and limitations. The aim of this article to provide a simplified approach for the selection of descriptive study design.
Introduction and background
A research design is defined as the “set up to decide on, among other issues, how to collect further data, analyze and interpret them, and finally, to provide an answer to the question” [ 1 ]. The primary objective of a research design is to guarantee that the collected evidence allows the answering of the initial question(s) as clearly as possible [ 2 ]. Various study designs have been described in the literature [ 1 - 3 ]. Each of them deals with the specific type of research or research questions and has points of strength and weakness. Broadly, research designs are classified into qualitative and quantitative research and mixed methods [ 3 ]. The quantitative study design is subdivided into descriptive versus analytical study designs or as observational versus interventional (Figure (Figure1). 1 ). Descriptive designs occupy the middle and lower parts of the hierarchy of evidence-based medicine pyramid. Study designs are organized in a hierarchy beginning from the basic "case report" to the highly valued "randomised clinical trial" [ 4 - 5 ].

Case report
The case report describes an individual case or cases in their natural settings. Also, it describes unrecognized syndromes or variants, abnormal findings or outcomes, or association between risk factors and disease. It is the lowest level and the first line of evidence and usually deals with the newly emerging issues and ideas (Table (Table1) 1 ) [ 4 , 6 - 10 ].
Case series
A case series is a report on data from a subject group (multiple patients) without control [ 6 , 11 - 12 ]. Commonly, this design is used for the illustration of novel, unusual, or atypical features identified in medical practice [ 6 ]. The investigator is governed by the availability and accuracy of the records, which can cause biases [ 13 - 14 ]. Bias in a case series can be decreased through consecutive patient enrollment and predefined inclusion and exclusion criteria, explicit specification of study duration, and enrollment of participants (Table 2 ) [ 11 - 12 ].
Correlational study design
Correlational studies (ecologic studies) explore the statistical relationships between the outcome of interest in population and estimate the exposures. It deals with the community rather than in individual cases. The correlational study design can compare two or more relevant variables and reports the association between them without controlling the variables. The aim of correlational study design or research is to uncover any types of systematic relationships between the studied variables. Ecological studies are often used to measure the prevalence and incidence of disease, mainly when the disease is rare. The populations compared can be defined in several ways, such as geographical, time trends, migrants, longitudinal, occupation, and social class. It should be considered that in ecological studies, the results are presented at the population (group) level rather than individuals. Ecological studies do not provide information about the degree or extent of exposure or outcome of interest for particular individuals within the study group (Table 3 ) [ 7 , 15 - 16 ]. For example, we do not know whether those individuals who died in the study group under observation had higher exposure than those remained alive.
Cross-sectional study design
The cross-sectional study examines the association between exposures and outcomes on a snap of time. The assessed associations are guided by sound hypotheses and seen as hypothesis-generating [ 17 ]. This design can be descriptive (when dealing with prevalence or survey) or analytic (when comparing groups) [ 17 - 18 ]. The selection of participants in a cross-sectional study design depends on the predefined inclusion and exclusion criteria [ 18 - 19 ]. This method of selection limits randomization (Table 4 ).
Case-control study
A case-control study is an observational analytic retrospective study design [ 12 ]. It starts with the outcome of interest (referred to as cases) and looks back in time for exposures that likely caused the outcome of interest [ 13 , 20 ]. This design compares two groups of participants - those with the outcome of interest and the matched control [ 12 ]. The controls should match the group of interest in most of the aspects, except for the outcome of interest [ 18 ]. The controls should be selected from the same localization or setting of the cases [ 13 , 21 - 22 ]. Case-control studies can determine the relative importance of a predictor variable about the presence or absence of the disease (Table (Table5 5 ).
Cohort study design
The cohort study design is classified as an observational analytic study design. This design compares two groups, with exposure of interest and control one [ 12 , 18 , 22 - 24 ].
Cohort design starts with exposure of interest comparing them to non-exposed participants at the time of study initiation [ 18 , 22 , 24 ]. The non-exposed serve as external control. A cohort design can be either prospective [ 18 ] or retrospective [ 12 , 20 , 24 - 25 ]. In prospective cohort studies, the investigator measures a variety of variables that might be a risk factor or relevant to the development of the outcome of interest. Over time, the participants are observed to detect whether they develop the outcome of interest or not. In this case, the participants who do not develop the outcome of interest can act as internal controls. Retrospective cohort studies use data records that were documented for other purposes. The study duration may vary according to the commencement of data recording. Completion of the study is limited to the analysis of the data [ 18 , 22 , 24 ]. In 2016, Setia reported that, in some instances, cohort design could not be well-defined as prospective or retrospective; this happened when retrospective and prospective data were collected from the same participants (Table (Table6) 6 ) [ 24 ].
The selection of the study design is the most critical step in research methodology [ 4 , 26 ]. An appropriate study design guarantees the achievement of the research objectives. The crucial factors that should be considered in the selection of the study design are the formulated research question, as well as the method of sampling [ 4 , 27 ]. The study design determines the way of sampling and data analysis [ 4 ]. The selection of a research study design depends on many factors. Two crucial points that should be noted during the process selection include different study designs that may be applicable for the same research question(s) and researches may have grey areas in which they have different views about the type of study design [ 4 ].
Conclusions
The selection of appropriate study designs for research is critical. Many research designs can apply to the same research. Appropriate selection guarantees that the author will achieve the research objectives and address the research questions.
Acknowledgments
The author would like to acknowledge Dr. M. Abass, Dr. I. Eljack, Dr. K. Salih, Dr. I. Jack, and my colleagues. Special thanks and appreciation to the college dean and administration of the College of Medicine, University of Bisha (Bisha, Saudi Arabia) for help and allowing the use of facilities.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
ORIGINAL RESEARCH article
Enhancing sexual health and empowerment among migrant women sex workers: a community health worker-led intervention in marseille, france.

- 1 Aix Marseille Univ, INSERM, IRD, SESSTIM, Sciences Economiques and Sociales de la Santé and Traitement de l’Information Médicale, Aix Marseille Institute of Public Health ISSPAM, Marseille, France
- 2 ANRS-MIE, University of Health Sciences, Phnom Penh, Cambodia
- 3 Prospective Coopération NGO, Marseille, France
- 4 PHAReS, Centre INSERM U1218, Bordeaux Population Health, Université de Bordeaux, Bordeaux, France
- 5 Association AIDES, Pantin, France
- 6 Laboratoire de Recherche Communautaire, Coalition PLUS, Pantin, France
- 7 Unité des Virus Emergents (UVE), Aix-Marseille Université, IRD 190 INSERM 1207 EFS-IRBA, Marseille, France
Introduction: Given the high infection rate of sexually transmitted infections (STI) among migrant women sex workers (WSWs), it is necessary to understand how to improve prevention, information and care for this vulnerable population. Community health workers (CHWs), by linking community to health services, are positioned to improve health outcomes in migrant communities. This article aims to describe a pilot innovative intervention performed by CHWs to improve sexual health in migrant WSWs.
Methods: This one-year intervention study used a respondent-driven sampling (RDS) to recruit a representative cohort of migrant WSWs in Marseille, France. Four CHWs were recruited from different communities and participated in all stages of the research. They performed individual and group interventions of prevention, support in care and empowerment. Data on participant characteristics, type of intervention and adherence to the intervention were reported via questionnaires given to participants. Simultaneously, semi-structured interviews and informal interviews of migrant WSW, CHWs and care providers were carried out.
Results: A total of 132 migrant WSWs were included in the cohort. Very few of them knew about PrEP (12%) or already used HIV post-exposure treatment (9%). Migrant WSWs were often victims of rape or racism, 15 and 21%, respectively. In two-thirds of cases the level of health literacy was low. Participants suffered from a combination of vulnerability factors: difficulties with access to social rights, food or housing. Only 13% reported having benefited from medical follow-up or assistance by an NGO in the 3 months prior to the program. By 3 months, more than one third of the participants had been tested for HIV (35%) and 63% knew about PrEP. A total retention rate of 70% was reported in the cohort after 6 months.
Conclusion: CHWs enabled to improve care access for migrant WSWs by improving the collaboration between care and social actors at a local level. Through these “bring-back-to” interventions for this hard-to-reach population, CHWs enabled an optimization of the care pathway. Our results also highlight the importance of a population-based approach for individual and group support of empowerment interventions in order to strengthen their capacity for action.
1 Introduction
In Europe, the epidemic of HIV and sexually transmitted infections (STI) remains particularly active among migrants, who, along with men who have sex with men (MSM), are the populations who are the most vulnerable to these infections ( 1 ). Migrants, particularly those from sub-Saharan Africa, represent a significant proportion of people living with HIV in France (PLHIV). Although prevalence in their country of origin is high, a large proportion of these people contract HIV in France due to poor living conditions ( 2 ). Moreover, foreign-born PLHIV are also at risk of late detection ( 3 ). Finally, foreign-born PLHIV are characterized by a high proportion of women because they combine intersectional risks such as gender inequality, racism, insecurity and violence ( 4 ). All these data underline the importance of specific, optimized screening and prevention strategies.
Despite this context, there is a poor perception of risk and consequently little demand for PrEP among migrants ( 5 ). The main difficulties encountered by migrant women are unfamiliarity with prevention tools, difficulties in follow-up and in access to social rights. Other specificities that are insufficiently taken into account, such as problems related to contraception, pregnancy, relationships with partners, etc. require holistic approaches ( 5 ).
Woman sex workers (WSWs) also represent one of the key populations for controlling the HIV epidemic, due to them having a combination of social, economic and cultural risk factors ( 6 , 7 ). Several approaches have been tested to reduce HIV incidence in this population. Usually, access to condoms is at the heart of HIV prevention measures. However, these prevention methods are only partially effective ( 8 , 9 ). In fact, as has been demonstrated, WSWs are not necessarily in a position to impose this type of prevention, particularly for their regular partners ( 10 ). WSWs are also more frequently victims of violence which makes the use of this prevention tool difficult ( 10 , 11 ).
The ANRS-PARCOURS study showed that migrants experience a long period of insecurity upon arrival in France ( 2 ). In the PARCOURS study, factors linked to the likelihood of migrant women resorting to transactional relationships included the lack of housing and of residence permits ( 12 ). Thus, the factors of precariousness (housing, food, right to work, etc.) among migrant women are at the origin of SW activity. While community-based risk reduction programs for MSM have been successful, particularly in terms of levels of knowledge and access to PrEP, the same cannot be said for migrant populations ( 13 ).
All these factors point to the growing importance of community health programs in public health strategies. The development of these programs and the need for health mediation and Community Health Workers (CHWs) are now widely recognized, both nationally and internationally ( 14 , 15 ). Community health is thus an integral part of public health, representing a strategy within health promotion approaches. Its specific feature is that it is population-based rather than individual-based, and promotes and implements a holistic vision of health on a fine territorial level. In practice, benefits are expected at individual, community and institutional levels. The power of these programs lies in the fact that they aim to empower people and communities. However, evaluation and scaling up of community health initiatives are hampered by the length of time needed to measure their effects, and by the fact that they are often adapted to a specific context and not easily replicated or synchronized ( 16 ). In order to understand better the different levels at which community health interventions can act, detailed intervention descriptions are needed.
This article aims to describe, via a cohort conducted as part of a pilot intervention to improve sexual health in migrant WSWs, the characteristics of this population and the actions implemented by CHWs.
2 Materials and methods
2.1 study design.
This cohort, with a mixed method descriptive analysis, is an ancillary study of the FASSETS program (Favoriser l’Accés à la Santé SExuelle des Travailleuses du Sexe). The program protocol has already been published ( 17 ). The cohort was set up using Respondent-Driven Sampling (RDS). A 6-month follow-up was set up with a quantitative and qualitative evaluation. CHWs carried out the interventions throughout the follow-up period.
2.2 Community-based participatory research
The FASSETS study is a community-based participatory study. Community-based participatory research is an approach to research that involves a collective, reflective and systematic study in which the researcher and community stakeholders are involved in all stages of the research process with the aim of improving practices ( 18 ). This approach promotes shared control over individual and collective health and social conditions ( 19 , 20 ). The FASSETS project was initially developed around two community-based non-governmental organizations (NGOs): AIDES and The Truth, which provide community-based sexual and reproductive health interventions for migrant sex workers. These NGOs include CHWs from the communities involved in the research. In line with the principles of community-based participatory research, this study involved the creation of partnerships, regular exchanges between partners and community organizations/groups, and the sharing of experiences between researchers, CHWs and the community of migrant WSWs.
2.3 Population, study area and recruitment
2.3.1 study area.
The study sites included all of the medical and social care sites, including outreach activities, for migrant WSWs in Marseille, as well as the inclusion and follow-up site specific to the FASSETS study.
2.3.2 Population study
The study population included: (i) the 4 CHWs from Nigeria, Eastern Europe, Brazil and North Africa (two of the four are peer workers), (ii) the partners: health institutions and organizations involved in sexual health care in Marseille (Planning familial, Amicale du Nid, CEGIDD, AIDES, Autres Regards, COREVIH, ARS etc.) and (iii) the migrant WSWs accompanied by the FASSETS mediators.
2.3.3 Recruitment of migrant WSW
As migrant WSWs are a hidden population, the FASSETS study used the Respondent-Driven Sampling method to obtain a cohort as representative as possible of the different migrant WSW communities, whether or not they were already in the care system ( 21 ). There were 10 seeds in total, of different ages and belonging to cis or transgender women’s communities, who were from sub-Saharan Africa, North Africa, South America and Eastern Europe communities.
2.3.4 Inclusion criteria
The criteria for inclusion in the FASSETS cohort were: (i) cis or transgender women over 18 years of age, (ii) having provided sexual services in exchange for a service or monetary compensation during the last 12 months, (iii) born abroad, (iv) working, living or regularly passing through Marseille and (v) having signed a free and informed consent to take part in this study. Non-mastery of the French language was not a criterion for exclusion. Questionnaires and follow-up were conducted by CHWs in the participants’ native language.
2.4 Data collection
The FASSETS CHWs were previously trained in the survey technique by researchers and infectious disease physicians. They collected quantitative data from the migrant WSWs using a standardized tablet questionnaire. The interview method was face-to-face with CHWs in the participant’s native language for the first questionnaire and the two following ones. Additional follow-up by CHWs could be face-to-face, by telephone or via social networks, depending on needs. They also listed all the actions carried out and how they were implemented. Members of the project team worked with a team of sociologists to collect qualitative data from the WSWs. Data on partners was collected by questionnaires and focus groups.
Variables were collected through standardized questionnaires and included demographic characteristics, sex work characteristics, behavioral characteristics (alcohol use, drug use), medical history, level of health literacy and needs in sexual health. Perceived stress was measured using the Perceived Stress Scale (PSS) ( 22 ). A committee of experts from outside the study reviewed the questionnaire. Questions and variables were standardized on previous PARCOURS studies, on precariousness scales and on the conceptual framework for describing CHW activities previously validated in the literature ( 12 , 23 , 24 ).
For this ancillary study, only data collected between April (the start of the study) and November 2022 were analyzed.
2.5 Analysis
2.5.1 quantitative analysis.
Categorical variables were compared using Fisher’s exact test. Means were compared using Student’s t-test. The association between lost to follow-up and explanatory variables were assessed using univariate analysis. All p < 0.05 were considered statistically significant. Statistical analysis was carried out using R software (R Foundation for Statistical Computing, 3.3.1-Studio).
2.5.2 Qualitative analysis
An inductive approach was used, particularly adapted to exploratory research. Questions were focused on the needs and representation of sexual health and care among migrant WSWs. Health care providers, CHWs and migrant WSWs were interviewed. Migrant WSWs were encouraged to share specific experiences such as stories from their own lives to generate conversation. A revision workshop was organized where researchers provided a summary of the data collected to the participants in order to get their feedback and confirmation of results. The interviews and notes of these exchanges were transcribed and were subjected to manual thematic coding. A total of 13 semi-structured and 12 informal interviews were performed.
Qualitative and quantitative data were collected and analyzed, respectively, and simultaneously, followed by a triangulation of qualitative and quantitative data to interpret the results.
The protocol received approval from French Ethics Committee in October 2021 (no. 2021—A01746-35).
3.1 Characteristics of the migrant WSW participants
A total of 132 participants were included in the study. Table 1 provides population estimates of socio-demographic characteristics. More than half could not write ( n = 85/132, 65%) and the level of health literacy was low ( Table 1 ).
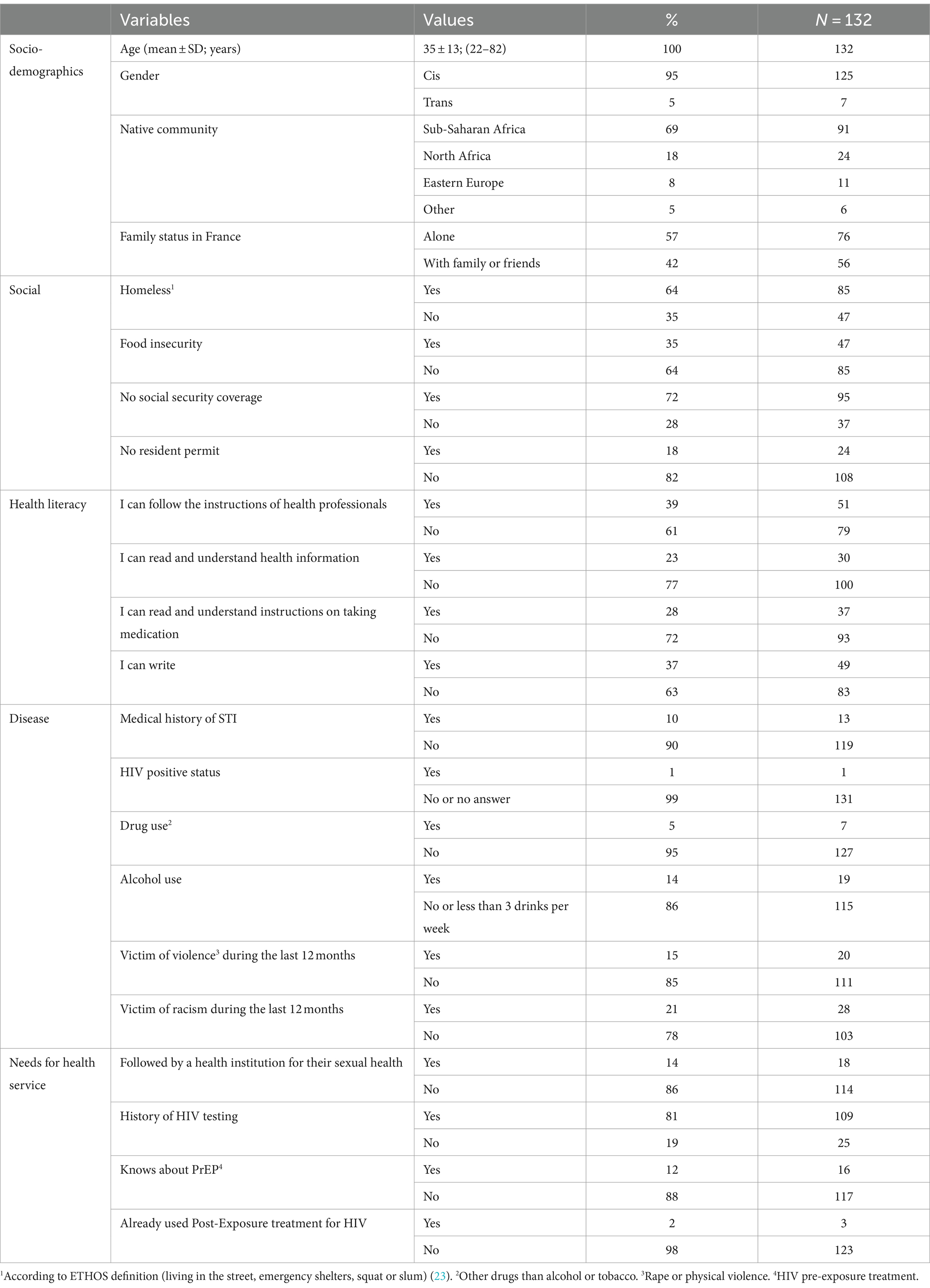
Table 1 . Socio-demographic, social, disease and needs of health service variables and indexes.
The majority of migrant WSWs were socially very vulnerable. In over half of the cases they were homeless, and they reported food insecurity or having no social security coverage or resident permit ( Table 1 ).
During the previous 12 months a significant number of participants reported having suffered from violence and racism ( Table 1 ).
The majority of participants (87%, n = 114) said that they had had no contact with NGOs or institutional care structures for their sexual health within the last 3 months.
Most Migrant WSW had children (87%, n = 115) with a mean of 2.12 children. They had been in France for an average of 7.8 years (SD = 10.1).
A total of 56% ( n = 56) of participants assessed had a low level of stress, 32% ( n = 30) a moderate level, and 12% ( n = 11) a high level of perceived stress according the PSS.
The RDS reported a near-perfect homophily of the communities network ( Figure 1 ). A total of 10 seeds were used. The RDS was stopped at the third wave for reasons of human resource capacity (CHWs) to monitor the recruited cohort correctly.
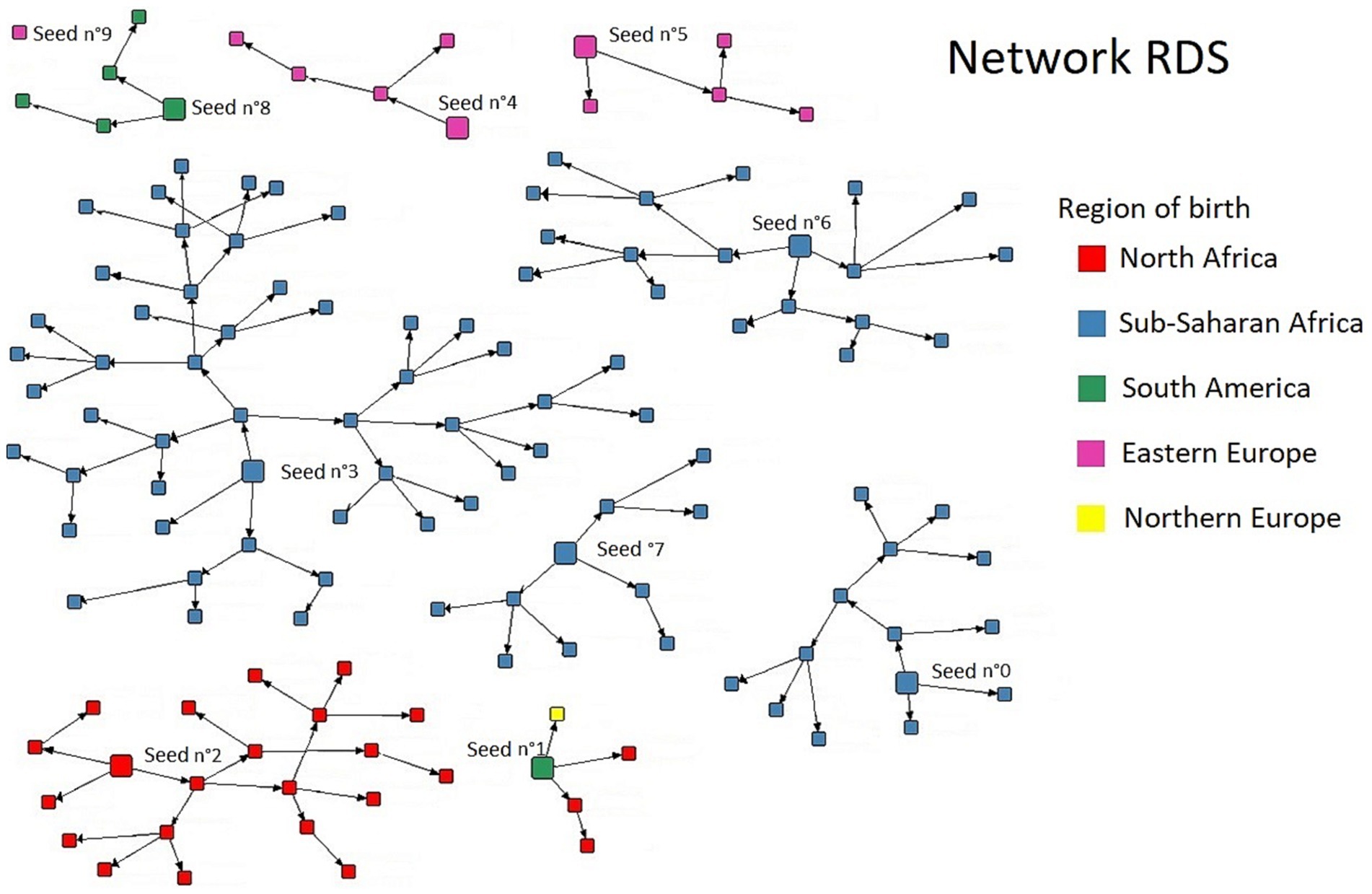
Figure 1 . Result of the respondent-driven sampling in migrant WSWs.
3.2 FASSETS activities of CHWs
A total of 4 CHWs were recruited from the various regions of origin of the migrant WSWs. Two of them were peer workers. All were women and one of them was transgender. CHWs activities are very varied, an example of a CHW’s activities is shown in Table 2 .
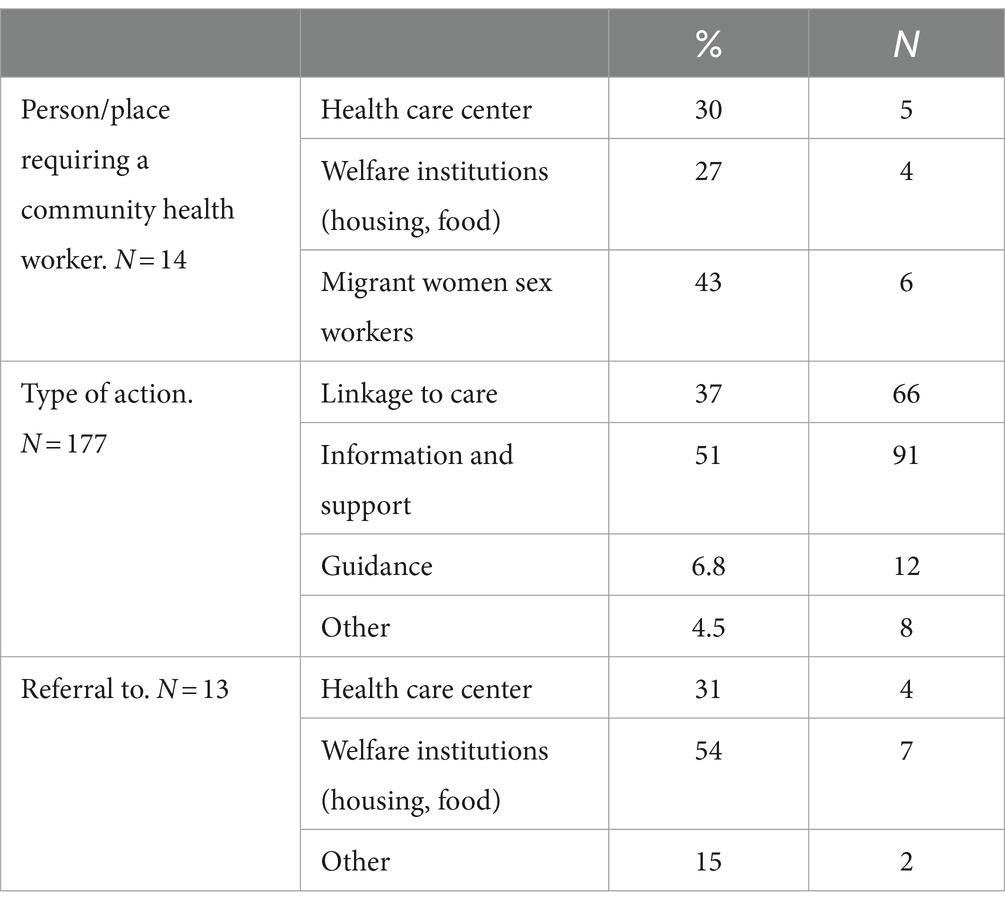
Table 2 . Example of the activity of one community health worker from April 2022 to November 2022.
The actions implemented by CHWs to improve the sexual health of migrant WSWs take place at different levels ( Table 3 ; Figure 2 ). At an individual level, it is necessary to perceive the person’s health needs (all the more difficult in the presence of discrimination or a competitiveness of needs, notably here with access to social rights, food and family needs), then to improve levels of knowledge in sexual health and facilitate access to care. Taking into account past experiences, vicarious experiences, medical history and perceptions also play a role in the migrant WSWs’ self-efficacy and capacity to act. The CHWs also work on a collective and social level to gain recognition of the participants’ specificities, notably when setting up care pathways dedicated to women (adaptation of the care system) or their advocacy actions ( Figures 2 , 3 ).
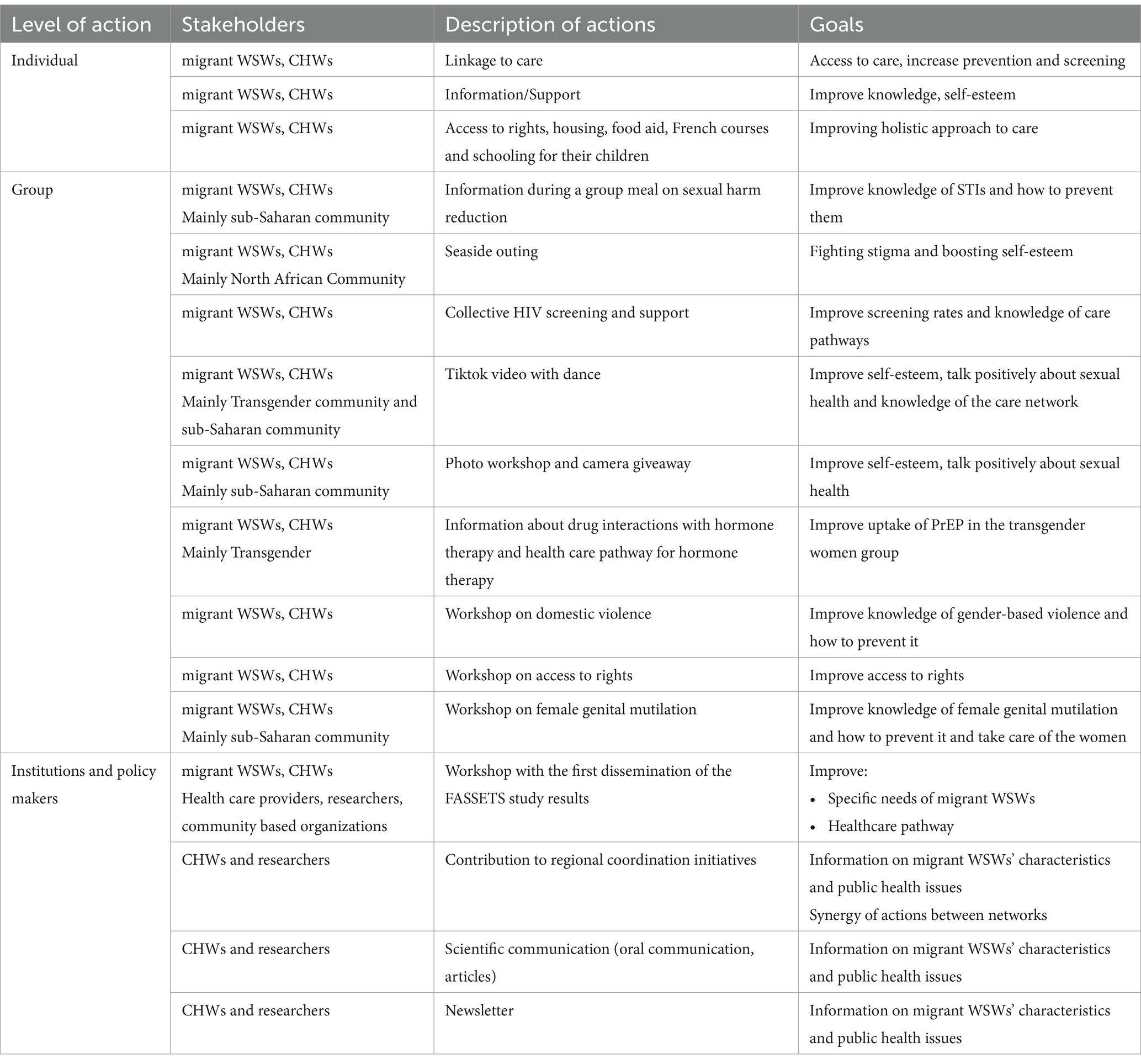
Table 3 . Description of actions carried out among and with migrant women sex workers.
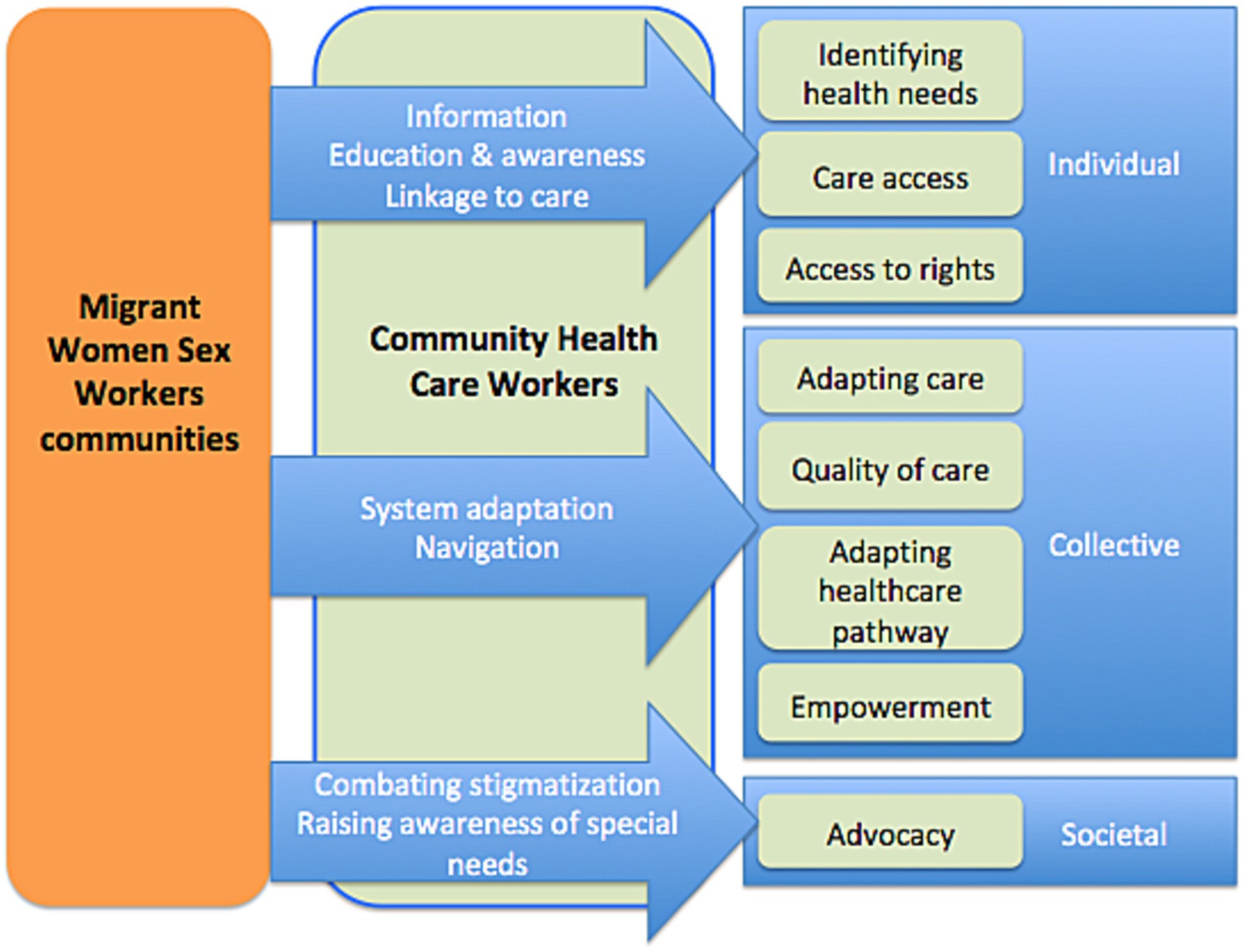
Figure 2 . Type and level of community health workers health actions with migrant women sex workers.

Figure 3 . Example of an empowerment group for Nigerian women on sexual health and information about PrEP.
It is clear from these actions ( Table 3 ) that the CHWs enable the needs formulated by the MWSWs to be incorporated into collective actions and have an impact on institutions ( Figure 2 ).
CHWs take into account the complex intersections between structural barriers affecting migrant WSWs and their gender, education, race, and socio-economic status. Based on the needs expressed by migrant WSWs, CHWs not only optimize access to care but also impact it by encouraging adaptations ( Figure 2 ).
3.3 Qualitative multilevel assessment (migrant WSWs, CHWs and health care providers), different needs according to communities
The results of the interviews showed that cisgender women differ from transgender women (TGW) in their perception of the sexual health risks to which they are exposed, in their knowledge of prevention tools and in the expression of their needs to the medical-social sector.
“Normally South American [trans] girls are mainly looking for access to care, health, help with their papers, it’s stuff… frankly it’s light… when they arrive at the association they know what they’re looking for, what they want… it’s different from Nigerian girls where you have to unpack the whole package to try and find out what they want…” (CHW, sex workers NGO).
For the NGOs, TGW are more receptive to sexual health issues. According to health care workers, migrant TGW feel much more “at risk” of contracting HIV and other STIs than migrant cisgender women.
There are also community-specific characteristics, particularly among Nigerian women, related to the violence and trauma of migration.
“As I was telling you earlier, there's normal prostitution and forced prostitution… and right now we’re taking much more care of Nigerian girls than other WSWs at the association… 70% of our active file I think. As these are girls who have experienced rape, exploitation… they don’t see prostitution as work…” (Health mediator, association for sex workers).
The migrant WSWs interviewed frequently told stories of rape, particularly during their migration pathway. Most of the Nigerian women reported psychosomatic trauma, and said they were not treated for post-traumatic stress disorder due to a lack of English-speaking psychologists, who also refused to treat migrants without documents. Migrant WSWs from North Africa, who have been living in France for longer, reported a particular need to fight stigmatization and build social ties. Eastern European migrant WSWs reported frequent trips back to their home countries to see their families and often their children, limiting their follow-up in care facilities.
Participants, particularly those of sub-Saharan origin, also often mentioned the notion of excision and lack of knowledge of their own body.
“Most don’t know if they have been or not” (Health care worker talking about genital mutilation/cutting).
3.4 Impact of community health interventions during follow-up and retention
Upon inclusion, 28% ( n = 37/132) of migrant WSWs felt that the CHWs could not help them with their sexual health. Moreover, the vast majority of migrant WSWs (69%, n = 93/132) provided no help to their peers to improve their sexual health.
At 3 months, 63% ( n = 60/95) of participants knew about PrEP. A total of 21% of migrant WSWs were referred to care for their sexual health needs. More than one third of participants had been tested for HIV (34%, n = 33/95).
At 6 months of follow-up, 45% ( n = 42/93) of migrant WSWs declared having asked the CHWs for help with their care.
At 3 and 6 months of follow-up by the CHWs, the cohort retention rates were 72 and 70%, respectively.
4 Discussion
This study used a community-based recruitment and follow-up method. The main results from the migrant population showed relatively closed networks and community-specific needs. CHWs were able to set up multi-level actions with the migrant WSWs, while adapting to the local healthcare offer and the needs of each community.
The RDS network results of our study showed a significant compartmentalization of the migrant WSWs network. These sub-networks are structured around communities of belonging linked to the migrant WSWs country and geographic region of origin. Indeed, these results show the importance of community mediation actions investing in these sub-networks. Few studies exist about the characteristics of interactions between sex workers ( 25 ). Some studies provide some information about exchanges of social support and others resources between partners, clients, peers or co-workers ( 26 , 27 ), but data is lacking on the organization and quality of the relationships described. Indeed, trust between migrant WSWs and CHWs is a key element in the linkage to care. Here we show that groups are compartmentalized, have different needs and require specific actions. The TGW community seemed, in our program, to have a better understanding of STI prevention issues than cisgender migrant women. One hypothesis is that they benefit more from the LGBTQ+ community network and targeted communication campaigns. TGWs may also benefit from information and support via LGBTQ+ Social Network apps ( 28 ). Furthermore, other studies comparing cis and transgender black women have shown that beyond gender, it is access to employment that is linked to prevention practices ( 29 ). Unfortunately, we can also confirm, notably in the sub-Saharan community, the high rate of post-traumatic stress disorder linked to the violence experienced during the migration pathway, and its consequences in terms of mental health ( 30 , 31 ).
CHWs seem to be able to adapt actions to needs at individual and collective levels. They also enable institutions to adapt themselves in terms of care provision or recognition of specific community health needs. This study is exploratory but seems to show an impact even after 3 months on knowledge and screening practices. These results need to be confirmed with longer follow-up times and larger groups.
These results also showed women with a combination of vulnerability factors: lack of housing, multiple forms of violence and food insecurity. This calls for a complex, holistic approach on multiple levels. Indeed, the WHO is increasingly recommending integrated approaches for STI prevention and care ( 32 ). Levels of insecurity are high and probably lead to significant risk-taking ( 2 ). The participants have to meet their own needs as well as those of their families, and studies have shown that the presence of dependent children exacerbates the need for money and sexual risk-taking ( 33 ). There is a competitiveness of needs, with those of the children always taking precedence over those of the mother. Illegal status on the territory, lack of housing, multiple forms of violence and food insecurity mean that migrant WSWs need an approach that prioritizes their urgent needs. Numerous studies and “housing first” programs have shown that, in order to be effective, all preventive and therapeutic actions must first ensure the safety of the beneficiaries ( 34 ). Given the complexity of needs, CHWs could help optimize access to local resources, but this would clearly not be sufficient in a context of chronic lack of accommodation and food aid in France for the most vulnerable ( 35 ).
Community health work involves information-, education-, and communication-based activities, as well as health system navigation activities, and includes activities to involve professionals, stakeholders and communities. Health mediation is thus both a promising intervention (“one whose effectiveness has not been evaluated by research, but for which a solid normative evaluation induces a presumption of relevant results” ( 36 )) and a complex one to study, in that it combines varied practices that require constant adaptation to a socially shifting context. Our results show that community health interventions with empowerment actions are part of an ecological concept that applies to interactive change at several levels: the individual, the organization and the community ( 37 ). Working on mediation issues therefore implies studying not only individual changes, but also changes in the social setting itself. In fact, to our knowledge, with the exception of some pioneering studies ( 38 , 39 ), no study has been able to demonstrate its effectiveness by taking into account the conditions of the effect of mediation on health, because this evaluation requires integrating all this complexity. In fact, as mentioned above, healthcare mediation practices are multi-faceted, constantly adapting and multi-level ( 24 ). They make up an interventional system centered around the individual ( 40 ). Following this systemic approach, Richard et al. ( 20 ) proposed to map the theoretical conditions of feasibility and success of health mediation to promote the use of health services within a conceptual framework characterizing their potential interrelationships, which it would be interesting to map out in real life.
This study provides community data from a hidden key population, who are without linkage to care. Indeed, migrant WSWs do not receive care in the usual screening centers in the study region ( 41 ). Specific information on these communities is required to control the STI epidemic. More and more studies and programs are using RDS to reach these populations and enable specific interventions ( 42 , 43 ). Furthermore, our findings demonstrated that migrant WSWs were able to recruit others, regardless of the level of education or vulnerability, showing how RDS could reach participants, even those with an illegal status and not followed by the NGOs network, within a short recruitment period. To our knowledge, this is the first RDS study in France on sex workers or on migrants. However, other RDS studies have been successfully carried out in other countries among sex worker populations ( 44 , 45 ).
Some limitations have to be acknowledged. The study’s findings may lack generalizability due to its specific focus on Marseille and a relatively small sample size. Sampling bias and the absence of a control group limit the ability to establish a causal relationship between community health worker interventions and observed outcomes. The small size of the study population precluded extensive multivariate analysis, especially of subgroups. The short six-month follow-up period may not capture sustained changes over time. Additionally, reliance on self-reported data introduces the potential for recall and social desirability biases. However, this is important exploratory research within a difficult-to-reach population, which will allow us to set up more specific interventional studies.
In conclusion, CHWs can carry out complex and comprehensive interventions with migrant WSWs. This key population has multiple vulnerability factors and requires a holistic approach that takes into account different levels of network: the women’s family (especially their children), their community of origin to which they seem extremely connected, and the local care network to which they have little access despite their substantial needs. Other studies are required, using specific methodologies, to evaluate CHW actions, their acceptability, their cost effectiveness, and their impact on the health of beneficiaries and on public health. Finally, these actions carried out by harm-reduction CHWs should be accompanied by public policy measures to help secure the most vulnerable people, at the very least in terms of protection from stigma, discrimination and violence, and by providing emergency accommodation and food aid.
Data availability statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by French Ethics Committee in October 2021 (no. 2021—A01746-35). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any identifiable images or data included in this article.
Author contributions
EM: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization. MH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing, Supervision. FA: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. HR: Data curation, Methodology, Validation, Writing – review & editing. ER: Conceptualization, Methodology, Validation, Writing – review & editing. DM: Conceptualization, Methodology, Validation, Writing – review & editing. MM: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Validation, Writing – review & editing. GI: Data curation, Investigation, Project administration, Validation, Writing – review & editing. MR: Conceptualization, Data curation, Project administration, Writing – review & editing. BS: Conceptualization, Methodology, Supervision, Writing – review & editing. SV: Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing. ML: Data curation, Funding acquisition, Project administration, Resources, Validation, Writing – review & editing. CE: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – review & editing. PR: Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Sidaction grant number [2020-2-AEQ-12890], by the city of Marseille and by ViiV Healthcare.
Acknowledgments
The authors thank all participants, The Operational Team and NGOs and Especially Prospective Coopération, l’Amicale du Nid, Autres Regards, AIDES and the truth for their support and help.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. European Centre for Disease Prevention and Control, World Health Organization . HIV/AIDS Surveillance in Europe 2020: 2019 Data . LU: Publications Office (2020).
Google Scholar
2. Desgrees-du-Lou, A, Pannetier, J, Ravalihasy, A, Le Guen, M, Gosselin, A, Panjo, H, et al. Is hardship during migration a determinant of HIV infection? Results from the ANRS PARCOURS study of sub-Saharan African migrants in France. AIDS . (2016) 30:645–56. doi: 10.1097/QAD.0000000000000957
PubMed Abstract | Crossref Full Text | Google Scholar
3. De Monteynard, L-A . Infection Par le VIH Chez les Patients Migrants Suivis en France. [PhD Thesis] , vol . 6. Paris:theses.hal.science (2016).
4. Cazein, F, Lot, F, Pillonel, J, Le Strat, Y, Sommen, C, Pinget, R, et al. Découvertes de séropositivité VIH et de sida, France, 2003-2013. Bull Epidémiol Hebd . (2015) 9:152Á61.
5. Hadj, L, Desgrées du Loû, A, Dupont, J, and Nguyen, V-K. Acceptabilité et freins chez les populations africaines et caribéennes vivant en Ile-de-France d’une nouvelle offre de prévention du VIH: le Truvada en prophylaxie pré-exposition (PrEP): une enquête exploratoire. Bulletin Epidemiologique Hebdomadaire . (2017) 6:110–4.
6. Baral, S, Beyrer, C, Muessig, K, Poteat, T, Wirtz, AL, Decker, MR, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis . (2012) 12:538–49. doi: 10.1016/S1473-3099(12)70066-X
7. Scorgie, F, Chersich, MF, Ntaganira, I, Gerbase, A, Lule, F, and Lo, Y-R. Socio-demographic characteristics and behavioral risk factors of female sex workers in sub-saharan Africa: a systematic review. AIDS Behav . (2012) 16:920–33. doi: 10.1007/s10461-011-9985-z
8. Weller, S, and Davis, K. Condom effectiveness in reducing heterosexual HIV transmission. Cochrane Database Syst Rev . (2002) 2012:CD003255. doi: 10.1002/14651858.CD003255
Crossref Full Text | Google Scholar
9. Wilson, AL . A systematic review and Meta-analysis of the efficacy and safety of intermittent preventive treatment of malaria in children (IPTc). PLoS One . (2011) 6:e16976. doi: 10.1371/journal.pone.0016976
10. Parriault, M-C, Basurko, C, Melle, AV, Gaubert-Maréchal, E, Rogier, S, Couppié, P, et al. Predictive factors of unprotected sex for female sex workers: first study in French Guiana, the French territory with the highest HIV prevalence. Int J STD AIDS . (2015) 26:542–8. doi: 10.1177/0956462414545794
11. Parriault, M-C, van Melle, A, Basurko, C, Gaubert-Marechal, E, Macena, RHM, Rogier, S, et al. HIV-testing among female sex workers on the border between Brazil and French Guiana: the need for targeted interventions. Cad Saude Publica . (2015) 31:1615–22. doi: 10.1590/0102-311X00138514
12. Desgrées du, LA, Pannetier, J, Ravalihasy, A, Gosselin, A, Supervie, V, Panjo, H, et al. Migrants subsahariens suivis pour le VIH en France: combien ont été infectés après la migration?: estimation dans l’étude ANRS-Parcours. Bull Epidémiol Hebd . (2015) 40:752–8.
13. Puppo, C, Spire, B, Morel, S, Génin, M, Béniguel, L, Costagliola, D, et al. How PrEP users constitute a community in the MSM population through their specific experience and management of stigmatization. The example of the French ANRS-PREVENIR study. AIDS Care . (2020) 32:32–9. doi: 10.1080/09540121.2020.1742863
14. de Santé, HA . La Médiation en Santé Pour les Personnes Éloignées des Systèmes de Prévention et de Soins. Référentiel de Compétences, Formations et Bonnes Pratiques, Rapport Final Haute Autorité de Santé (HAS) (2017)
15. Sarriot, E, Davis, T, Morrow, M, Kabore, T, and Perry, H. Motivation and performance of community health workers: nothing new under the Sun, and yet …. Glob Health Sci Pract . (2021) 9:716–24. doi: 10.9745/GHSP-D-21-00627
16. Cometto, G, Ford, N, Pfaffman-Zambruni, J, Akl, EA, Lehmann, U, McPake, B, et al. Health policy and system support to optimise community health worker programmes: an abridged WHO guideline. Lancet glob. Health . (2018) 6:e1397–404. doi: 10.1016/S2214-109X(18)30482-0
17. Mosnier, E, Artigas, F, Richard, E, Hoyer, M, Michels, D, Vandentorren, S, et al. Effectiveness of a community empowerment intervention to improve access to pre-exposure prophylaxis in migrant women sex workers: protocol for a mixed methods implementation study. JMIR Res Protoc . (2023) 12:e42844. doi: 10.2196/42844
18. Ridde, V . Suggestions d’ameliorations d’un cadre conceptuel de l’evaluation participative. Can J Program Eval . (2006) 21:1–23. doi: 10.3138/cjpe.21.001
19. Baum, F, MacDougall, C, and Smith, D. Participatory action research. J Epidemiol Community Health . (2006) 60:854–7. doi: 10.1136/jech.2004.028662
20. Tremblay, M-C, Martin, DH, McComber, AM, McGregor, A, and Macaulay, AC. Understanding community-based participatory research through a social movement framework: a case study of the Kahnawake schools diabetes prevention project. BMC Public Health . (2018) 18:487. doi: 10.1186/s12889-018-5412-y
21. Malekinejad, M, Johnston, LG, Kendall, C, Kerr, LR, Rifkin, MR, and Rutherford, GW. Using respondent-driven sampling methodology for HIV biological and behavioral surveillance in international settings: a systematic review. AIDS Behav . (2008) 12:S105–30. doi: 10.1007/s10461-008-9421-1
22. Yılmaz Koğar, E, and Koğar, H. A systematic review and meta-analytic confirmatory factor analysis of the perceived stress scale (PSS-10 and PSS-14). Stress Health . (2023) 40:e3285. doi: 10.1002/smi.3285
23. ETHOS . Typology on Homelessness and Housing Exclusion. (2017). Available at: https://www.feantsa.org/en/toolkit/2005/04/01/ethos-typology-on-homelessness-and-housing-exclusion (Accessed March 15, 2021)
24. Richard, E, Vandentorren, S, and Cambon, L. Conditions for the success and the feasibility of health mediation for healthcare use by underserved populations: a scoping review. BMJ Open . (2022) 12:e062051. doi: 10.1136/bmjopen-2022-062051
25. Shushtari, ZJ, Hosseini, SA, Sajjadi, H, Salimi, Y, Latkin, C, and Snijders, TAB. Social network and HIV risk behaviors in female sex workers: a systematic review. BMC Public Health . (2018) 18:1020. doi: 10.1186/s12889-018-5944-1
26. Chen, Y, Latkin, C, Celentano, DD, Yang, X, Li, X, Xia, G, et al. Delineating interpersonal communication networks: a study of the diffusion of an intervention among female entertainment workers in Shanghai, China. AIDS Behav . (2012) 16:2004–14. doi: 10.1007/s10461-012-0214-1
27. Reisner, SL, Mimiaga, MJ, Bland, S, Mayer, KH, Perkovich, B, and Safren, SA. HIV risk and social networks among male-to-female transgender sex workers in Boston. Massachusetts J Assoc Nurses AIDS Care . (2009) 20:373–86. doi: 10.1016/j.jana.2009.06.003
28. Sun, CJ, Sutfin, E, Bachmann, LH, Stowers, J, and Rhodes, SD. Comparing men who have sex with men and transgender women who use Grindr, other similar social and sexual networking apps, or no social and sexual networking apps: implications for recruitment and health promotion. J AIDS Clin Res . (2018) 9:757. doi: 10.4172/2155-6113.1000757
29. Rutledge, JD, Anderson-Carpenter, K, and Puckett, J. HIV testing and associated characteristics among black cisgender and transgender women in the United States. J Healthc Sci Humanit . (2021) 11:149–62.
PubMed Abstract | Google Scholar
30. Khouani, J, Blatrix, L, Tinland, A, Jego, M, Gentile, G, Fond, G, et al. Health status of recently arrived asylum seekers in their host country: results of a cross-sectional observational study. BMC Public Health . (2022) 22:1688. doi: 10.1186/s12889-022-14095-8
31. Khouani, J, Landrin, M, Boulakia, RC, Tahtah, S, Gentile, G, Desrues, A, et al. Incidence of sexual violence among recently arrived asylum-seeking women in France: a retrospective cohort study. Lancet Regional Health Europe . (2023) 34:100731. doi: 10.1016/j.lanepe.2023.100731
32. WHO . Consolidated Guidelines on HIV, Viral Hepatitis and STI Prevention, Diagnosis, Treatment and Care for Key Populations . Geneva, Switzerland: World Health Organization (2022).
33. Hao, C, Guida, J, Morisky, DE, and Liu, H. Family network, workplace network, and their influence on condom use: a qualitative study among older female sex Workers in China. J Sex Res . (2015) 52:924–35. doi: 10.1080/00224499.2014.973101
34. Baxter, AJ, Tweed, EJ, Katikireddi, SV, and Thomson, H. Effects of housing first approaches on health and well-being of adults who are homeless or at risk of homelessness: systematic review and meta-analysis of randomised controlled trials. J Epidemiol Community Health . (2019) 73:379–87. doi: 10.1136/jech-2018-210981
35. La Fondation Abbé Pierre . 28e Rapport Sur l’état du Mal-Logement en France 2023. (2023). Available at: https://www.fondation-abbe-pierre.fr/actualites/28e-rapport-sur-letat-du-mal-logement-en-france-2023
36. Lacouture, A. Etat de l’art des Dispositifs mis en Oeuvre à l’étranger pour Favoriser Auprès des Décideurs le Recours aux Données sur des Interventions Probantes ou Prometteuses dans le Champ de la Prévention ou de la Promotion de la Santé . EHESP Eole Des Hautes Etudes en Santé Publique (2016).
37. Wallerstein, N . Powerlessness, empowerment, and health: implications for health promotion programs. Am J Health Promot . (1992) 6:197–205. doi: 10.4278/0890-1171-6.3.197
38. Musso, S, and Delaquaize, H. Réinventer la roue? La difficile capitalisation des expériences de médiation en santé en France In: Convention Nationale 2016 Sidaction . HAL science Paris, France: Mairie de Paris; Sidaction (2016). 1–20.
39. DGS . Évaluation des Actions de Proximité des Médiateurs de Santé Publique et de Leur Formation dans le Cadre d’un Programme Expérimental mis en Oeuvre par l’IMEA . Direction Générale de la Santé (2006)
40. Cambon, L, Terral, P, and Alla, F. From intervention to interventional system: towards greater theorization in population health intervention research. BMC Public Health . (2019) 19:339. doi: 10.1186/s12889-019-6663-y
41. Eldin, C, Hoyer, M, Martinet, P, Saule, J, Villermy, P, Inegbeze, G, et al. There Is Still a Long Way to Go to Facilitate PrEP Use in Migrant Women Sex Workers . ESCMID congress 2022 (2023).
42. Nagot, N, D’Ottavi, M, Quillet, C, Debellefontaine, A, Castellani, J, Langendorfer, N, et al. Reaching hard-to-reach people who use drugs: a community-based strategy for the elimination of hepatitis C. Open Forum Infect Dis . (2022) 9:ofac181. doi: 10.1093/ofid/ofac181
43. Des Jarlais, D, Duong, HT, Pham Minh, K, Khuat, OHT, Nham, TTT, Arasteh, K, et al. Integrated respondent-driven sampling and peer support for persons who inject drugs in Haiphong, Vietnam: a case study with implications for interventions. AIDS Care . (2016) 28:1312–5. doi: 10.1080/09540121.2016.1178698
44. de Matos, MA, da França, DD, Carneiro, MADS, Martins, RMB, Kerr, LRFS, Caetano, KAA, et al. Viral hepatitis in female sex workers using the respondent-driven sampling. Rev Saude Publica . (2017) 51:65. doi: 10.1590/S1518-8787.2017051006540
45. Mbunda, T, Tarimo, EAM, Bakari, M, Sandström, E, and Kulane, A. Recruitment using respondent driven sampling, risk behaviors assessment and willingness of young female sex workers (18–25 years) in Dar Es Salaam, Tanzania to participate in HIV vaccine trials. BMC Public Health . (2019) 19:1537. doi: 10.1186/s12889-019-7822-x
Keywords: community health interventions, women sex workers, migrants, cohort, community-based participatory research, health promotion, community health workers
Citation: Mosnier E, Hoyer M, Artigas F, Regnault H, Richard E, Michels D, Mosnier M, Inegbeze G, Robledo MS, Spire B, Vandentorren S, Lescaudron M, Eldin C and Roux P (2024) Enhancing sexual health and empowerment among migrant women sex workers: a community health worker-led intervention in Marseille, France. Front. Public Health . 12:1359363. doi: 10.3389/fpubh.2024.1359363
Received: 21 December 2023; Accepted: 21 February 2024; Published: 27 March 2024.
Reviewed by:
Copyright © 2024 Mosnier, Hoyer, Artigas, Regnault, Richard, Michels, Mosnier, Inegbeze, Robledo, Spire, Vandentorren, Lescaudron, Eldin and Roux. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emilie Mosnier, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

IMAGES
VIDEO
COMMENTS
When to use a cohort study. Cohort studies are a type of observational study that can be qualitative or quantitative in nature. They can be used to conduct both exploratory research and explanatory research depending on the research topic.. In prospective cohort studies, data is collected over time to compare the occurrence of the outcome of interest in those who were exposed to the risk ...
The cohort study design is an excellent method to understand an outcome or the natural history of a disease or condition in an identified study population ... A review of cohort study design for cardiovascular nursing research. J Cardiovasc Nurs, 24 (6), E1-9. doi: 10.1097/JCN.0b013e3181ada743 ...
Cohort studies are types of observational studies in which a cohort, or a group of individuals sharing some characteristic, are followed up over time, and outcomes are measured at one or more time points. ... Cohort Studies: Design, Analysis, and Reporting Chest. 2020 Jul;158(1S):S72-S78. doi: 10.1016/j.chest.2020.03.014. Authors Xiaofeng ...
Keywords: Cohort study, research design, prospective study, retrospective study, STROBE guidelines, India Previous articles in this series on research design discussed classifications in research design 1 and prospective and retrospective, cross- sectional and longitudinal studies. 2 This article examines a specific research design that is ...
Case‐control studies based within a defined cohort is a form of study design that combines some of the features of a cohort study design and a case‐control study design. When a defined cohort is embedded in a case‐control study design, all the baseline information collected before the onset of disease like interviews, surveys, blood or ...
A study design where one or more samples (called cohorts) are followed prospectively and subsequent status evaluations with respect to a disease or outcome are conducted to determine which initial participants exposure characteristics (risk factors) are associated with it. As the study is conducted, outcome from participants in each cohort is ...
Previous articles in this series on research design discussed classifications in research design 1 and prospective and retrospective, cross- sectional and longitudinal studies. 2 This article examines a specific research design that is increasingly being employed in medicine and psychiatry: the cohort study.
Cohort studies are a powerful tool for conducting research in human populations. They are a type of longitudinal study design. Longitudinal studies follow participants over a period of time.
Cohort studies can be either prospective or retrospective. The type of cohort study is determined by the outcome status. If the outcome has not occurred at the start of the study, then it is a prospective study; if the outcome has already occurred, then it is a retrospective study. 4 Figure 1 presents a graphical representation of the designs of prospective and retrospective cohort studies.
Cohort Studies Examined from the perspective of research design, cohort studies are empir-ical because they collect and examine data. They are sample-based because a group of individuals is studied. They are always longitudinal because there is a follow-up, but can be prospectively HOW TO CITE THIS ARTICLE: Andrade C. Research Design: Cohort ...
A study combining two study designs, the case-cohort design, is a combination of a case-control and cohort design that can be either prospective or retrospective. The case-cohort design can be viewed as a variant of the nested case-control design.7 In a nested case-control study, one starts with identifying cases that have already
A prospective cohort study is a type of longitudinal research where a group of individuals sharing a common characteristic (cohort) is followed over time to observe and measure outcomes, often to investigate the effect of suspected risk factors. In a prospective study, the investigators will design the study, recruit subjects, and collect ...
A cohort is a group of individuals that share a common exposure or experience over a similar time period. Cohort studies are commonly used in medical practice because they offer a high level of evidence, provide useful data and offer flexibility in terms of their structure. They are a type of observational study, where a group of individuals is ...
What is a Cohort Study design? Cohort studies are longitudinal, observational studies, which investigate predictive risk factors and health outcomes. ... Journal of Psychosomatic Research, 101, 24-30. Forman, J.P., Stampfer, M.J. & Curhan, G.C. (2009). Diet and lifestyle risk factors associated with incident hypertension in women.
Despite the ease of conducting cohort studies and the research value of such studies, few centers with long-term research goals conduct such studies. This article provides easy-to-understand practical guidance on how to start and run a cohort study. Key words: Cohort study, research design, schizophrenia A n earlier article1 in this series ex-
It is a type of nonexperimental or observational study design. The term "cohort" refers to a group of people who have been included in a study by an event that is based on the definition decided by the researcher. For example, a cohort of people born in Mumbai in the year 1980. This will be called a "birth cohort.".
A cohort study is a particular form of longitudinal study that samples a cohort ... treatment, or exposure is administered to participants in a cohort design; and no control group is defined. ... Shorter term studies are commonly used in medical research as a form of clinical trial, or means to test a particular hypothesis of clinical ...
A prospective study, sometimes called a prospective cohort study, is a type of longitudinal study where researchers will follow and observe a group of subjects over a period of time to gather information and record the development of outcomes.. The participants in a prospective study are selected based on specific criteria and are often free from the outcome of interest at the beginning of the ...
First, by the specific research question. That is, if the question is one of 'prevalence' (disease burden) then the ideal is a cross-sectional study; if it is a question of 'harm' - a case-control study; prognosis - a cohort and therapy - a RCT. Second, by what resources are available to you. This includes budget, time, feasibility re-patient ...
Center for Cohort Studies, Total Healthcare Center, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Samsung Main Building B2, 250 Taepyung-ro 2ga, Jung-gu, Seoul 04514 ... Department of Clinical Research Design and Evaluation, SAIHST, Sungkyunkwan University, 115, Irwon-ro, Gangnam-gu, Seoul 06355, Republic of Korea.
Research study design is a framework, or the set of methods and procedures used to collect and analyze data on variables specified in a particular research problem. ... Typically, most cohort studies are prospective studies (though there may be retrospective cohorts), whereas case-control studies are retrospective studies. An interventional ...
A study design where one or more samples (called cohorts) are followed prospectively and subsequent status evaluations with respect to a disease or outcome are conducted to determine which initial participants exposure characteristics (risk factors) are associated with it. As the study is conducted, outcome from participants in each cohort is ...
Objective To examine the influence of having a baseline metabolic disorder (diabetes, hypertension, and/or obesity) on the risk of developing new clinical sequelae potentially related to SARS-CoV-2 in a large sample of commercially insured adults in the US. Design, setting, and participants Deidentified data were collected from the IBM/Watson MarketScan Commercial Claims and Encounters (CCAE ...
Objectives To determine the strength and nature of the association between delirium and incident dementia in a population of older adult patients without dementia at baseline. Design Retrospective cohort study using large scale hospital administrative data. Setting Public and private hospitals in New South Wales, Australia between July 2001 and March 2020. Participants Data were extracted for ...
Abstract. In a cohort study, a group of subjects (the cohort) is followed for a period of time; assessments are conducted at baseline, during follow-up, and at the end of follow-up. Cohort studies are, therefore, empirical, longitudinal studies based on data obtained from a sample; they are also observational and (usually) naturalistic.
Design: Nationally representative prospective cohort study. Setting: United States (U.S.). Participants: Data come from the National Longitudinal Study of Adolescent to Adult Health, a national cohort of adolescents in grades 7-12 in U.S. in 1994 followed for 25 years over five interview waves.
The observational design is subdivided into descriptive, including cross-sectional, case report or case series, and correlational, and analytic which includes cross-section, case-control, and cohort studies. Each research design has its uses and points of strength and limitations. The aim of this article to provide a simplified approach for the ...
2.1 Study design. This cohort, with a mixed method descriptive analysis, is an ancillary study of the FASSETS program (Favoriser l'Accés à la Santé SExuelle des Travailleuses du Sexe). ... In line with the principles of community-based participatory research, this study involved the creation of partnerships, regular exchanges between ...